Life Extension Magazine®
People today are aware of the importance of maintaining optimal blood levels of vitamin D for their overall health and well being. What many people do not know is that vitamin D is also indispensable to the health, beauty, and longevity of the largest organ in the body: your skin. The problem is that while the body uses sunlight to make vitamin D, sun exposure itself accelerates skin aging. Over time, ultraviolet light damages the skin, leading to wrinkles, sun spots, and higher risk of skin cancer. In addition, much of the vitamin D produced in the skin is taken up and used by other systems of the body. In this article, you will discover the critical role vitamin D plays in skin cell development and repair, as well as how it mobilizes your skin’s immune system and helps destroy free radicals that can cause premature aging. You will also learn how topical vitamin D lotion can deliver benefits directly to your skin, preserving its softness, health, and youthful appearance. Shedding Light on Vitamin D’s True IdentityTechnically, vitamin D doesn’t fit the classic definition of a vitamin at all. A vitamin is a substance that is crucial to normal everyday life function, but can’t be synthesized in sufficient quantities by an organism, and thus must be obtained from the diet.1 Your skin has the ability to manufacture as much as 10,000 IU of vitamin D after 20–30 minutes of summer sun exposure.2 But there are many limiting factors to internal vitamin D synthesis that include age, skin color, geographic latitude, seasonal variation in sunlight availability, and the widespread (but necessary) use of sunscreen, which all make it difficult for your body to produce the vitamin D it needs for optimal health through sun exposure alone. Too much sun damages the skin, creating wrinkles and fine lines, while increasing skin cancer risk. Still, your skin’s ability to synthesize a portion of its daily requirement directly from sunlight3 makes vitamin D unique among all other nutrients. Functionally speaking, vitamin D more closely resembles a hormone than a vitamin.4,5 Hormones are chemical messengers produced by certain glands and cells in your body that bind to specific receptors in order to produce a targeted biological response. The active form of vitamin D, calcitriol, is one of the most powerful hormones in the human body, endowed with the ability to activate over 2,000 genes (roughly 10% of the human genome).2 In order to become calcitriol, however, vitamin D must first undergo a complex series of biochemical reactions that begin in your epidermis, the outermost layer of your skin and the key to its youthful appearance. (See page 2 "Sunlight, Heat, and Skin: The Intricate Process of Vitamin D Production")
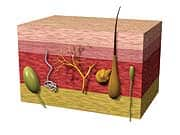
The Key Nutrient for Skin Cell Growth and ReplacementBeing fat-soluble, vitamin D as calcitriol easily crosses the phospholipid membranes of your cells and migrates to the nucleus. Here it binds with vitamin D receptors,6 a special group of proteins that sense the presence of steroid hormones. This linking regulates the expression of genes that turn different cell functions on or off.7,8 Vitamin D receptors are directly involved in cell proliferation and differentiation, as well as optimal immune function. These issues are vitally important to your skin, which not only serves as your first line of defense against pathological invaders, but must also replace approximately 30-40,000 lost cells a minute.9 This constant loss of cells on your skin’s surface must be offset naturally by an ongoing vitamin D- dependent renewal process that takes place in specialized cells called keratinocytes. Keratinocytes account for about 95% of all cells in your epidermis.10 They possess two properties which make them extremely valuable—the ability to actively divide, and the ability to differentiate. They are continuously providing new cells for replenishment of your skin’s surface. Cell activity in this layer is responsible for the creation of an underlying structural framework for your skin to reinforce the delicate matrix of skin tissue. This helps your epidermis form a watertight barrier that locks in moisture and keeps your skin soft and supple. This is where vitamin D comes in: rates of cell division and differentiation are triggered by growth factors and other molecules that are controlled by the presence of vitamin D.11-13 If adequate amounts of vitamin D are not available, your epidermal cells won’t differentiate optimally. As a result, the outer layer of your skin may become thinner and more fragile. It begins to sag from lack of adequate support. Dryness and wrinkles set in as moisture is gradually lost to the outside.14 This is one of the main reasons why vitamin D is absolutely essential to the maintenance of healthy-looking skin.
| ||||