LIFE EXTENSION MAGAZINE
Introduction by William Faloon
These articles are written for those who have, or suspect they have prostate cancer.
They are authored by Dr. Stephen Strum, a medical oncologist with extensive expertise and clinical experience.
These articles provide meticulous details about diagnostics and treatment options that are not widely practiced. They are not meant for casual reading.
They require intensive focus for those seeking better diagnostics and prostate cancer treatments.
To appreciate the content, I suggest at least two reads for those who have, or suspect they have a prostate malignancy. The purpose is to empower you with comprehensive data about current diagnostic and treatment options.
Part 1: Optimized Prostate Cancer Treatment
Introduction
I have been challenged by William Faloon, co-founder of Life Extension®, to share with you what I believe to be the best way to treat prostate cancer (PC).
What follows are my "Take Home Lessons" presented to you, the current patient or the future patient with PC. These notions span 60 years of work in the arena of cancer and immunology, and given the importance of the concepts presented, I believe you will agree that they should be invoked in contexts involving any form of cancer, and in fact any serious illness.
This task given to me was daunting, and in response I have investigated 570 peer-reviewed papers over the course of many months. I can assure you, the reader, and Mr. Faloon, that this is an honest appraisal.
I have selected almost 300 key articles and created a public Dropbox™ for those of you wishing to delve deeply into this vital topic and related issues. The link below will enable you to download close to 300 PDFs and graphic files into a zip file on your computer. You can unzip this to open and see all the files sorted alphabetically by lead author and by year of publication and title. https://bit.ly/bestwaytotreatPC
The Decline in Real Medicine
Degradation in the Patient-Physician relationship
Over the past 20 years, I have seen a gradual but persistent degradation in the communication between physician and patient.
This is the only relationship in life I know of where there is an opportunity to share with another person their history, their fears, their deepest concerns. It is a sacred relationship. How tragic that for many "physicians" it has been turned into a business transaction.
Medical professionals today often hide behind a computer, focus more on ordering tests than talking to the patient, give patients insufficient time to ask pertinent questions, and often relegate their responsibilities to other lesser-trained members in their office.
The patient feels like a commodity rather than a person facing a critical crossroad in their life. This has too often been my own experience when I, a seasoned internist and hematologist/oncologist have faced serious issues with my health. Clearly, we need to remember that talking to patients remains essential in the care of the patient.
The Therapeutic Index Forgotten
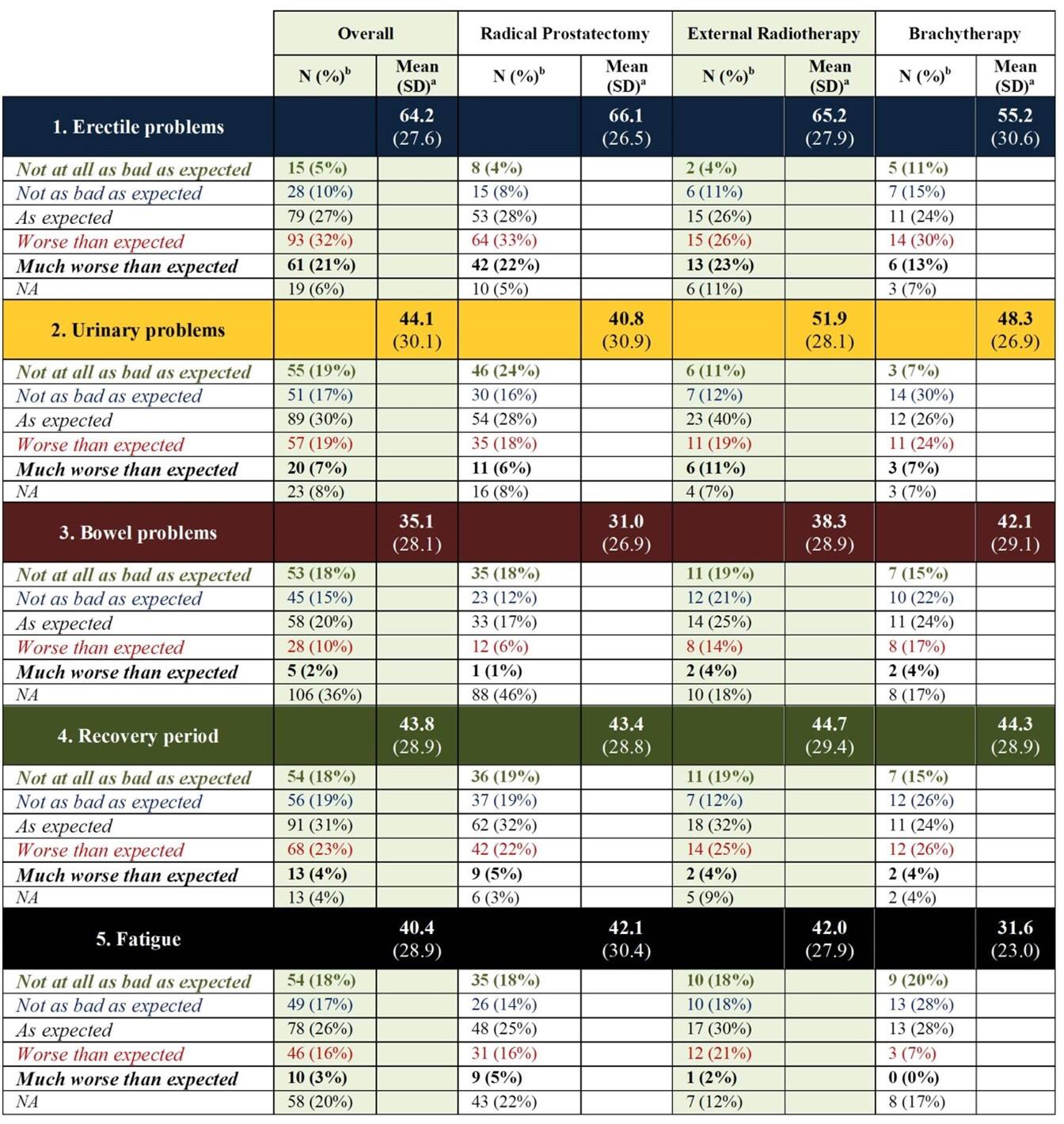
The therapeutic index (TI) is considered the Holy Grail of medicine. Do as much good to the patient as possible and do as little or no harm. Such a simple concept but one so often forgotten or ignored. When it comes to prostate cancer (PC), the most common malignancy affecting males, there are far too many unmet expectations that befall the newly diagnosed man with PC because physicians have forgotten the TI.
In 2020, this was pointed out in a medical article by Wollersheim, et al.1
A table provided at the end of this article details these unmet expectations by showing "worse than expected" and "much worse than expected" outcomes in response to the three most common prostate cancer treatments: RP (radical prostatectomy), EBRT (external beam RT) and BT (brachytherapy).
These 2020 data emphasized the need to look for ways to treat men with PC with less collateral damage relating to erectile and urinary functional outcomes while maintaining or improving oncologic (cancer) outcome. This should be a major priority in care of the man diagnosed with PC because quality of life (QoL) is at stake. This principle is applicable to all illnesses and their treatment.
The use of focal therapy (FT) intends to enhance QoL by lessening or eliminating collateral damage. At the same time, the oncologic or anti-tumor outcome is maintained. This last concept is the main motivation for that which will be described in the second article published on this web page.
What is the Foundation for Optimal Communication and Adherence to the Therapeutic Index?
First, we need to understand key factors that are at the crux of the best way to treat prostate cancer (PC), any cancer, or any serious illness.
The Critical Nature of Context
A 75-year-old man sits across from me. Because the patient has significant Alzheimer's disease, his daughter is by his side; she wants my advice on how to prolong her father's life. His medical records, which are quite voluminous, have been reviewed by me. In summary, he was seen at a major cancer center with a history of having been diagnosed with PC at age 75.
His prostate-specific antigen (PSA) was 85 ng/ml at the time of his diagnosis. The Gleason score, reflecting the aggressiveness of the PC based on pathologic findings was (4,4), indicating an aggressive biological behavior. This man's prostate cancer represents high-risk PC, with little likelihood that the cancer is confined to the prostate gland, but instead has spread systemically.
The digital rectal examination (DRE) revealed a prostate of about 40 cc with multiple hard nodules in the right lobe and a significant probability of EPE (extra-prostatic extension). His bone scan and CT of the abdomen and pelvis did not reveal metastatic disease.
He was advised to have a radical prostatectomy (RP), and this was done by the head of the urology department at the well-known cancer center. Three months after the RP, a repeat PSA was 45 ng/ml. This "residual" PSA reflected persistent PC that had not been removed by the RP. It was confirmed with repeat testing that showed a serial increase in PSA to 55 and then to 65 at one and two months, respectively, post-RP.
The patient was referred to radiation oncology and received radiation therapy (RT) over the course of six weeks to the prostate bed and regional lymph nodes. One month after completion of the radiation, the PSA was back up to 85 ng/ml.
This was the context of this patient when I saw him in consultation. His physical examination, including a digital rectal exam (DRE), did not reveal any findings of residual PC, and there was no enlargement of any lymph node accessible to a thorough physical examination.
The patient was demented. He had overt short-term memory loss and was not oriented to time or location. The medication (Aricept®) he was taking for his Alzheimer's disease had already been shown in studies to afford no significant improvement, and at most it might stabilize the disease for a few months. This patient's Alzheimer's disease was moderate to advanced; his daughter stated that he was combative and had struck his wife on multiple occasions.
I advised the daughter that my major concern was her mother's safety. Her father could not be managed at home with the risk of harming his wife. I did not hold back in telling the daughter that her father's PC care was inappropriate, and that from the start this was a man with advanced non-localized PC with no chance of cure with any form of conventional treatment, be it surgery (RP), radiation (RT) or other available local treatment (e.g., cryosurgery, laser ablation, high-intensity focused ultrasound).
I informed the daughter, as well as the patient's wife, that in the context of systemic disease the only reasonable approach would be androgen deprivation therapy (ADT). And I speculated that the significant lowering of testosterone might have a chance in diminishing the patient's combative behavior while keeping the PC in control. Context is so important in how we physicians advise our patients and their families. For that matter, context is vital in all aspects of life's matters.
I shall be telling this with a sigh
Somewhere ages and ages hence:
Two roads diverged in a wood, and I—
I took the one less traveled by,
And that has made all the difference.
—Robert Frost
Context should lead us down the right road so that our journey is not one of countless potholes and pitfalls along the way. Context is the setting, the environment; and in medicine it involves the most important of concepts: status (i.e., the patient's biologic reality).
Over and over, I have and continue to advise patients to assess their status, because failure to do so will lead you down the wrong road. An accurate assessment of status begets a strategy that optimizes the likelihood of a successful outcome. In all of biology, and for certain in the biology of health and disease, we must remember to focus on the individual's unique contextual menu.
The Contextual Menu
In the case above, the key points in this man's contextual menu included: age, mental status, PSA and Gleason score. There was a one in 10,000 chance for this man, with a PSA of 85 and a Gleason score of (4,4), to have OCD (organ-confined disease). He had systemic disease until proven otherwise.
In the early 1990s we did not have the more accurate staging tools, such as prostate specific membrane antigen (PSMA) PET/CT, and today, in 2022, we still do not have whole-body MRI (wb-MRI) in 99% of medical facilities in the U.S. wb-MRI is a 20-minute test costing $350 that has been used in Europe for many years.2-4
The above case is an example of the mistreatment that occurs when the patient's context is ignored, and when important tools such as nomograms, neural nets, machine learning and artificial intelligence, which generate probabilities of OCD (organ-confined disease) vs. regional vs. distant metastatic disease are not routinely part of the patient's assessment of status.
In contrast, when the detective work involved in determining the extent of disease is performed, a world of difference in predicting outcome occurs. Not only is the treatment likely to be successful, and healthcare costs diminished, but also the adverse effects of unnecessary treatment are avoided. This is the desired trifecta. This is akin to an engine fine-tuned for optimal performance; this is the therapeutic index as our modus operandi, or operating system.
The Physician as Artist vs. the Physician as Schmearer
As a young lad working in my father's gas station, the mechanic (Artie) watched me paint a wooden block. He asked: "Stevie, do you want to be an artist or a schmearer? I replied: "What's a schmearer?" A schmearer is someone that does not know how to properly hold a paint brush, gets pain all over himself and not the object he is painting, and fails to enhance the beauty of what he is painting. Be an artist, Stevie." I remembered those words 10 years later when a close friend (Bob) and I were making money during summer vacation painting homes. At the end of one job, the customer remarked: "If I need my house repainted, I will ask you, but please leave your friend at home." Bob, indeed, was a schmearer.
Having an outstanding MD (medical detective) intimately involved with a patient faced with a dire illness is another foundational requisite to achieve superior results. Such is the case of DM, diagnosed with PC at age 58, and presenting with a PSA of 7.3, a clinical stage of T2a assessed with a digital rectal exam (DRE) showing one lobe of his prostate gland with ≤ 50% tumor involvement), and a Gleason score of 4,4.
Stage T2 is when the tumor appears to be confined to the prostate. Due to the size of the tumor, the doctor can feel it during a digital rectal exam (DRE). The cancer may also be seen with imaging. A staging of T2a reflects a tumor has invaded one-half (or less) of one side of the prostate gland.
Validation of Critical Data
The Gleason score (GS) is rendered by a pathologist and relates the aggressiveness of the PC. Validation of the GS and ensuring that the result has been confirmed by an expert in PC pathology is most often not done. Validation of critical data is another foundational concept.
There are not many experts in PC pathology in the U.S. and it is hoped that artificial intelligence (AI) or machine learning (ML) will be shown to be of high accuracy so that we can avoid the pitfall of underestimating the GS. In my former clinical practice, expert review of the pathology resulted in a change to a higher GS (meaning more aggressive prostate cancer) in almost 80% of patients.
DM's PSA density (prostate specific antigen density or PSAD) was 0.20 based on a transrectal ultrasound (TRUS) gland volume of 36 cubic centimeters (cc). A multi-parametric MRI (mp-MRI) was performed and indicated that the Prostate Imaging Reporting and Data System (PI-RADS) score was 4 (intermediate to high aggressive PC likely).
DM was seen at a major center for PC, and the consultation concluded that a RP (radical prostatectomy) was indicated. This decision unfortunately neglected any calculation of his risk for EPE (extra-prostatic extension), SVI (seminal vesicle invasion) or LNI (lymph node involvement).
Multiple calculators, however, performed shortly thereafter, showed a risk of 22%-39% for lymph node involvement. DM did have an 18F NaF PET/CT (sodium fluoride positron emission tomography), which was negative for bone metastases, but no imaging study with reported high accuracy had been done to assess his lymph node status. The question of whether DM had node metastases and where they were had not been part of his assessment of status.
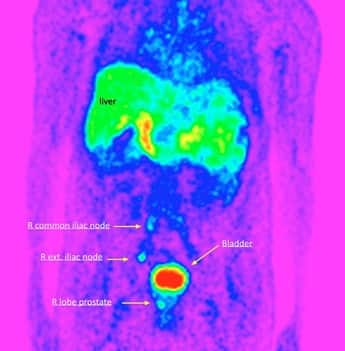
The patient consulted with me on 3/21/18. Given the findings of the various risk calculators that included nomograms and artificial neural nets (ANNs) (see http://www.prostatecalculator.org), I strongly recommended the patient defer prostatectomy and have a 68Ga-PSMA-11 PET/CT to exclude nodal metastases. That study showed metastatic disease in the right external iliac nodes, a right common iliac node and in one aortocaval bifurcation node.
A radiation oncology consultation was obtained at UCLA. A consensus opinion led to the patient being first treated with abiraterone (Zytiga®), leuprolide (Lupron®) and dutasteride (Avodart®) on 4/11/18. The purpose of this androgen deprivation therapy (ADT) was to reduce the tumor volume (burden) to enhance the probability of a complete and durable remission when RT commenced. Basically, the smaller the tumor target to be eradicated by RT, the higher the likelihood that a complete response will occur.
In six months, the patient attained an undetectable PSA (then defined as < 0.05 ng/ml), indicating sensitivity of the tumor cell population to androgen deprivation. On 3/18/19, the PSA had dropped further from 0.03 to < 0.006. A second mp-MRI performed on 7/12/19 showed that all prior tumor activity had disappeared.
Note that the PET portion of the PET/CT shows if there is functional uptake of the imaging isotope (Gallium-68) by attraction to PSMA (prostate specific membrane antigen) on the tumor cells. In reality, the isotope attachment to PSMA is more complex and involves a chelator, linker, and pharmacophore that binds to active recognition sites (ARS) of the PSMA molecule.
DM also had a repeat 68Ga-PSMA-11 PET/CT study which showed that all isotope uptake had disappeared after ADT. The CT portion of the PET/CT provides information about the size or anatomy of the tumor(s), and this second examination showed no nodes that looked suspicious for PC based on size (anatomical) criteria.
Radiation therapy commenced on 7/23/19 and was completed by 9/24/19. The patient received IMRT (intensity modulated radiation therapy) to a dose of 45 Gy to the prostate and 45 Gy to pelvic lymph nodes, with a boost to 60-62 Gy to grossly positive nodes. The patient had problems with nocturia x 6, likely due to radiation-induced inflammation.
Lupron® was stopped on 10/3/19. Inflammation biomarkers such as neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) were grossly abnormal with values of 15.5 (normal < 3) and 765 (nl < 192), respectively. By 1/22/20, urinary symptoms were almost gone. The patient did have fatigue and muscle loss and minor rectal leakage.
As of this writing, the patient is now almost three years since the completion of RT. The PSA levels have fluctuated up and down in the range of 0.124 ng/ml to 0.360 ng/ml, but no serial increase has occurred. It is possible that inflammation-related radiation prostatitis is causing the PSA fluctuations. DM has been informed to follow up with repeat markers and to consider measures to reduce inflammation if found to be present.
There is a world of difference between these two cases, but both have in common the critical issue of the value of context, how a patient is advised, an assessment of status prior to treatment, and how status was monitored. The physician and the patient should be aware of the patient's status if a successful strategy is to be used. If this is not done, then achieving an optimal outcome is highly unlikely.
Yogi Berra Hits a Home Run
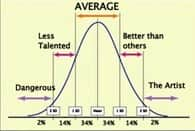
Yogi was a baseball star on the NY Yankee team. He was outstanding but his fame seems to live on for one of Yogi's typical quotes: "It's déjà vu all over again." And so, I keep coming back to one concept that seems to dominate in importance. Find the Artist. In my own struggle with a recent diagnosis of a B-cell malignancy called light-chain amyloidosis, I was not faithful to my own teaching; and it almost cost me my life but definitely has led to a serious decline in my quality of life. My only excuse is perhaps the shock of having a rare malignancy, and also being admonished by colleagues not to be my own doctor. Yet, this is the harsh reality of life, and given the consequences of health gone awry, nowhere else is finding the artist tantamount to either remaining alive and free of disease or succumbing to it. The quality of all human services is simply a bell-shaped curve and finding those who fit the criteria of an artist is daunting, but possible. Like the words of Robert Frost: "And that has made all the difference."
An artist in medicine cares about patient outcomes. He or she cares about minimizing toxicities and achieving the highest Therapeutic Index: the ratio of Benefits to the Patient ÷ Adverse Effects.
The artist associates with other artists, learns from colleagues, from patients and is voracious in reading the peer-reviewed literature to seek out the best of everything for those under his medical care or aegis. The word "aegis" is appropriate since it connotes protection; it is a virtual shield the physician-artist invokes to protect his patients from a spectrum of potholes that range from incompetent physicians to treatments where the therapeutic index is so low that any benefit is surpassed by adverse effects.
The artist is the ultimate ombudsman for the patient. Such healthcare practitioners are scattered over the country and the world. But they should be sought out and found, because the human body and psyche can handle just so many insults.
In almost 60 years of cancer medicine, I feel the strongest about this advice and yet it is given minimal attention.
Exactly 20 years ago, this prime principle was the subject of an editorial I wrote entitled "Strategy of Success in the Treatment of Prostate Cancer." The article starts off with a case history of GB, age 69, who was diagnosed with PC in August of 1999. The patient, a Canadian from Vancouver, sought out my consultation in Marina del Rey, California. He had bulky PC with a flagrantly abnormal DRE (clinical stage T2c or possibly T3b), a Gleason score read by the PC pathology expert David Bostwick that was (3,4) with a 20% grade 4 component. This was high-risk PC using the D'Amico risk calculator. https://www.thecalculator.co/health/d%E2%80%99Amico-Prostate-Cancer-Risk-Calculator-715.html
GB's local radiation oncologist wanted to immediately start RT. I objected and discussed with the Canadian oncologist why there was a major need to first reduce the tumor burden with ADT to allow the best chance of cure with RT (as done with patient DM). In other words, there was just too much cancer volume for RT to eradicate all the tumor, especially at the center of the tumor where radiation-resistant hypoxic cells exist.
ADT could achieve tumor reduction to facilitate the efficacy of RT. With ADT, the PSA dropped to undetectable levels. And with the drop in PSA (reflecting a decrease in tumor volume) the DRE gradually improved, and over months became normal. Then, with that goal accomplished, the patient was advised to initiate RT. GB is alive at 92-years of age and cured of PC. GB sought out the artist, who happened to be me, followed my guidance, and has lived 23 years without complications from the disease or treatment.
Where the Patient with Cancer Goes Wrong Time After Time
The article on Strategy of Success in the Treatment of Prostate Cancer starts with this sentence, which tells the tale of the wrong road taken by so many cancer patients.
After a diagnosis of prostate cancer has been made and the initial shock of a life-threatening diagnosis has begun to lessen, the thoughts of the patient almost invariably focus on "What should I do to get rid of this disease?" Family and friends reinforce this mental set as well as add to the anxiety of the situation by asking, "What are you going to do?"
And the pitfall described above is one that almost everyone falls into: the focus on what treatment to select, instead of gathering information to objectively understand the status of the patient.
When joined with the other naïve assumption that all physicians are equal in expertise, this pitfall creates the perfect storm for a less than optimal outcome.
A better first response after being told of a diagnosis of PC, or any other cancer, should be:
"Where is the disease and how much tumor there is, and what other issues in my health might be relevant to the strategy selected (e.g., lower urinary tract symptoms, potency issues, co-morbid conditions affecting blood supply and tissue repair such as diabetes). Will the status of my cardiac, kidney, pulmonary mental health, or any other issue unique to my biology have relevance to the treatment options presented to me?
All of us are subject to this frequently traveled rocky "road." I came close to dying from an overly zealous medical oncologist who did not take into account my contextual menu. I was also at fault in selecting this oncologist because he was more convenient insofar as his geographic location. I learned, too late, that those with my illness (light chain amyloidosis) were highly sensitive to the toxicity of chemotherapy. Only one cycle of chemotherapy has left me with chronic edema of my lower extremities that necessitates diuretic drugs, and in turn those drugs have wrecked my life by causing excruciating painful muscle spasms in my lower extremities that have left me afraid to sleep. And that, dear readers, is why I am editing this article at 2:23 AM. Get educated about your illness, or risk paying the consequences for your ignorance.
I "wised-up" quickly and sought out the artist and was guided by that artist and by other highly talented physicians in areas that needed fixing. I practiced what I had been preaching for decades, but only after a close encounter with death. I think Shakespeare got it wrong with "frailty, thy name is woman." Perhaps "frailty, thy name is human" would be far more accurate.
I need to restate that I was asked to write this article by William Faloon to bring to the forefront the most exciting and effective way to treat PC. However, what so many tend to forget is that a treatment is not an entity unto itself—it must be coupled with patient context, and it must be applied in that context by an artist or at the very least, a highly talented physician. Such a physician considers his or her prime directive the patient's outcome, and not the physician's income.
Yes, there are treatments that I have found to be highly effective and patient-friendly in the goal to cure PC, but they only accomplish this goal under proper conditions: the appropriate patient context and the delivery of that treatment by healthcare practitioners of special talent. Before sharing my thoughts on the best way to treat PC, another story will be informative.
In the early 80's, working in my office in Culver City, California, I was treating patients with a wide variety of malignancies. This included leukemias, lymphomas, cancers of the breast, lung, brain, pancreas, colon and virtually every adult form of malignancy. I was not specializing in any particular type of cancer.
One day, a patient brought in a newspaper clipping about a Canadian physician named Fernand Labrie who was seeking American collaborators to experimentally treat metastatic PC with a combination of two major hormonal manipulations. This involved suppressing luteinizing hormone (LH) that drives production of male hormone in the testicles, and a second drug in the anti-androgen class that blocked the AR (androgen receptor) to inactivate any residual male hormone (e.g., testosterone and dihydrotestosterone (DHT)). Labrie called this combination hormone blockade or CHB.
I was one of six physicians in the U.S. who collaborated with Labrie, and soon the word spread among the PC community of patients, and my office became a central point of such patients seeking this therapy. The results of CHB were dramatic, and it was common to see complete disappearance of bone metastases in men, the very same men, who had been told by their local physicians to go home and get their affairs in order.
What followed in the ensuing years was that men with all stages of PC came to see me in consultation. Some had no pathologic diagnosis of PC but did have a strong family history of PC. Others were newly diagnosed with PC and others had far advanced disease.
In the 1980s and to a great extent today, patients are rarely referred to a medical oncologist in the early stages of PC. I had to rapidly gain major expertise in this context if I were to optimally serve patients under my care.
The mainstay of treatment back then was RP (radical prostatectomy) and for the first few patients with apparently localized PC I referred patients to the local urologists. But in doing so, I soon learned a most painful lesson that has haunted me.
During a follow up visit of a patient who had undergone a RP, I performed a digital rectal examination (DRE) and while doing so noted urine dripping from the patient's penis. He was grossly incontinent as a result of the RP. I was quick to learn that all urologists are not equal in their talent, and I, ignorantly, had not selected an artist for my patient needing surgery.
With every patient who consulted with me in the months and years that followed, I noted who the urologist was and if the patient remained "dry" or instead had lasting incontinence. A clear picture of who the RP artists were emerged.
As a result, I only selected those highly talented urologists. I applied the same detective work for patients who came to me from every state and created a directory of artists (experts). I did the same for other areas involving special skills such as radiation therapy (RT), cryotherapy, HIFU (High Intensity Focused Ultrasound). I created analogous similar lists of medical oncologists, pathologists and radiologists evidencing expertise.
The vast majority of my patients thrived (i.e., they did very well, had high qualities of life and the overwhelming majority did not succumb to PC). Years later, when I became a full-time medical director of the PCRI (Prostate Cancer Research Institute), I posted these lists of experts on the PCRI website. Unfortunately, this list was not routinely updated and it has been removed from the PCRI website.
The bottom line in successful outcomes in healthcare continues to be ignored. Patients and most physicians still react to a diagnosis with "What should I do to get rid of this disease?"
We do not wish to face the harsh reality that the bell-shaped curve exists in all walks of life. But the value of this understanding becomes the clearest and most severe in the arena of human healthcare, affecting both quality and quantity of life. In an attempt to turn these elements of successful outcome into an equation, I have come up with this rudimentary equation—but it is a start. The equation attempts to embrace all crucial elements necessary for successful outcome.
S (successful outcome) = (Art+ EOD +PE + Emp) – C (co-morbidity total)
- Art is the artistry factor of the physicians involved, with a subpar MD having a score of 0, an average MD a score of 25, and a true artist a score of 80.
- EOD (extent of disease) is whether or not the patient has had refined staging techniques (score 30) to properly assess the extent of disease. If not done, no points are appointed.
- PE (path expert) relates to whether the pathology was reviewed by an expert (a point score of 30 is allotted if this has occurred).
- Emp is patient empowerment or how involved and committed the patient and family is in the understanding of his or her disease and committed to interacting with all physicians on the patient's team. Major PE gets a score of 20 points, while no PE is scored -20.
- C (co-morbidities) is the patient's context as defined by taking into account existing co-morbidities (subtract 10 points each for diabetes, heart disease, obesity, kidney disease, cognitive decline).
A patient with an average medical doctor (25), having refined staging (30), expert pathology review (30), major PE (20) and obesity and diabetes (-20 from total score), would have a total score of 85. But a patient with the same co-morbidities (-20), no refined staging (0), an expert pathology review (30), and a subpar MD (0) would have a score of 10. This is crude, but you get the gist of the equation. We cannot simply focus on choosing a treatment as if it were an item on a menu. In each patient's narrative, we need to know the rest of the story.
So now we come to the task I was assigned: What is the best way to treat prostate cancer that appears to be locally confined to the prostate gland. On the surface this sounds simple. Besides the crucial elements of success that have been detailed, there are mitigating factors for each and every treatment.
Caveats
Caveat 1. Curing PC with surgery, radiation, cryotherapy, HIFU, laser ablation involves destroying prostate tissue.
For RP (radical prostatectomy) this an immediate effect (i.e., the prostate is removed). For RT (radiation therapy), cryo, HIFU and laser ablation there may be a delayed effect where over months to years the prostate undergoes fibrotic (scarring) changes and eventually there may only be a nubbin of what was once the prostate gland.
The prostate gland has a role in the muscular aspects of orgasm and in the production of semen. The nature of ejaculation and the volume of the ejaculate often correlates with the intensity of orgasm and its quality. A man undergoing these procedures will not return to the normal sexual life he once had prior to any of these procedures.
Discussions of this nature between physician and patient are uncommon for the man newly diagnosed with PC. There is far more disclosure in a real estate transaction than in human health matters involving genitourinary functions.
Caveat 2. A diagnosis of any disease, including PC, is a warning flag that the integrative nature of health has been compromised.
Disease creeps up on us and the focus on prevention in healthcare is sorely lacking. We too often wait for a disease, treat it to make signs and symptoms go away, and neglect looking into the causative factors that tipped the balance of health toward disease. It is a rare occurrence, for example, to see the following addressed routinely when evaluating a man recently diagnosed with PC, or for that matter, any patient newly diagnosed with cancer or any serious illness:
- Vitamin D levels—measured in the serum as (25-OH)-D3, and with optimum levels in the 75 to 95 ng/ml range in my view. (Life Extension's optimal range for 25-hydroxyvitamin D (25-OH) is 50 to 80 ng/mL for most individuals.)
- Inflammation out of control—measured as homocysteine, high sensitivity C-reactive protein (hsCRP), neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), w-6/w-3 fatty acid levels and ratio, LA/DHA- a key fatty acid ratio in Western society where processed food high in the omega-6 fatty acid linoleic acid (LA) is ingested in dangerous quantities; AA/EPA—another fatty acid level looking at arachidonic acid (AA), a precursor in the eicosanoid pathway leading to pro-inflammatory PGE2 (prostaglandin E2). These are the readily available markers of inflammation, and there are others that can be ordered from Life Extension if indicated.
Test |
Optimal Range |
Reference Range |
|---|---|---|
Homocysteine (μmol/L) |
< 12 good < 8 ideal |
0.0-14.5 (18-60y) |
High sensitivity C-reactive protein (hsCRP) (mg/L) |
Women < 1.0 Men < 0.55 |
Low risk <1.0 Average 1.0-3.0 High >3.0 |
Omega 6 : Omega 3 ratio |
<4:1 |
|
AA:EPA ratio |
≤ 4.9:1 Good ≤ 1.7:1 Ideal |
|
Omega 3 index (%) |
8-12% |
2.90-12.90% |
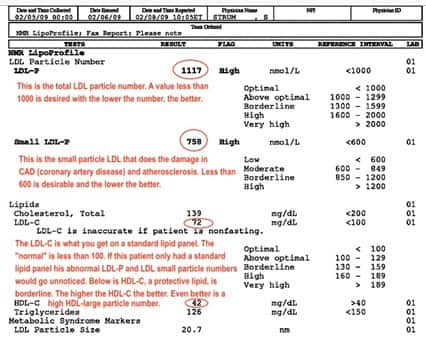
- Assessing lipid particle numbers with nuclear magnetic resonance (NMR) lipoprofile—this quantitates the disease promoting LDL small particles and the health promoting HDL large particles. This test, done by LabCorp, is extremely useful to monitor those not only at risk for cardiovascular disease but also with the realization that lipids are used as fuel by most cancers. An example of a normal LDL-C level but with a high LDL small particle number and high LDL total particle number and suboptimal HDL-C is shown below.
- Investigating bone integrity insofar as bone density and to determine if there is active bone resorption—overly active bone resorption (breakdown) is associated with release of bone-derived growth factors that stimulate cancer growth and spread. Bone resorption is measured by DpD (deoxypyridinoline), a collagen end-product that is released into the urine as bone is broken down.
Such a patient, over time, becomes osteopenic at first and then osteoporotic. The current "gold" standard for measuring bone mineral density (BMD) is the DXA (aka DEXA) radiology study. But it is often an underestimate of the patient's actual bone density since degenerative joint disease (DJD), osteoarthritis (OA) and/or vascular calcifications are mistakenly interpreted by DXA as bone density. Therefore, the DXA misinforms the physician and patient and results in a falsely high bone density. The better test is quantitative computerized tomography (QCT), but this imaging procedure has been edged out by the tech company and physicians who see an easy profit in doing DXA in the MD's office, whereas QCT is usually done in the out-patient department of a hospital. The QCT is often done as part of a total ultra-fast body CT scan.
The above is an introduction indicating some of the measures involved with Caveat 2. But those are vital to the successful outcome of a patient having a significant illness, and to the resolution of the same factors that led to the first occurrence of the major illness. We don't want deju vu all over again. This caveat, in my opinion, is a crucial part of what the strategy of active surveillance (AS) for low-risk PC should include, and this is why I have preferred active objectified surveillance (AOS) rather than simply AS. This will be discussed further later on.
Caveat 3. Let the Buyer Beware.
Be aware (beware) of the physician whose prime directive is physician income >> patient outcome. All highly skilled people are entitled to profit in their occupation, but not at the expense of patient life and well-being. How much time is spent by the MD with you? Are you examined thoroughly at intervals in your care? When your physician examines your lungs does he listen with his stethoscope through your shirt or blouse? If so, that is the sign of superficiality. When your lower extremities are assessed for any edema (ankle swelling), are your socks removed? If not, it is another indicator of "fast-food" medicine, and the doctor is not an artist, but a schmearer. Most patients can sense if their physician is working predominantly for them. Sadly, today, most physicians regard themselves as employees and the patient is a buyer. So, remember caveat emptor, i.e., "let the buyer beware." We docs once had a profession (a calling), but that is becoming extinct.
"One of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient."
—Sir Francis Weld Peabody to Harvard medical students in 1917
Caveat 4. Primum Non Nocere.
During my early years in hematology and oncology, I was frequently asked to consult on patients where the primary medical problem was "iatrogenic." This word means physician induced. In all medical schools the maxim primum non nocere is emphasized. I recall seeing this on the wall of a building at my medical school, the University of Chicago. It means "First, Do No Harm."
Decades later, I have realized this most importantly applies to the bell-shaped curve, and that a significant number of those having an MD after their name pose a danger to patients.
During my internship, I and many other interns would not allow one particular intern see our patients (do coverage) because of the high number of patients who died or developed serious complications under his watch. My profession was, and remains, overtly derelict in not correcting or removing such dangerous physicians from public care. Physicians should be objectively rated as to how well their patients do, but this will not happen in my lifetime.
Primum non nocere is very relevant to the realm of prostate cancer. The therapies that totally ablate the prostate tissue leave a lot to be desired. In good hands and in the right context they do succeed in achieving high-level oncologic outcomes, but quality of life or functional outcomes are too often affected. For my illness, I have learned the impact of collateral damage. I went from being able to shovel my complete driveway three times in one week to being barely able to walk to my next-door neighbor's house.
For prostate cancer, we can treat men with apparently circumspect (gland localized) disease with focal therapies such as focal cryo, focal laser ablation, focal HIFU (High Intensity Focused Ultrasound), vascular-targeted photodynamic therapy (VTP) or other less than whole-gland approaches. Those therapies can allow the patient to have his cake and eat it too—perhaps.
But remember, in our equation for success, there is the need to identify an artist and there is also the prerequisite of accurate staging and appropriate context. Without accurate staging we may be using focal therapy to treat a patient who has widespread disease.
In cases where more extensive disease is inaccurately assessed, PSA levels rise in a serial fashion after treatment, an inadequate nadir in the biomarker PSA is seen, short PSADT (PSA doubling time) or higher PSAV (prostate specific antigen velocity) calculations occur. These biologic markers or biomarkers are "telltales" that a problem exists.5-8 The same is true if abnormal findings are discerned upon repeating a multi-parametric MRI (mp-MRI) with targeted biopsies after focal therapy, or in those followed by active surveillance (AS).9-11 But underestimating the stage of PC could possibly have unfortunate consequences involving mutations in the tumor cell population that may confer more resistant disease. That question remains unanswered.
As to consulting with an artist, how do you, the patient, know who is an artist? Your chance of finding an artist is enhanced if you are under the care of a physician who will investigate other doctors and ascertain the likelihood that they are experts or artists.
You, as an empowered patient, should be active in support groups in real time and online. This could lead you to identify other patients who have undergone treatment with outstanding results and who have physicians that fit the definition of an artist. And if you consult with a physician and are uncertain if he or she is an artist, you can ask him for the names and contact information of three patients he or she has successfully treated in the last year. But otherwise, this is a crapshoot. You have no idea who is really outstanding, who is mediocre, and who is dangerous.
Patients' evaluation of pre-treatment expectations and post-treatment experiences of side effects following active treatment of prostate cancer. Modification of Table S1 (supplementary material) from Wollersheim BM, van Stam MA, Bosch R, et al. Unmet expectations in prostate cancer patients and their association with decision regret. J Cancer Surviv. 2020;14(5):731-738.
Part 2: Focal Therapy
Focal therapy (FT) means directing a particular form of energy to the major lesion (called the index lesion) of an organ or tissue, while leaving the rest of the organ or tissue intact. This is done to preserve as much normal function as possible while achieving good oncologic outcomes. The goal with focal therapy is to reduce side effects and improve recovery times compared with radical treatment options. In an investigational setting, FT is used to damage tumor cells (instead of removing/destroying the primary cancer), and triggering a systemic immune response against any local, regional or metastatic cells.
Currently available FT options are:
- Focal Cryotherapy
- Focal HIFU (high intensity focused ultrasound)
- Focal Laser Ablation (FLA)
- Irreversible Electroporation (IRE)
- Vascular-Targeted Photodynamic Therapy (VTP)
- Focal Cryo-Immune Therapy (investigational)
- Radiofrequency ablation (RFA)
- HDR-brachytherapy (high-dose rate brachytherapy)
- Focal brachytherapy (FB) using seeds
The goal of all forms of FT is to be as selective as possible in targeting malignant tissue that has lethal potential while sparing normal tissue that is crucial to the normal function of the individual and thus their quality of life.
That said, all focal therapies involve energy sources that are ablative or destructive, with an emphasis on some irreversibly destroying cells while others inflict a range from sub-lethal to lethal damage.
Sub-lethal tumor cell kill may be of paramount importance insofar as allowing for immune destruction of distant sites of metastases; this is purported to be the case for radiation therapy, focal cryotherapy and VTP, when these focal therapies are combined with immune checkpoint inhibitors (like Keytruda®, Yervoy® and Opdivo®) ± granulocyte-macrophage colony stimulating factor (GM-CSF).12-15 This is an exciting area that is investigational and undergoing clinical trials.
The release of tumor antigens and subsequent immune response was demonstrated in a paper published in 1967 in the journal Immunology, whereby cryoablation therapy alone studied in rabbits resulted in a rapid antibody response to cells damaged/destroyed via the freezing process.
In the best of worlds, we would prevent PC. In the second best of worlds, we would have some form of medical treatment that is easily administered, has negligible side effects and is not outrageously expensive. But this is not the reality of PC treatment anywhere in the world in 2022.
The current "gold standard" in treating localized PC involves surgically removing the entire prostate or delivering radiation therapy to the entire prostate. Despite the growing peer-reviewed literature on focal therapy, the overwhelming majority of men are still undergoing radical prostatectomy (RP) and radiation therapy (RT), and far fewer focal cryotherapy, focal laser ablation therapy or focal HIFU.
In the last 10 years, there are increasing peer-reviewed papers reporting the use of various focal therapies in men with intermediate-risk disease.
But realizing the importance of factors such as:
- accurate determination of extent of disease,
- accuracy of the Gleason score, and
- the expertise of the physician performing the focal therapy…
…the current dilemma the man with PC faces is much better understood.
It is important to remember the three major risk groups per D'Amico. These are low-risk, intermediate-risk and high-risk.
The risks are based on PSA, Gleason score and the clinical stage (based on DRE).
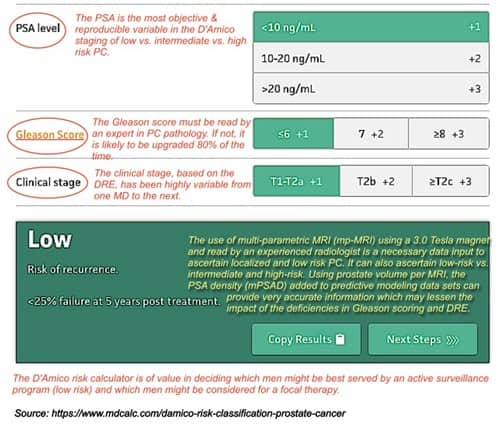
We can assign points to each variable to remember these risk categories. As shown in the graphic below, PSA levels are stratified as < 10 vs. 10-20, and vs. > (greater than) 20, with point scores of +1, +2 and +3, respectively.
The Gleason score categories are:
- ≤ (less than or equal to) 6 vs. 7 vs. 8 or greater, with points of +1, +2 and +3, respectively.
- The clinical stage categories are T1c to T2a vs. T2b, vs. T2c or greater, with points of +1, +2 and +3, respectively.
- The annotations in the graphic (red and yellow font) are my comments.
The lowest score (3-point total) is the low-risk PC category. Such patients are candidates for what is called active surveillance (AS).
The intermediate-risk score patients may be candidates for one of the focal therapies, the latter being a topic of much controversy. Some in the intermediate-risk classification having a Gleason score of 6 but either a PSA of 10-20 ng/ml or a clinical stage of T2b behave as low-risk patients and can be followed with an active surveillance protocol.
The crucial importance of any Gleason grade 4 disease (3,4), (4,3), (4,4) or higher is demonstrated.16
As to the gold standards of total gland removal (radical prostatectomy) or whole gland radiation (intensity modulated radiation therapy), the contemporary literature swings back and forth about which treatment is best, but the critical ingredients of success of either therapy: the expertise of the technician, in this case a urologist (surgeon) or a radiation oncologist (internist) is never analyzed.
And in 2022, with more papers being published each year on artificial intelligence (AI) and machine learning (ML), why are we not using those technologies to get a highly accurate determination on one key variable-- the Gleason score, because this is such a vital element relating to outcome.
We move far too slowly when it comes to human life, and the cost is great to everyone.
The so-called "war on cancer" that takes 20 years to bring a promising therapy to the patient is not the way to win a battle involving human life. Too many lives are lost along the way with this meandering road approach.
However, early access to promising therapies mandates obsessive follow-up of patient outcomes relating benefits and side effects with punitive damages to physicians and pharmaceutical companies that do not provide such post-approval data.
If we get real about the numbers of artists in cryosurgery, laser ablation, HIFU, and other focal therapies in the U.S., then it is not possible to get significant numbers of men with PC treated by someone with outstanding technical skill.
In my opinion, expertise in cryotherapy may be limited to as little as 10 artists in the U.S.
With HIFU, expertise in my experience was initially only to be found in Germany, but perhaps the situation has changed, and maybe there are artists in the U.S. I would assume that those considered artists in any field are limited by factors of experience and natural talent.
The same concerns would apply to focal laser ablation and to vascular-targeted photodynamic therapy (VTP). I know from my past experience that HDR-brachytherapy (high-dose rate brachytherapy), another form of focal therapy, was limited to less than 10 radiation oncologists in the U.S.
Comparing the "expertise" of physicians performing technical procedures is never done. In medicine, we do not have a scoring system that grades physician skill.
When cryotherapy was first started by Onik and Cohen in 1992, I emphasized the need for an accreditation process, but this issue was side-stepped by Cryomedical Sciences Inc. and never revisited. Physicians may be compensated equally for their services whether they be artists or duffers. Some have a minuscule talent and some exude talent.
As previously noted, in my initial state of ignorance I referred a patient to a local urologist who left the patient grossly incontinent. In subsequent cases when I referred patients over the ensuing years to those two or three locally identified artists, those patients never experienced incontinence of any significance, and often erectile potency was preserved.
Insofar as potency, the age of the man, how strong his erections are prior to the diagnosis of PC, and the ability to spare both neurovascular bundles are additional factors determining good erectile function after any ablative therapy, be it total ablation or focally ablative therapies. Note that in this editorial, additional forms of focal therapy: irreversible electroporation (IRE), vascular-targeted photodynamic therapy (VTP), focal brachytherapy, stereotactic ablative radiation therapy, and hemi-prostatectomy are not discussed. However, the same issues apply to all forms of focal therapy.
There have been advances in imaging with the advent of multi-parametric MRI (mp-MRI). And within the world of MRI there have been enhancements in magnet strength so that 3.0 Tesla magnets render superior imaging compared to 1.5 Tesla units. But again, the human element pervades every facet of care. The person interpreting your mp-MRI should be to the far right of the bell-shaped curve.
The only area of optimism I see to possibly bypass the issue of human expertise in arenas such as pathologic interpretation, MRI and other imaging interpretation is the use of artificial intelligence (AI), machine learning (ML) and predictive modeling (PM). This is emerging, but like everything in medicine, the time to routine human application of such advances too often takes 10 to 20 years, and sometimes longer.
So, in a best-case scenario, the empowered patient has networked with local-regional and/or national support groups and has discovered where the experts are. This again points to the value of collaboration, but in this case, it is between patients. Men do not collaborate as well as women.
There are other obstacles such as accessibility to the expert and perhaps the issue of insurance coverage. In my own battle with a rare malignant hematologic disease called light chain amyloidosis, I had initial problems with accessibility, and I am a hematologist/oncologist. Imagine what the ordinary lay citizen encounters?
AS or FT?
But there is another crossroad: how do you decide if the patient is better off with active surveillance (AS) or with focal therapy (FT)?
Because standard therapies such as radical prostatectomy (RP) or radiation therapy (RT) for low-risk PC equate with both overtreatment as well as adverse effects (e.g., incontinence and/or sexual function decline), active surveillance (AS) is a reasonable tactic to use in this patient context.
Active surveillance (AS) is described later in this article.
Again, the issue of status (i.e., the individual patient's findings) must be emphasized. The risk assessment designation of "low-risk" is determined by PSA, clinical stage per digital rectal exam (DRE) and Gleason score.
The Gleason score must be a (3,3) for the patient to be considered low-risk and therefore it is essential that an expert in PC pathology review the diagnostic biopsy to ensure this is not upgraded to (3,4), (4,3) or higher.
In a 2016 study involving the rate of metastasis in 980 men followed on an active surveillance protocol, Yamamoto, et al. found that only 3% (30 men) developed metastatic disease. Fourteen of those 30 men had intermediate-risk PC. What they found as independent risk factors for metastatic disease were:
- PSADT < 3yrs (Hazard Ratio or HR 3.7), i.e., PSA doubling time (PSADT) occurring in less than 3 years revealed a 3.7-fold increase in metastatic prostate cancer risk.
- Gleason score < 7 (HR 3.0), i.e., Gleason score over 3.0 revealed a 3-fold increase in metastatic prostate cancer risk.
- ≥ 3 positive cores (HR 2.7) i.e., needle biopsy yielding more than three malignant cores have a 2.7-fold increase in metastatic prostate cancer risk.
HR indicates hazard ratio, so a PSA doubling time (PSADT) of less than three years increased the risk of metastatic disease 3.7-fold17.
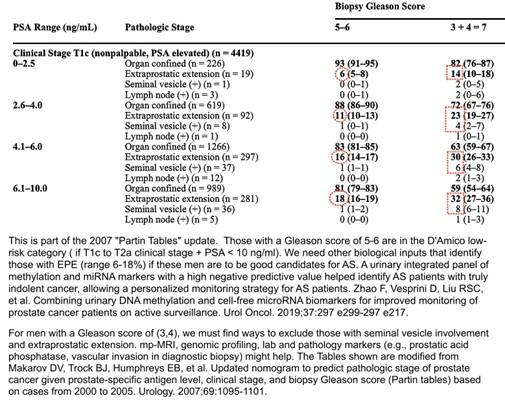
What we see with a study such as Yamamoto, et al. is the involvement of risk factors that are embedded in the patient's individual biology. This is what led me to the early use of the four tables from Johns Hopkins that correlated the patient's PSA, clinical stage and Gleason score with the findings of RP. I termed these the "Partin Tables" and found these nomograms to be highly consistent in individual patient outcomes.18
These tables have been updated in 2001 and 2007.19,20 The 2001 update emphasized the importance of distinguishing the Gleason score of (3,4) vs. (4,3). This confirms the landmark article by Stamey and McNeal that showed that the amount of prostate cancer with Gleason grade 4 or higher was the most critical determinant of PC progression.21
I strongly advise that that the amount of grade 4 be quantitated, and that the term "Gleason differential" would be an appropriate term to use. Note that Gleason (3,4) [% grade 4] applies to a (3,4) lesion and that the Gleason differential can range from as little as 5% to as high as 49%. This would seem likely to be a pathologic marker pertinent to explain which patients with intermediate-risk PC may behave as low-risk patients if the percentage of grade 4 disease is perhaps in the 5%-19% range. This becomes another critical factor in deciding if a man may be served best by active surveillance (AS) vs. focal therapy (FT) vs. whole-gland therapy. Also note that in this seminal paper by Stamey and McNeal, in addition to the amount of Gleason grade 4 or 5, that cancer volume and the presence of vascular invasion were additional significant factors in cancer progression of PC.21 The presence of vascular invasion has been shown to be an adverse pathologic finding with high prognostic importance, not only in PC, but also in Hodgkin's disease, breast cancer, renal cell carcinoma, head and neck cancer, gastric cancer, and other malignancies.
Stage T1c prostate cancer is usually early-stage disease detected with a PSA blood test. These patients have a nonpalpable digital rectal exam and are diagnosed by needle biopsy. When more patients were diagnosed early because of widespread PSA screening, the distribution of early-stage (T1c) shifted upwards. This "stage migration" was a result of the greater use of the biomarker PSA as detailed below.
The 2007 update analyzed 5,730 men between 2000 and 2005. With the increase in PSA testing 77% of patients presented with T1c disease, 76% had Gleason score 5-6, 80% had a PSA between 2.5 and 10.0 ng/ml and based on radical prostatectomy, 73% ended up having organ-confined disease.20
Such a change in the natural history of PC has a huge impact on the number of men who are candidates for AS and FT. The 2007 "Partin Tables" update did away with the Gleason scores of 2-4 since no PC pathologist was reporting 2-4. I would state that I have not seen a Gleason score of 5 in decades and in future updates, I am sure we will only see Gleason scores of 6 or higher.
The table below shows part of one of the four "Partin Tables" that is important in categorizing a patient as to candidacy for AS or FT (only PSA up to 10.0, Gleason score of 6 or (3,4) and clinical stage T1c).
Table 2, with the additional low-risk variable of clinical stage T2a, is not shown. Those numbers with red circles or red rectangles indicate pathologic risk factors that are more likely to translate into progressive disease when either AS or FT is the treatment selected.
Once again, this calls for the use of AI, ML or other tools such as additional nomograms or ANNs to sort out these "outliers." This is the approach I used in advising men on options for treatment.
One such additional nomogram by Nakanishi showed the discriminatory value of adverse findings such as older age, higher PSAD values, and greater tumor length.22 Others have shown the value of having a threshold of only two positive cores23,24 or less than 50% of cancer in any one core.23,25 It is striking that almost all of these "new" developments confirm the foundational importance of the Stamey and McNeal study of 1999 that emphasized Gleason grade 4, cancer volume and vascular invasion by PC.21
In my opinion, the Partin data and other nomograms should be used to define patient risk, as well as artificial neural nets (ANNs) such as one found at http://www.prostatecalculator.org. Vascular invasion in the diagnostic biopsy specimen should be ruled out. In my work in Hodgkin's disease, vascular invasion was a key risk factor for Hodgkin's disease spread to the spleen and to the liver.26 Others have found vascular invasion to be a key pathologic finding in breast cancer27-31 and other cancers, as noted earlier. The "truth" is out there; we just do not do the work to find it. This is the very nature of research.
In other words, what I believe happens in medicine, and in most of life, is that we try to simplify the biologic factors that define how we treat patients. In the arena of focal therapy this involves what patients need to be treated with whole-gland ablative therapy versus focal therapy (e.g., hemi-gland, sector or index lesion-based therapy) versus those who can be managed medically with what is being called active surveillance (AS).
Human nature attempts to pigeon-hole the individual's biology into categories rather than accept the unique biology that each of us expresses. Eventually, we will realize the fallacy in such "one-size fits all" thinking. Again, the value of artificial intelligence (AI) and machine learning (ML) combining multiple variables into an equation that best defines risk or lack of risk must be explored. There are recent publications that validate this use of combined variable analysis.32,33
Patients must not forget, and physicians must be reminded that the nature of humankind is to conserve energy and do less work. Yet we have the experiences of generations of human history that show the significance of the basic concept I casually term the "Duck principle."
"But when I see a bird that quacks like a duck, walks like a duck, has feathers and webbed feet and associates with ducks, I'm certainly going to assume that he is a duck."
—Emil Mazey Secretary-Treasurer UAW Labor leader 1946.
We need to learn to think before we act. What we are seeing in the world of medicine and elsewhere in life is a failure to understand critical thinking.
My grandmother from Poland, in her humorous misunderstanding of English aphorisms used to say, "Don't jump off the bridge until you come to it." Well, what too many of us do is "jump" prior to the necessary work that must be done to enhance a successful outcome. In the make-shift laboratory of my high school years, a plaque on the wall reminded me that "The only place were success comes before work is in the dictionary."
All of us must be master carpenters: measure twice and cut once. In the case of human lives, employ all the measures it takes to make the best decision. Always remember that MD stands for medical detective. Get the information, determine the patient's status accurately, find the people of special talent and discuss the possible strategies. This "road less traveled" will yield amazing dividends.
Active Surveillance Should be Active Objectified Surveillance (AOS)
With 40 years of field work involving thousands of PC patients, my contention is that AS is not what it should be. A man with PC, no matter what the risk category, developed this disease, so why not investigate possible factors which may be operative, and remove any impetus for the PC to continue to grow, mutate and spread. One such impetus is the condition of excessive inflammation. Inflammation can be analyzed by lab testing of omega-3 and omega-6 fatty acid levels.
Life Extension® has made this available via the Omega Index Complete. Previously mentioned were inflammation-related biomarkers such as homocysteine, high-sensitivity C-reactive protein (hsCRP), neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR)—simple mathematical derivatives from the CBC. All of these are readily accessible lab tests in the U.S.
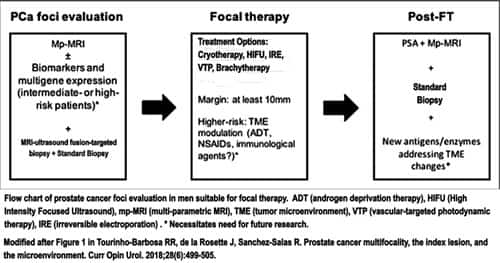
An excellent article by Tourinho-Barbosa from 2018 entitled "Prostate cancer multifocality, the index lsesion, and the microenvironment" provides key insights into the tumor microenvironment (TME), or what I call the patient's biological milieu. In 1889, Stephen Paget referred to this as "the seed and the soil" in his analysis of breast cancer patients34 A modified graphic from Tourinho-Barbosa shows how multiple factors, including the TME, play a role in managing those receiving focal therapy.35 The same principle can be applied to AS patients, or at an earlier stage to prevent the emergence of disease. This was reported in a recent paper showing how an agent like a standardized lipid extract of Serenoa repens can affect the typical age-related development of benign prostatic hyperplasia (BPH).36
Cancer cells also must have fuels to grow and flourish. The most important fuel for all cancer cells is glucose. In our country obesity has become the norm and not the exception, and abdominal obesity is a hallmark of an excessive dietary consumption of refined carbohydrates and a risk for diabetes mellitus. Too many physicians only bother with a fasting blood sugar. Instead, check the patient's system (under biologic stress) with a glucose level obtained at two hours after breakfast, lunch and dinner for three days. Do this by purchasing an over-the-counter (OTC) glucometer, or more easily with the Freestyle Libre System in conjunction with a simple food diary of what was eaten at those mealtimes. This is the most accurate means to determine a pre-diabetic or diabetic state.37
Another cancer fuel is LDL, so determine LDL particle numbers using the NMR lipoprofile (LabCorp test code 123810) and treat accordingly with LDL-lowering therapies.
Assessing the patient for exuberant release of bone-derived growth factors by testing for excessive bone breakdown using the urine test DpD (deoxypyridinoline) (LabCorp test code 511105) and treating appropriately if the DpD is high with agents that block cells called osteoclasts that release IL-6 and cause bone breakdown. Your physicians should be doing this. The vast majority, however, do not. A detailed discussion of the above can be found in Prostate Cancer. Essential Concepts for Survival.
All of the above affect the tumor microenvironment (TME). Measuring these biologic factors (e.g., DpD, NMR lipoprofile, post-prandial blood glucose (PPBG) at two hours after meals, inflammation markers) objectifies what we are doing to optimize health during AS and possibly prevents the disease from ever starting.
So, you see this is a complex situation. It is not simply selecting treatment A vs. B vs. C. Men would not decide on what car to purchase or which woman to marry based on only one parameter, they would do a far more detailed analysis; PC is no different. The "best way" to treat localized PC cannot be a recitation of treatment A vs. B. It first must involve all the inspections that must be done just as you would do when purchasing a house. Depending on how much work you put into the inspections, you either end up with a gem, or you own a lemon. You are the deciding factor.
In summation…
I was asked to write this article with the intent being to specify particular leading-edge treatments.
After reading over 400 articles, the harsh reality of a particular foundational truth came crashing down like a curtain falling at the end of a Shakespearean tragedy.
That truth was something shared with many of you over my many years in medicine.
Each of us is a unique biologic organism—with a distinctive set of biologic fingerprints.
When we forget this essential concept, the possibility of brilliant responses to treatment escapes us, and the probability of treatment-associated adverse effects leading to a diminution in the quality of our life, and a shortening of our time here becomes significantly greater.
In essence, we have shot ourselves in the foot, but a lot worse. I know this from my recent challenge with light chain amyloidosis and a close encounter with death that amazingly but not surprisingly was transformed into a durable complete remission, now over two years, when I explored additional factors such as my genetics and my tumor microenvironment.
I, therefore, have presented to you, the current and future patient, an insight that if applied will alter the duration and quality of your life.
John Ruskin was appalled at Whistler asking a huge price for a work. Ruskin said: "For two days labour, you ask two hundred guineas?" Whistler replied: "No, I ask for the knowledge of a lifetime."
Abbreviations Used in This Article
(suggest you print out and have handy while reading this article)
- < : less than
- ≤ : less than or equal to
- AA: arachidonic acid
- ADT: androgen deprivation therapy
- AI: artificial intelligence
- ANNs: artificial neural nets
- AR: androgen receptor
- ARS: active recognition sites
- AS: active surveillance
- BMD: bone mineral density
- BPH: benign prostatic hyperplasia
- CHB: combination hormone blockade
- DEXA or DXA: dual energy X-ray absorptiometry
- DHA: docosahexaenoic acid
- DHT: dihydrotestosterone
- DJD: degenerative joint disease
- DpD: deoxypyridinoline (aka Pyrilinks-D)
- DRE: digital rectal examination
- EBRT: external beam radiation therapy
- EOD: extent of disease
- EPA: eicosapentaenoic acid
- EPE: extra-prostatic extension
- FT: focal therapy
- GS: Gleason score
- HDL-C: high-density lipoprotein cholesterol
- HDR-brachytherapy: high-dose rate brachytherapy
- HIFU: High Intensity Focused Ultrasound
- HR: hazard ratio
- hsCRP: hypersensitive C-reactive protein
- IRE: irreversible electroporation
- LA: linoleic acid
- LDL-C: low-density lipoprotein cholesterol
- LH: luteinizing hormone
- ML: machine learning
- NLR: neutrophil to lymphocyte ratio
- NMR lipoprofile: nuclear magnetic resonance lipoprofile
- NSAIDs: non-steroidal anti-inflammatory drugs
- OCD: organ-confined disease
- PGE2: prostaglandin E2
- PI-RADS: Prostate Imaging Reporting and Data System
- PLR: platelet to lymphocyte ratio
- PM: predictive modeling
- PSA: prostate specific antigen
- PSAD: PSA density
- PSADT: PSA doubling time
- PSMA: prostate specific membrane antigen
- QCT: quantitative computerized tomography
- RP: radical prostatectomy
- RT: radiation therapy
- TI: therapeutic index
- TME: tumor microenvironment
- TRUS: transrectal ultrasound
- UBO: unique biologic organism
- VTP: vascular-targeted photodynamic therapy
- wb-MRI: whole body MRI
References
- Wollersheim BM, van Stam MA, Bosch R, et al. Unmet expectations in prostate cancer patients and their association with decision regret. J Cancer Surviv. Oct 2020;14(5):731-738. doi:10.1007/s11764-020-00888-6
- Chan Y, Chan K, Lam W, Metreweli C. Comparison of whole body MRI and radioisotope bone scintigram for skeletal metastases detection. Chin Med J (Engl). Jun 1997;110(6):485-9.
- Lauenstein TC, Freudenberg LS, Goehde SC, et al. Whole-body MRI using a rolling table platform for the detection of bone metastases. Eur Radiol. Aug 2002;12(8):2091-9. doi:10.1007/s00330-002-1344-z
- Steinborn MM, Heuck AF, Tiling R, Bruegel M, Gauger L, Reiser MF. Whole-body bone marrow MRI in patients with metastatic disease to the skeletal system. J Comput Assist Tomogr. Jan-Feb 1999;23(1):123-9.
- Ganzer R, Robertson CN, Ward JF, et al. Correlation of prostate-specific antigen nadir and biochemical failure after high-intensity focused ultrasound of localized prostate cancer based on the Stuttgart failure criteria - analysis from the @-Registry. BJU Int. Oct 2011;108(8 Pt 2):E196-201. doi:10.1111/j.1464-410X.2011.10091.x
- Iremashvili V, Kava BR, Manoharan M, Parekh DJ, Punnen S. Is It Time to Revisit the Role of Prostate-specific Antigen Kinetics in Active Surveillance for Prostate Cancer? Urology. Sep 2016;95:139-44. doi:10.1016/j.urology.2016.04.016
- Kongnyuy M, Islam S, Mbah AK, et al. PSA kinetics following primary focal cryotherapy (hemiablation) in organ-confined prostate cancer patients. World J Urol. Feb 2018;36(2):209-213. doi:10.1007/s00345-017-2130-5
- Zhang L, Loblaw A, Klotz L. Modeling prostate specific antigen kinetics in patients on active surveillance. J Urol. Oct 2006;176(4 Pt 1):1392-7; discussion 1397-8. doi:10.1016/j.juro.2006.06.103
- Paxton M, Barbalat E, Perlis N, et al. Role of multiparametric MRI in long-term surveillance following focal laser ablation of prostate cancer. Br J Radiol. Jul 29 2021:20210414. doi:10.1259/bjr.20210414
- Glass AS, Dall'Era MA. Use of multiparametric magnetic resonance imaging in prostate cancer active surveillance. BJU Int. Nov 2019;124(5):730-737. doi:10.1111/bju.14705
- Felker ER, Raman SS, Lu DSK, et al. Utility of Multiparametric MRI for Predicting Residual Clinically Significant Prostate Cancer After Focal Laser Ablation. AJR Am J Roentgenol. Dec 2019;213(6):1253-1258. doi:10.2214/AJR.19.21637
- Britschgi C, Riesterer O, Burger IA, Guckenberger M, Curioni-Fontecedro A. Report of an abscopal effect induced by stereotactic body radiotherapy and nivolumab in a patient with metastatic non-small cell lung cancer. Radiat Oncol. May 31 2018;13(1):102. doi:10.1186/s13014-018-1049-3
- Lippert TP, Greenberg RA. The abscopal effect: a sense of DNA damage is in the air. J Clin Invest. May 3 2021;131(9)doi:10.1172/JCI148274
- Soule E, Bandyk M, Matteo J. Percutaneous ablative cryoimmunotherapy for micrometastaic abscopal effect: No complications. Cryobiology. Jun 2018;82:22-26. doi:10.1016/j.cryobiol.2018.04.013
- Zhu L, Hu S, Chen Q, et al. Macrophage contributes to radiation-induced anti-tumor abscopal effect on transplanted breast cancer by HMGB1/TNF-alpha signaling factors. Int J Biol Sci. 2021;17(4):926-941. doi:10.7150/ijbs.57445
- Dall'Era MA, Klotz L. Active surveillance for intermediate-risk prostate cancer. Prostate Cancer Prostatic Dis. Mar 2017;20(1):1-6. doi:10.1038/pcan.2016.51
- Yamamoto T, Musunuru HB, Vesprini D, et al. Metastatic Prostate Cancer in Men Initially Treated with Active Surveillance. J Urol. May 2016;195(5):1409-1414. doi:10.1016/j.juro.2015.11.075
- Partin AW, Yoo J, Carter HB, et al. The use of prostate specific antigen, clinical stage and Gleason score to predict pathological stage in men with localized prostate cancer. J Urol. Jul 1993;150(1):110-4. doi:10.1016/s0022-5347(17)35410-1
- Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD. Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology. Dec 2001;58(6):843-8. doi:10.1016/s0090-4295(01)01441-8
- Makarov DV, Trock BJ, Humphreys EB, et al. Updated nomogram to predict pathologic stage of prostate cancer given prostate-specific antigen level, clinical stage, and biopsy Gleason score (Partin tables) based on cases from 2000 to 2005. Urology. Jun 2007;69(6):1095-101. doi:10.1016/j.urology.2007.03.042
- Stamey TA, McNeal JE, Yemoto CM, Sigal BM, Johnstone IM. Biological determinants of cancer progression in men with prostate cancer. JAMA. Apr 21 1999;281(15):1395-400. doi:10.1001/jama.281.15.1395
- Nakanishi H, Wang X, Ochiai A, et al. A nomogram for predicting low-volume/low-grade prostate cancer: a tool in selecting patients for active surveillance. Cancer. Dec 1 2007;110(11):2441-7. doi:10.1002/cncr.23055
- Carter HB, Kettermann A, Warlick C, et al. Expectant management of prostate cancer with curative intent: an update of the Johns Hopkins experience. J Urol. Dec 2007;178(6):2359-64; discussion 2364-5. doi:10.1016/j.juro.2007.08.039
- van den Bergh RC, Roemeling S, Roobol MJ, et al. Outcomes of men with screen-detected prostate cancer eligible for active surveillance who were managed expectantly. Eur Urol. Jan 2009;55(1):1-8. doi:10.1016/j.eururo.2008.09.007
- Carter HB, Walsh PC, Landis P, Epstein JI. Expectant management of nonpalpable prostate cancer with curative intent: preliminary results. J Urol. Mar 2002;167(3):1231-4.
- Strum SB, Allen LW, Rappaport H. Vascular invasion in Hodgkin's disease: its relationship to involvement of the spleen and other extranodal sites. Cancer. Nov 1971;28(5):1329-34. doi:10.1002/1097-0142(1971)28:5<1329::aid-cncr2820280536>3.0.co;2-s
- Westenend PJ, Meurs CJ, Damhuis RA. Tumour size and vascular invasion predict distant metastasis in stage I breast cancer. Grade distinguishes early and late metastasis. J Clin Pathol. Feb 2005;58(2):196-201. doi:10.1136/jcp.2004.018515
- Rezaianzadeh A, Talei A, Rajaeefard A, et al. Vascular invasion as an independent prognostic factor in lymph node negative invasive breast cancer. Asian Pac J Cancer Prev. 2012;13(11):5767-72. doi:10.7314/apjcp.2012.13.11.5767
- Ouyang FS, Guo BL, Huang XY, et al. A nomogram for individual prediction of vascular invasion in primary breast cancer. Eur J Radiol. Jan 2019;110:30-38. doi:10.1016/j.ejrad.2018.11.013
- Maltoni R, Fici P, Amadori D, et al. Circulating tumor cells in early breast cancer: A connection with vascular invasion. Cancer Lett. Oct 10 2015;367(1):43-8. doi:10.1016/j.canlet.2015.06.020
- Abdollahi A, Jahanian S, Hemmati N, Mohammadpour H. The Difference of Expression of 18 Genes in Axillary Invasion and Vascular Invasion Compared to Control Samples in Breast Cancer. Iran J Pathol. Summer 2019;14(3):223-231. doi:10.30699/ijp.2019.92094.1894
- Dall'Era M. Liquid biomarkers in active surveillance. World J Urol. Jan 2022;40(1):21-26. doi:10.1007/s00345-021-03609-5
- Zhao F, Vesprini D, Liu RSC, et al. Combining urinary DNA methylation and cell-free microRNA biomarkers for improved monitoring of prostate cancer patients on active surveillance. Urol Oncol. May 2019;37(5):297 e9-297 e17. doi:10.1016/j.urolonc.2019.01.031
- Paget S. The distribution of secondary growths in cancer of the breast. The Lancet. 1889;133(3421):571-573.
- Tourinho-Barbosa RR, de la Rosette J, Sanchez-Salas R. Prostate cancer multifocality, the index lesion, and the microenvironment. Curr Opin Urol. Nov 2018;28(6):499-505. doi:10.1097/MOU.0000000000000537
- Strum SB. Serenoa Repens (Saw Palmetto) for Lower Urinary Tract Symptoms (LUTS): The Evidence for Efficacy and Safety of Lipidosterolic Extracts. Part III. Uro. 2021;1(3):155-179.
- Zeevi D, Korem T, Zmora N, et al. Personalized Nutrition by Prediction of Glycemic Responses. Cell. Nov 19 2015;163(5):1079-1094. doi:10.1016/j.cell.2015.11.001