Life Extension Magazine®
The leading cause of acute liver failure in the United States is acetaminophen toxicity.1
Each year, this popular drug is responsible for thousands of emergency room visits and hundreds of deaths in the United States.
It took decades for groups like Life Extension to force the FDA to mandate a warning on the label of acetaminophen drugs about liver toxicity.
Regular use of acetaminophen is associated with increased risk of kidney damage, kidney cancer, and dementia, yet nothing on the label warns of these dangers.2-4
Ibuprofen is another over-the-counter drug that pain sufferers often take daily. Regular use can inflict stomach and kidney injuries.5
In 1995, OxyContin® was approved for routine pain relief. Makers of this drug recognized the potential to cause addiction and the resistance they would face from doctors.6
The company developed a fraudulent marketing campaign designed to promote OxyContin® as a time-released drug that was less prone to abuse.6
Between 1999 and 2019, nearly 500,000 people died from an overdose involving natural and synthetic opioids.7
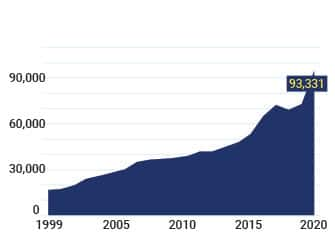
CDC data show that drug-related overdose deaths in 2020 hit a record high of 93,331 Americans.8,9
As you can see by the chart on this page, overdose deaths have surged higher since widespread prescribing of opioid drugs began around 1999.
Poisonings inflicted by non-opioid pain drugs continue to disable and kill.
This editorial describes an alternative that has been shown to work as well as acetaminophen for acute pain, without the side effects.
Number of drug overdose deaths in the U.S. from 1999 to 2020*
* Historical data from 1999 to 2020. Source: Centers for Disease Control and Prevention
Relief from acute and chronic pain is a major medical challenge.
Powerful nonsteroidal anti-inflammatory drugs (NSAIDs) were introduced in the 1960s-1970s. Their effectiveness was impeded by increased risk of peptic ulcers that resulted in thousands of deaths a year from acute gastrointestinal hemorrhage.
In the late 1990s, more selective anti-inflammatory drugs like Vioxx® were approved that mitigated stomach damage but doubled the risk of heart attack and stroke.10
Merc® withdrew Vioxx® in 2004 and later paid $4.85 billion to settle litigation for hiding the cardiovascular risks of this purportedly safer pain reliever.11,12
Most side effects caused by Vioxx® were associated with longer-term duration of usage and escalating dosages.
Non-Prescription Pain Killers
Over-the-counter drugs like ibuprofen and acetaminophen are widely used for acute and chronic pain relief.
While short-term moderate-dose use is safe, those who frequently take acetaminophen or NSAIDs face potential risks to their liver, kidneys, and other organs.13,14
If acetaminophen is combined with heavy alcohol ingestion, there is a higher risk of acute liver failure.15,16
Acetaminophen produces a toxic byproduct that depletes the liver of glutathione, which disables the liver’s ability to detoxify alcohol. This can lead to acute liver failure.17
Combining acetaminophen with alcohol to relieve a hangover can damage your liver.18,19
In the 1980s, one of our medical advisors suggested that we make a product that combined acetaminophen with N-Acetyl-L-Cysteine (NAC) to protect against glutathione depletion.
The challenge is the FDA requires expensive clinical trials when combining a drug with a nutrient.
There is no acetaminophen + N-Acetyl-L-Cysteine combination available today. Those who rely on acetaminophen may choose to take a 600 mg capsule of NAC with each acetaminophen dose.
Our Position on Routine Pain Relief
Acetaminophen, opioids, and some other analgesic drugs work in the central nervous system to dull the sense of pain.20
We at Life Extension have advocated for decades that it is more efficient to neutralize underlying causes.This includes pain resulting from joint cartilage degeneration or inflammation-induced musculoskeletal pain.
Reliance on drugs that block pain signals to the brain can enable the degenerative causes to worsen, leading many to increase their daily use of toxic pain relievers.
Many people find long-term relief using nutrients such as glucosamine, gamma linolenic acid (GLA) and/or omega-3s.
For those with acute discomfort, a novel nutrient blend has been shown to work as effectively as acetaminophen without the toxic side effects.
Excess Dietary Omega-6 Fats Cause Painful Inflammation
The American diet is loaded with omega-6 fats that are contributors to chronic inflammatory reactions.
Processed foods often contain fats high in omega-6s, like safflower, cottonseed, soybean, and corn oils.
When one ingests an omega-6 fat, there are two major pathways it follows in the body.
As shown on the chart on the next page, a common pathway is for an enzyme called delta-5-desaturase to convert omega-6s into pain-inducing prostaglandin E2 and leukotrienes.
The desired pathway for omega-6 fats is for enough of them to convert to an anti-inflammatory compound called prostaglandin E1.
A preclinical study showed that the sesame oil component known as sesamin inhibits the delta-5-desaturase enzyme,21 thus shunting more omega-6 fats away from pro-inflammatory pathways to anti-inflammatory prostaglandin E1.
Boswellia and turmeric extracts provide additional protection against omega-6 fats converting into leukotrienes and prostaglandin E2.22
Contrast the beneficial mechanisms of nutrients to acetaminophen that blocks pain signals to the brain, or COX-2 inhibitors like Celebrex® that impede only part of the pro-inflammatory omega-6 breakdown pathway.
Clinical Trial Compares Nutrients to Acetaminophen
To assess the efficacy of nutrients compared to acetaminophen, a clinical trial was conducted.
Half the people received 1,000 mg daily of acetaminophen while the other half received 1,000 mg daily of black sesame oil plus turmeric and Boswellia extracts.22
The blend of these extracts relieved pain as quickly and effectively as acetaminophen.22
Pain is more than just a physical experience. It also causes emotional strain.23
The nutrient blend was 8.57 times better than acetaminophen at relieving the emotional distress and unpleasantness of acute pain.22
This makes sense, as the nutrients combat underlying causes of musculoskeletal pain whereas acetaminophen works by blocking pain signals to the brain.
When assessing total pain relief endpoints in this study, the results showed the nutrient blend worked as well as acetaminophen.
Fast- versus Slow-Acting Nutrients
Nutrients like glucosamine and omega-3s do not provide immediate relief.
In contrast, a blend of black sesame oil plus turmeric and Boswellia extracts was shown to reduce pain scores to a similar degree as acetaminophen, starting day one.
These data indicate a potential for acute-pain suffers to find fast-acting relief, and an opportunity for chronic-pain sufferers to use this nutrient blend for an extended period, as there are no toxicity concerns.
Young Bodies Heal Fast
Children’s injuries usually heal quickly.
Healing rates in older adults are so slow that there are those who suffer immobility caused by injuries and persistent inflammation.24
Elderly individuals suffer musculoskeletal pain caused by degenerative processes that can be exacerbated by past or current injuries.
Chronic reliance on pain-relieving drugs can lead to side effects.
A better solution is to restore older persons to more youthful functionality, to reverse frailty, and to extinguish inflammatory fires that typically accompany aging.
Those suffering from musculoskeletal pain may consider a proprietary blend of black sesame oil-turmeric-Boswellia and also:
- Reduce ingestion of dietary omega-6 fats,
- Consume more omega-3s, and
- Reduce all forms of sugar intake.
In this month’s issue…
The article on page 50 of this month’s issue describes the research demonstrating pain relief in response to a combination of black sesame oil, turmeric and Boswellia.
Page 35 discusses a 2021 study showing that vinpocetine (used to boost cognitive function) can also help reverse certain forms of hearing loss.
Migraine sufferers continue to benefit from magnesium and a study described on page 70 of this issue further corroborates this.
Anti-Aging Update
In November 2020, headline news stories around the world announced findings from a hyperbaric oxygen study that lengthened telomeres by 20% in study subjects.25 The media proclaimed aging had been reversed for the first time in humans.
To achieve these telomere elongation benefits, study subjects underwent hyperbaric oxygen therapy plus breathing in pure oxygen five days a week for three consecutive months.
Telomeres are tips at the end our chromosomes that shorten with each cell division. When there is no more telomere structure, cells die.
We’ve been informed that a study will soon be published showing hyperbaric therapy combined with healthy behavior patterns elongated telomeres an average of 40% in older people!
We are carefully monitoring this research and interacting with the scientists to validate whether this telomere elongation is associated with indicators of systemic age reversal.
In the meantime, you can reduce your rate of telomere shortening by:25
- Engaging in healthy lifestyles
- Doing high-intensity interval training
- Ensuring adequate antioxidant intake
- Consuming high amounts of omega-3s
- Including walnuts in your diet
- Restricting your calorie intake
Healthy choices you make today help protect against a wide range of degenerative disorders, including reducing inflammatory pain and maintaining longer telomeres.
Your support of Life Extension helps us fund research that aims to reestablish youthful structure and function in our aging bodies.
For longer life,
William Faloon
Life Extension Buyers Club
Published in the Journal Aging on November 18, 2020
Hyperbaric oxygen therapy increases telomere length and decreases immuno-senescence in isolated blood cells: a prospective trial
"Results: Telomeres length of T helper, T cytotoxic, natural killer and B cells increased significantly by over 20% following hyperbaric oxygen therapy (HBOT).... There was a significant decrease in the number of senescent T helpers by -37.30%±33.04 post-HBOT. T-cytotoxic senescent cell percentages decreased significantly by -10.96%±12.59 post-HBOT.
In conclusion, the study indicates that HBOT may induce significant senolytic effects including significantly increasing telomere length and clearance of senescent cells in the aging populations."
Origins of the Opioid Crisis
In 1995, the FDA approved a time-released opioid drug called OxyContin® that purportedly was less prone to addiction and abuse compared to other prescription opioids.
Aggressive promotion of OxyContin® along with the FDA’s approval led to an epidemic of opioid addictions that continue to destroy the lives of millions of Americans.
Many endure the agonies of opioid withdrawal only to succumb to the powerful addicting properties and resume using prescription opioids or turn to street opioids like heroin and fentanyl.
The financial success of OxyContin® led about a dozen other pharma companies (including a subsidiary of Johnson & Johnson) to create their own opioid brands that were approved by the FDA and aggressively marketed to medical doctors and dentists.
The media blames opioid makers like Purdue Pharma for deliberately downplaying the addiction risk to doctors and illegally encouraging widespread prescribing.
While the actions of Purdue and other opioid makers are deplorable, I continue to argue that it was the FDA’s approval of the opioid drugs that enabled the criminal behaviors of Big Pharma to occur.
Physicians’ prescribing practices are largely based on whether the drug is approved by the FDA to treat a specific indication. In the case of extended-release opioid prescription drugs, the FDA approved them for pain relief and said they were less prone to addiction and abuse.26
Hurried physicians trusted the FDA’s approval process, even though it was later discovered that two FDA-employed doctors who pushed OxyContin® through the approval process went to work for Purdue Pharma soon after. (This is known as the “revolving door” that breeds corruption throughout Congress and governmental agencies.)
Had the FDA recognized that any opioid carries an addiction risk, this drug class would never have been approved for widespread use.
Even after addiction and overdose deaths became apparent, the FDA continued to approve other opioid drugs that were then inappropriately marketed to physicians for widespread use.
Authors of Hyperbaric Study Describe Other Methods Shown to Preserve Telomere Length
- High consumption of omega-3s
- Diet rich in walnuts
- Calorie restriction
- Healthy lifestyles
- High-intensity interval training
- Antioxidants
https://www.aging-us.com/article/202188/text
Novel Hyperbaric Oxygen Protocol Extends Telomere Length and Improves Immune Markers
- Some immune-cell telomeres elongated by over 20%.
- Some senescent immune cells reduced by 37%
- Improved immune markers.
First Hyperbaric Chamber Clinic of its Type Opens in Central Florida
Aviv Clinic The Villages, FL 32163
https://aviv-clinics.com/hyperbaric-centers/villages-florida/
References
- Available at: https://www.mayoclinic.org/diseases-conditions/acute-liver-failure/symptoms-causes/syc-20352863. Accessed October 13, 2021.
- Kanchanasurakit S, Arsu A, Siriplabpla W, et al. Acetaminophen use and risk of renal impairment: A systematic review and meta-analysis. Kidney Res Clin Pract. 2020 Mar 31;39(1):81-92.
- Choueiri TK, Je Y, Cho E. Analgesic use and the risk of kidney cancer: a meta-analysis of epidemiologic studies. Int J Cancer. 2014 Jan 15;134(2):384-96.
- Jones GR. The Alzheimer pandemic: is paracetamol to blame? Inflamm Allergy Drug Targets. 2014 Feb;13(1):2-14.
- Available at: https://www.drugs.com/sfx/ibuprofen-side-effects.html. Accessed October 14, 2021.
- Available at: https://www.nytimes.com/2007/05/10/business/11drug-web.html. Accessed October 18, 2021.
- Available at: https://www.cdc.gov/opioids/data/analysis-resources.html. Accessed October 18, 2021.
- Available at: https://www.commonwealthfund.org/blog/2021/drug-overdose-toll-2020-and-near-term-actions-addressing-it. Accessed October 18, 2021.
- Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed October 18, 2021.
- Available at: https://www.reuters.com/article/us-stroke-vioxx-idUSTRE49C84M20081013. Accessed October 14, 2021.
- Wadman M. Merck settles Vioxx lawsuits for $4.85 billion. Nature. 2007 2007/11/13.
- Available at: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/vioxx-rofecoxib-questions-and-answers. Accessed October 19, 2021.
- Moore N, Scheiman JM. Gastrointestinal safety and tolerability of oral non-aspirin over-the-counter analgesics. Postgrad Med. 2018 Mar;130(2):188-99.
- Keen MU, Aeddula NR. Analgesic Nephropathy. StatPearls. Treasure Island (FL)2021.
- Available at: https://www.raps.org/regulatory-focus™/news-articles/2015/11/fda-amends-liver-warning-labeling-guidance-for-some-otc-drugs-containing-acetaminophen. Accessed October 14, 2021.
- Zimmerman HJ, Maddrey WC. Acetaminophen (paracetamol) hepatotoxicity with regular intake of alcohol: analysis of instances of therapeutic misadventure. Hepatology. 1995 Sep;22(3):767-73.
- Available at: https://www.sciencedaily.com/releases/2002/10/021014072451.htm. Accessed October 14, 2021.
- Available at: https://www.medpagetoday.com/opinion/inotherwords/14895. Accessed October 19, 2021.
- Available at: https://health.clevelandclinic.org/is-acetaminophen-safe-to-take-when-youre-drinking/. Accessed October 19, 2021.
- Sullivan D, Lyons M, Montgomery R, et al. Exploring Opioid-Sparing Multimodal Analgesia Options in Trauma: A Nursing Perspective. J Trauma Nurs. 2016 Nov/Dec;23(6):361-75.
- Shimizu S, Akimoto K, Shinmen Y, et al. Sesamin is a potent and specific inhibitor of delta 5 desaturase in polyunsaturated fatty acid biosynthesis. Lipids. 1991 Jul;26(7):512-6.
- Rudrappa GH, Chakravarthi PT, Benny IR. Efficacy of high-dissolution turmeric-sesame formulation for pain relief in adult subjects with acute musculoskeletal pain compared to acetaminophen: A randomized controlled study. Medicine (Baltimore). 2020 Jul 10;99(28):e20373.
- Talbot K, Madden VJ, Jones SL, et al. The sensory and affective components of pain: are they differentially modifiable dimensions or inseparable aspects of a unitary experience? A systematic review. Br J Anaesth. 2019 Aug;123(2):e263-e72.
- Morri M, Ambrosi E, Chiari P, et al. One-year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep. 2019 Dec 10;9(1):18718.
- Hachmo Y, Hadanny A, Abu Hamed R, et al. Hyperbaric oxygen therapy increases telomere length and decreases immunosenescence in isolated blood cells: a prospective trial. Aging (Albany NY). 2020 Nov 18;12(22):22445-56.
- Available at: https://www.nytimes.com/2018/05/29/health/purdue-opioids-oxycontin.html. Accessed October 19, 2021.