LIFE EXTENSION MAGAZINE

In 1999, I reviewed an article for publication in this magazine that described a liver disease that I had not heard of.
The authors told me this "silent" disorder would lead to widespread illness and premature death.
Move forward 20 years, and nonalcoholic fatty liver disease has emerged as the leading cause of chronic liver disease.1
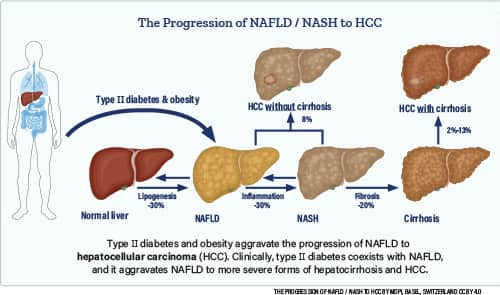
The underlying culprits are obesity and insulin resistance.2,3
In 1980, obesity was rare in the United States, affecting only 13% of adults according to some reports.4
In the most recent study period (2017-2018), a startling 42.4% of American adults were obese.5
Nonalcoholic fatty liver disease afflicts up to 75% of overweight adults, approximately 75% of type II diabetics, and about 90% of obese individuals.2,6
People with nonalcoholic fatty liver disease are seeking our assistance in combating its multiple morbidities.
The most effective treatment for early-to-mid-stage nonalcoholic fatty liver disease (NAFLD) is weight loss.7 Adjuvant approaches can also help.
Once NAFLD fatty liver disease advances to cirrhosis, the only long-term treatment option is a liver transplant.8
An article in this month’s issue describes ways to help protect liver health.
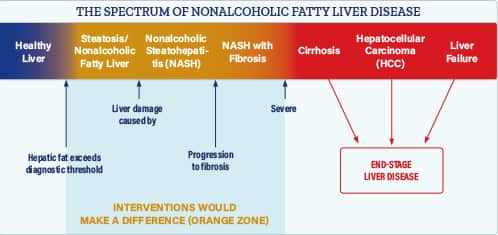
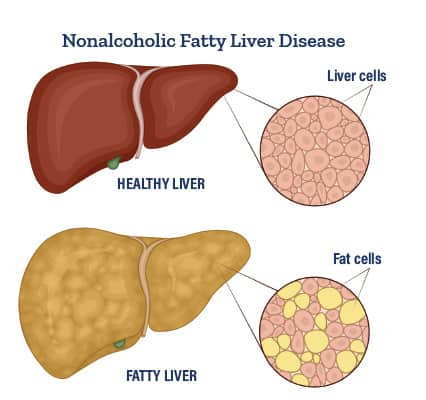
Nonalcoholic fatty liver disease or NAFLD begins when excess fat accumulates in liver cells. Over time, it can progress to advanced fibrosis and cirrhosis.9
As the condition is generally asymptomatic or has very mild symptoms initially, many people do not know they have it unless a blood test detects abnormal levels of liver enzymes.
When detected in time, NAFLD is a reversible condition, meaning those afflicted can avoid progressing to advanced-stage disease that requires a liver transplant.10
Fatty Liver Disease and Cancer
Liver failure is the most common manifestation of advanced nonalcoholic fatty liver disease (NAFLD).6
Another NAFLD risk is primary liver cancer called hepatocellular carcinoma.13 Five-year survival for this malignancy is less than 20%.14
A study published in 2018 evaluated 296,707 NAFLD patients and compared them with 296,707 matched controls. (This is a huge number of people to evaluate.)
This study found a more than 7.6-fold higher risk of hepatocellular carcinoma among NAFLD patients compared to controls.15
NAFLD patients with cirrhosis had an even greater incidence of hepatocellular carcinoma.
A medical-record review from this study found that approximately 20% of NAFLD patients with hepatocellular carcinoma had no evidence of cirrhosis.
This finding reveals hepatocellular carcinoma (HCC) risk in NAFLD patients who have not advanced to late-stage (cirrhosis) liver disease.15
This means people can skip past cirrhosis of the liver and develop primary liver cancer.
Diagnosing NAFLD
If you have a history of any of the following medical conditions you are at much greater risk of having some degree of NAFLD:6
- Excess body weight (abdominal obesity)
- Insulin resistance or type II diabetes
- Metabolic syndrome
Most patients with NAFLD, especially early in the disease, are asymptomatic, and are only identified when their disease becomes advanced.
Abnormal liver test results are frequently the earliest evidence of NAFLD, which emphasizes the value of routine laboratory testing to identify asymptomatic NAFLD patients.
Essential Liver Functions
More than 500 processes require healthy liver function, such as:11
- Making bile to carry away waste, break down fats during digestion
- Producing albumin and other blood plasma proteins
- Converting excess glucose into glycogen for storage
- Making proteins to carry fats through the body
- Balancing blood glucose levels
- Regulating blood levels of amino acids
- Processing hemoglobin
- Converting poisonous ammonia to urea
- Clearing the blood of drugs and other toxic substances
- Regulating blood clotting
- Resisting infections by making immune factors and removing bacteria from the bloodstream
- Clearing bilirubin
In advanced liver disease, when liver function is impaired, the result is systemic havoc that may manifest as fatigue, abdominal pain, and fluid accumulation, along with increased cardiovascular and diabetic risks.12
In particular, the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST) can be elevated in up to 50% of patients with NAFLD.16
Triglycerides can also be elevated in NAFLD but may not be in the early course of disease.
These three screening tests (ALT, AST, and triglycerides) are included in Life Extension®’s comprehensive CBC/Chemistry Panel for only $35.
The CBC/Chemistry Panel can be ordered 24-hours a day by calling 1-800-208-3444 or logging on to: www.LifeExtension/blood
Most of you live close to a drawing station so you can walk in for the CBC/Chemistry Panel at your convenience. Fast for eight hours before your blood draw.
Diagnosing Advanced Liver Disease
Symptoms of advanced NAFLD and cirrhosis can include loss of appetite, pain in the upper right abdomen, fatigue, muscle loss, and/or fluid accumulation in your belly (ascites).17
A physician’s exam can reveal an enlarged liver, spleen, and other clinical signs with advanced NAFLD.
There are a variety of imaging (MRI, ultrasounds, CT) and advanced blood tests that can detect suspicious liver abnormalities. These diagnostic tests are often useful to identify the degree of fatty liver damage.
One such blood test for those at risk is called NASH FibroSure. It is designed to assess what degree of liver damage has occurred.
The cost of this blood test is a prohibitive $595. For those with symptoms/signs of NAFLD, it might be best to have your physician prescribe this test and hopefully have it covered by your health insurance.
For definitive diagnosis, liver biopsies can establish the stage, and degree of structural damage in patients with NAFLD.
Reversing Damage Caused by NAFLD
If caught in time, healthy dietary and lifestyle choices can stop and help reverse fatty accumulation in your liver cells.
The single most effective way to control or reverse NAFLD is weight loss.
Those who wait for NAFLD to reach advanced stages have few treatment options beyond being placed on a liver transplant waiting list.
Prevention remains the most effective strategy!
For longer life,
William Faloon
Life Extension®
References
- Available at: https://www.ajmc.com/view/nafld-is-a-growing-driver-of-chronic-liver-disease-and-related-deaths. Accessed May 13, 2022.
- Kim H, Lee DS, An TH, et al. Metabolic Spectrum of Liver Failure in Type 2 Diabetes and Obesity: From NAFLD to NASH to HCC. Int J Mol Sci. 2021 Apr 26;22(9):4495.
- Kitade H, Chen G, Ni Y, et al. Nonalcoholic Fatty Liver Disease and Insulin Resistance: New Insights and Potential New Treatments. Nutrients. 2017 Apr 14;9(4).
- Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/su6001a15.htm. Accessed May 9, 2022.
- Available at: https://www.cdc.gov/nchs/products/databriefs/db360.htm. Accessed May 9, 2022.
- Available at: https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts. Accessed May 11, 2022.
- Available at: https://wwa.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/diagnosis-treatment/drc-20354573. Accessed May 10, 2022.
- Available at: https://www.uptodate.com/contents/cirrhosis-beyond-the-basics. Accessed May 10, 2022.
- Available at: https://www.uptodate.com/contents/pathogenesis-of-nonalcoholic-fatty-liver-disease. Accessed May 10, 2021.
- Available at: https://www.webmd.com/digestive-disorders/reverse-nonalcoholic-fatty-liver-disease. Accessed May 10, 2022.
- Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions. Accessed May 10, 2022.
- Available at: https://www.mayoclinic.org/diseases-conditions/liver-problems/symptoms-causes/syc-20374502. Accessed May 10, 2022.
- Piscaglia F, Svegliati-Baroni G, Barchetti A, et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: A multicenter prospective study. Hepatology. 2016 Mar;63(3):827-38.
- Available at: https://www.cancer.org/cancer/liver-cancer/detection-diagnosis-staging/survival-rates.html. Accessed May 10, 2022.
- Kanwal F, Kramer JR, Mapakshi S, et al. Risk of Hepatocellular Cancer in Patients With Non-Alcoholic Fatty Liver Disease. Gastroenterology. 2018 Dec;155(6):1828-37 e2.
- Oh RC, Hustead TR, Ali SM, et al. Mildly Elevated Liver Transaminase Levels: Causes and Evaluation. Am Fam Physician. 2017 Dec 1;96(11):709-15.
- Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/common-characteristics-of-liver-disease. Accessed May 10, 2022.