LIFE EXTENSION MAGAZINE

The U.S. Preventive Services Task Force (USPSTF) garners lots of attention when it makes new recommendations.
The USPSTF track record, however, is littered with errors that may collectively claim millions of lost life years.
We've exposed some of these tragedies in previous columns, such as the USPSTF recommending against PSA screening. The result has been an upsurge of metastatic prostate cancers that would have been curable if they had been caught in early stages using PSA blood tests.
The latest USPSTF proclamation advises against routine testing of vitamin D blood levels.1 They base this largely on a study where supplemental vitamin D by itself did not reduce fracture risk.2
Readers of this magazine know that it requires more than vitamin D alone to maintain bone density. The USPSTF seems oblivious to this.
Even more disturbing is the USPSTF's reliance on a study to discredit vitamin D that is loaded with so many defects that its findings are rendered virtually worthless.
One of the study's failings is that many in the placebo group were taking vitamin D supplements on their own, which diminished the difference between study subjects given vitamin D or placebo.
In this editorial I succinctly describe flaws in this widely publicized vitamin D study and how to best reduce fracture risks.
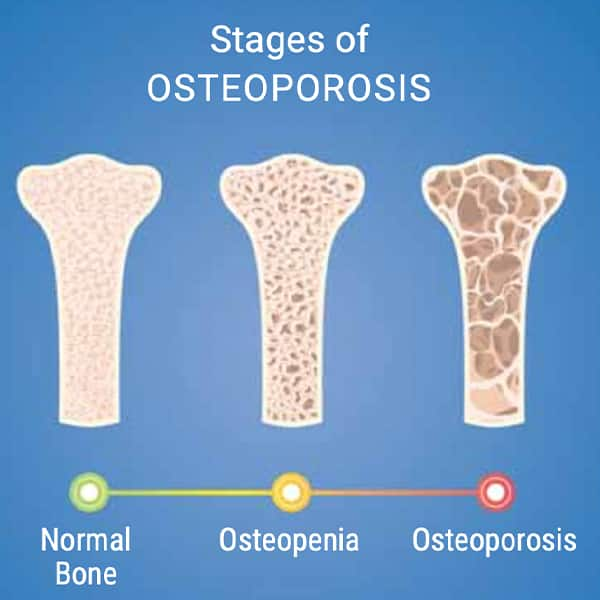
The importance cannot be overstated. A striking 43% of Americans over age 50 have low bone density that predisposes them to osteoporosis, shattered bones, and shortened longevity.3
Huge numbers of older Americans have less-than-optimal bone mass. Most don't know until they have a bone density test or suffer a crippling fracture.
Conventional medicine remains fixated on single agent therapies to protect bone mass. Yet it was well known decades ago that numerous factors contribute to osteoporosis and subsequent fractures.4,5
A study published in the New England Journal of Medicine evaluated people given 2,000 IU/day of supplemental vitamin D or placebo. When there was no difference in fracture rates between the two groups, the USPSTF, mainstream media, and some in conventional medicine advised against routine vitamin D blood testing.2
Overlooked were data sets showing that vitamin D requires magnesium to transform into its active form in the body. Most Americans are magnesium deficient.6
Also overlooked is the need for vitamin K to enable calcium and vitamin D to protect bone mass.7,8 Most Americans don't ingest optimal vitamin K.
Readers of Life Extension Magazine® already know it requires more than a single nutrient (like vitamin D) to maintain skeletal structure.
What pleasantly surprised me were harsh criticisms about this anti-vitamin D study that were later published in the New England Journal of Medicine (NEJM).
MAGNESIUM IS NEEDED TO ACTIVATE VITAMIN D
The graphic below depicts how magnesium is involved in the conversion of vitamin D from supplements and/or sunlight to a biologically active form.
Vitamin D from sunlight or supplements is converted by a magnesium-dependent enzymatic reaction to 25-hydroxyvitamin D in the liver.
It then converts to its biologically active 1,25-dihydroxy-vitamin D form in the kidneys also via a magnesium-dependent enzymatic reaction.
Activated vitamin D (1,25-hydroxy-vitamin D) is transported throughout the body in the blood via vitamin D-binding protein, for which magnesium is a cofactor.9
Conventional Doctors Condemn NEJM Study
Three months after the study attacking the value of vitamin D blood tests was published, the New England Journal of Medicine published a "correspondence" section of rebuttals.
The correspondence consisted of letters written by doctors critical of how the vitamin D study was designed and the conclusion to halt routine vitamin D blood testing.
Vitamin D Levels in Life Extension Readers
While conventional doctors debate the need for vitamin D blood testing, we at Life Extension uncovered the value decades ago when analyzing tens of thousands of vitamin D (25-hydroxyvitamin D) test results.
We found widespread individual variability even in people taking similar doses.
The chart on this page reveals the wide variation of 25-hydroxyvitamin D blood levels among Life Extension supporters.
When Life Extension staff see a 25-hydroxyvitamin D reading above 100 ng/mL, we notify the person that they are supplementing with too much vitamin D and should reduce their dose.
We reach out to those with very high 25-hydroxyvitamin D blood levels by phone and advise they discontinue vitamin D supplements until levels return to what we view as an optimal range of around 50-80 ng/mL.
We expect those in the low (0-30 ng/mL) range to know they need to increase their vitamin D intake.
Opinions on ideal ranges vary, but there is general consensus that 25-hydroxyvitamin D levels between 30 ng/mL-80 ng/mL confer protection and 71% of our supporters are in this range.
The optimal range of 25-hydroxyvitamin D to target is perhaps 50-80 ng/mL with 54% of our readers achieving this level.
Additional critiques
In addition to not providing broad-spectrum skeletal support to study subjects, there were other defects in this NEJM study that warrant further investigations.
The mean 25-hydroxyvitamin D level when the study began was 30.7 ng/mL. This is not considered deficient by the conventional medical community.
Among participants who provided two-year blood samples, the mean 25-hydroxyvitamin Dincreased from 29.2 ng/mL to 41.2 ng/mL in the vitamin D-supplemented group. It decreased slightly from 30.0 ng/mL to 29.4 ng/mL in the placebo arm.
An argument can be made that these differences are not clinically or statistically relevant in the context of this study. Neither vitamin D blood level meets Life Extension's optimal target range for 25-hydroxyvitamin D of 50-80 ng/mL.
The placebo group was allowed to supplement with up to 800 IU of vitamin D per day, and up to 1,200 mg per day of calcium. This hardly qualifies as a robust placebo group in the context of this study that sought to identify if 2,000 IU/day of supplemental vitamin D would reduce fracture rates.
We regret that only 4.8% of the participants were taking osteoporosis medications at baseline, yet 10.3% had a history of fracture caused by minor trauma. As much as one has to be selective about bone-building drugs, when one's bones are crumbling from severe osteoporosis, the proper medications have demonstrated significant benefits.
How to Avoid Osteoporotic-Induced Fractures
A leading cause of disability in the elderly is a fall, and fracture, followed by long term recuperation that can deteriorate into pneumonia, sarcopenia, and further bone loss due to lack of mobility.11
Aging men are particularly vulnerable to death from an osteoporotic fracture.12,13
A mistake many make is avoiding most, but not all osteoporotic risks.
For instance, a health-conscious person may avoid smoking, maintain youthful hormone balance, guard against nutrient deficiencies, cut back on alcohol, stay away from bone-depleting drugs (steroids, cortisone, proton-pump inhibitors, others), and engage in some degree of resistance training (weight-bearing exercise).
But for those predisposed to osteoporosis because of small body frame, family history, or lack of prevention initiated in early life, a comprehensive bone-protecting program is essential.
Some argue that failure to engage in weight-bearing exercise alone can cause significant bone loss that is not offset by other beneficial practices.
Those with significant bone loss or fracture history should consider bone-building medications, which would require a long chapter to discuss the pros and cons of each different drug class.
Doctors Harshly Critical of Anti-Vitamin D Study
Below are critiques by independent doctors about the anti-vitamin D study discussed in this editorial. These extracts were published on-line by the New England Journal of Medicine:10
"…the editorial on the VITAL trial…essentially advocates for clinicians to stop checking vitamin D levels or recommending supplementation. This advice is misguided and inconsistent with the data. The editorialists do not mention that the baseline vitamin D level in the participants was not low, which may be a reflection of the current era of supplementation by the general public. (More than 40% of the participants in this study were already taking vitamin D supplements, including those in the control group). Previous randomized trials involving patients with low vitamin D levels have shown a significant reduction in fracture risk. The editorialists also ignore the subgroup of participants in the VITAL trial who were receiving osteoporosis medication and who had a 46% reduction in fracture risk. Other outcomes from the same VITAL study showed a 22% reduction in the risk of autoimmune disease in participants who had a normal vitamin D level at baseline. In addition, other robust data have shown a reduction in the risk of infection (12% risk reduction overall and 70% risk reduction in patients with severe vitamin D deficiency). In light of data showing the benefits of vitamin D supplementation, the editorialists' broad recommendation to stop screening and supplementing vitamin D seems irresponsible."
"I would like to point out apparent errors in the editorial…on the VITAL study findings. The editorialists state that the VITAL trial showed decisively that vitamin D supplements do not significantly reduce the risk of bone fracture. However, the VITAL study population was not selected for vitamin D deficiency, and most participants had normal levels of vitamin D. Although 4,270 participants had a serum 25-hydroxyvitamin D level of less than 24 ng/mL (lowest quartile), only 227 fractures occurred in that group. Do the editorialists really believe that the trial provides conclusive evidence that persons with low vitamin D levels do not benefit from vitamin D supplements?On the basis of previous reports from the VITAL trial and other trials showing a lack of effect of vitamin D in preventing numerous medical conditions, the authors conclude that "providers should stop screening for 25-hydroxyvitamin D levels or recommending vitamin D supplements." This is an inaccurate summary of the VITAL results and fails to mention that vitamin D supplementation has been found to prevent autoimmune diseases and advanced (metastatic and fatal) cancer, with the latter confirmed by meta-analyses. Thus, there is no justification for claiming that patients should stop taking vitamin D supplements on the basis of available research."
"This article has received considerable coverage in the general media and has been inaccurately summarized as showing no benefit of supplemental vitamin D in patients with osteoporosis or vitamin D deficiency. As endocrinologists who care for patients with osteoporosis, we are concerned that this analysis, which was performed in a trial population with low fracture risk, will be used as evidence for not recommending vitamin D supplementation broadly and will negatively affect the treatment of patients at high fracture risk. The treatment of patients with osteoporosis, at a minimum, includes the intake of adequate calcium and vitamin D to reduce fracture risk."
"…should we follow the advice of the U.S. Preventive Services Task Force, which recommends against the routine monitoring of vitamin D levels in the first place? I am skittish about following that advice, because I have seen many cases of mild hyperparathyroidism that normalized with corrections of vitamin D levels from less than 20 ng/mL to 30 ng/mL or more…"
Why Life Extension and USPSTF So Often Disagree
The U.S. Preventive Services Task Force (USPSTF) has a mission to advise what the average American should do to reduce disease risk. Their recommendations take into consideration life expectancy of the average (typically unhealthy) elderly American and side effects caused by invasive diagnostics like colonoscopies (which USPSTSF recommended against in what now are considered higher risk age groups).14
Life Extension, on the other hand, seeks to radically extend the healthy human lifespan with no upper age limitation for when practical interventions should be considered.
As a result, there are often wide disparities on what the USPSTF advises for the "average" unhealthy American and what Life Extension suggests for supporters who are not average when it comes to protecting their precious health.
The USPSTF recommendation against routine vitamin D blood testing represents a tragic error that makes no sense in light of what we at Life Extension have studied and observed over many decades.
For longer life,
William Faloon, Co-Founder Life Extension®
References
- Available at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/vitamin-d-deficiency-screening. Accessed April 12, 2024.
- LeBoff MS, Chou SH, Ratliff KA, et al. Supplemental Vitamin D and Incident Fractures in Midlife and Older Adults. N Engl J Med. 2022 Jul 28;387(4):299-309.
- Available at: https://www.washingtonpost.com/health/the-big-number-141-million-americans-50-and-older-suffer-osteoporosis/2021/04/09/7ae5f382-9885-11eb-962b-78c1d8228819_story.html. Accessed April 12, 2024.
- Pouresmaeili F, Kamalidehghan B, Kamarehei M, Goh YM. A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag. 2018;14:2029-49.
- Available at: https://www.uptodate.com/contents/osteoporosis-prevention-and-treatment-beyond-the-basics. Accessed April 15, 2024.
- DiNicolantonio JJ, O'Keefe JH, Wilson W. Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart. 2018;5(1):e000668.
- Hu L, Ji J, Li D, et al. The combined effect of vitamin K and calcium on bone mineral density in humans: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2021 Oct 14;16(1):592.
- Lanham-New SA. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment. Proc Nutr Soc. 2008 May;67(2):163-76.
- Uwitonze AM, Razzaque MS. Role of Magnesium in Vitamin D Activation and Function. J Am Osteopath Assoc. 2018Mar 1;118(3):181-9.
- Vitamin D and Incident Fractures. New England Journal of Medicine. 2022;387(17):1625-8.
- Available at: https://www.nia.nih.gov/health/falls-and-falls-prevention/falls-and-fractures-older-adults-causes-and-prevention. Accessed April 16, 2024.
- Grewal S, Jawad AS. Morbidity associated with osteoporosis significant in older men. Trends in Urology & Men's Health. 2022;13(4):22-6.
- Available at: https://www.sciencedaily.com/releases/2017/03/170314081643.htm. Accessed April 12, 2024.
- Available at: https://www.uspreventiveservicestaskforce.org/uspstf/announcements/final-recommendation-statement-screening-colorectal-cancer-0. Accessed April 12, 2024.