Life Extension Magazine®

A documentary titled “Burden of Genius” was screened in late 2018 at Baylor University Medical Center.
The film depicts the relentless determination of a surgeon who made liver transplantation the routine procedure it is today.
The surgeon’s name is Thomas Starzl, M.D., Ph.D.
Despite fierce criticism that organ transplants were impossible, Dr. Starzl’s early efforts now save 20,000 lives each year.2
Dr. Starzl began liver transplant studies in 1958 with almost no resources.3 Back then, the notion of replacing a diseased liver with a healthy one was viewed as utter fantasy.
In 1963, Dr. Starzl attempted the first human liver transplant.4 The patient died on the operating table. Several other attempts resulted in tragic outcomes. Critics called him “reckless.”
The difficulties extended beyond connecting a new liver. A series of biochemical obstacles also had to be overcome, including organ rejection.
Dr. Starzl persevered against a tidal wave of technical and legal challenges. Today he is recognized as the “father of transplantation.”4
Today’s Liver Crisis
All rights reserved.
In the February 2004 issue of Life Extension® magazine, we described a condition that few doctors had heard about. It’s called non-alcoholic fatty liver disease or NAFLD.5
The disease ranges from simple fatty buildup to advanced fibrosis and cirrhosis. This end result can be liver failure and/or liver cancer.
Our predictions of an NAFLD epidemic have turned tragically real. NAFLD is expected to be the leading reason for people to require liver transplants in 2020.6
Approximately 25% of Americans suffer the damaging effects of NAFLD. Its prevalence and severity in overweight individuals are far higher.7,8
The encouraging news is that NAFLD is often a reversible condition, meaning those afflicted can avoid progressing to diseases like fibrosis and cirrhosis that increase the need for a liver transplant.
People often trivialize scientific advances that were considered impossible when the idea was conceived.
Instead of recognizing the heroic accomplishments of pioneering individuals, the attitude is that their discovery was obvious, and someone would have eventually done it. This is the opposite of reality.
“With determination and irresistible resolve, Thomas Starzl advanced medicine through his intuition and uncanny insight into both the technical and human aspects of even the most challenging problems.”9
How One Individual Changed the World

The accomplishments of Dr. Starzl are worthy of a book that should be mandatory reading for medical students.
Dr. Starzl spent decades discovering and improving the full spectrum of organ transplantation technologies. He tirelessly educated other surgeons so they could perform these lifesaving procedures worldwide.
In between, he battled an apathetic and sometimes hostile establishment that raised “ethical and legal” obstacles relating to organ transplantation.
To put the enormity of Dr. Starzl’s work in perspective, there was a time when he was averaging the publication of a new scientific paper every 7.3 days!3 In responding to pessimists Dr. Starzl wrote:
“What was inconceivable yesterday, and barely achievable today, often becomes routine tomorrow.”3
Challenges of Transplanting A Liver
Few people understand the difficulties of performing a liver transplant.
Some view transplantation as simple as removing and replacing parts like a toy model.
The reality is that liver transplantation requires the intricate disconnect and reconnect of blood vessels, ligaments, and ducts... while keeping the patient alive on the operating table.10
The metabolic challenges are more complex. A patient can die from coagulation imbalance, acidosis, ammonia toxicity, or the acute deficit of other critical liver functions.11-16
Lifelong monitoring, and anti-organ-rejection drugs are required.
The challenge of identifying tissue-type-matched donor organs in a timely manner was considered insurmountable in early years.
Why the Liver Is Essential to Sustain Life
Everything one ingests that is absorbed from the stomach or intestines first passes through the liver. This is where food, drinks, drugs and most everything else you consume is detoxified and/or converted into forms that are easier to use in cells throughout the body.
At any given moment, the liver contains about 13% of the body’s entire blood supply.19 As blood moves through the liver, numerous life-sustaining metabolic processes are performed.
This includes detoxifying ammonia that is a byproduct of normal cell metabolism.
Acute liver failure results in rapid ammonia buildup that quickly kills unless some liver function is restored.
Chronic liver dysfunction can result in excess ammonia levels that dangerously impact one’s health and wellbeing.15,16
The liver contains specialized proteins that vitamin K activates to enable blood to properly coagulate. A dysfunctional liver adversely impacts blood clotting.20
Diabetes is often thought of as a pancreatic disorder, but the liver also regulates glycemic control by, among other things, storing excess blood glucose (as glycogen). It then releases glucose back into the blood as needed. Type II diabetics often have impaired liver function that results in poorly controlled blood glucose.21,22
Healthy digestion is highly dependent on the liver to produce bile that breaks down dietary fats for absorption in the small intestine.

Few understand the difficulty of advancing transplant technology.
Some think organ transplantation is as simple as removing and replacing parts like a model.
Replacing an organ requires the intricate disconnect and reconnect of vasculature, peritoneum, ligaments, and much more... it is exceedingly complex.
Chronic Illnesses Can Begin in the Liver
Age-related diseases often begin as the liver slowly fails. That’s because the liver is responsible for everything you’ve read so far and more, including:19,23-25
-
Degrading old, red blood cells to make room for new, red blood cells that can efficiently carry oxygen,
-
Producing lipoproteins essential to transport fats, and
-
Making essential plasma proteins (like albumin).
The liver is responsible for more than 500 vital functions, including making immunoglobulins, that are essential for immune health.19
When the liver completely fails, the result is death unless a transplant is readily available.
Today’s Chronic Liver Disease Issue
Hepatitis C was once a leading cause of liver cirrhosis, liver cancer and eventual liver failure.
Drugs approved seven years ago now cure over 90% of hepatitis C viral infections.26 This is an under-appreciated medical breakthrough.
Liver cirrhosis caused by excess alcohol consumption has remained rather constant over the past four decades.27
The disorder that is explosively increasing in prevalence is non-alcoholic fatty liver disease, which is abbreviated as NAFLD.
NAFLD represents more than 75% of all liver disease. Its severe form, non-alcoholic steatohepatitis (NASH), is becoming a leading reason people need liver transplants.28
Long before acute liver failure occurs, NAFLD can inflict multiple miseries when it progresses to its more severe form, NASH, which causes a chronic inflammatory disorder that impacts quality of life.
Most physicians respond to the health problems caused by NAFLD by prescribing drugs to treat the various disorders that arise as liver function declines.
A better approach is to reverse the damage and fat in the liver by increasing insulin sensitivity and lowering glucose and lipid levels. This can be accomplished by losing excess body fat and increasing physical activity.
These lifestyle changes are easier said than done.
NAFLD that has progressed to NASH can be so severe that more than dietary and physical activity improvements are needed.
New Approach to A Healthier Liver
NAFLD and NASH increase the risk of death from liver disease by 1.5-fold to over 10-fold.29
Before causing death, the buildup of fibrotic (non-functional) liver tissue ignites a series of chronic conditions that are often confused with degenerative aging.
Decades ago, Life Extension® identified nutrients to help benefit those afflicted with non-alcoholic fatty liver disease (NAFLD).
The nutrients included n-acetylcysteine,30,31 milk thistle extract,32,33 and an expensive nutrient (sold as a drug in Germany) called polyenylphosphatidylcholine (PPC).34
I’m pleased to announce a new approach that demonstrates a marked reduction in severe liver-fibrosis scores in addition to the modest benefits achieved by lifestyle modifications.
This non-drug method showed a 46% decrease in C-reactive protein (CRP), indicating a significant lowering of systemic inflammation.
The article on page 46 of this month’s issue describes this advance that may save lives while improving one’s quality of life.
This is of particular importance to abdominally obese individuals who have chronically elevated inflammatory markers (such as C-reactive protein).
The burden of NAFLD on the escalation of liver disease can be summarized in the following percentages of those afflicted:8
Adults |
Percent with NAFLD |
|
|
|
|
Obese → Overweight → Normal Weight → |
Up to 91% Between 35-67% Up to 25% |
|
|
|
A Hero Today
I grew up in Pittsburgh, Pennsylvania, at the time Dr. Starzl was performing the first, human liver transplants in the 1960s.
Yet the first time I heard his name was in 2017 in an obituary announcing his death at the age of 90. (I read obituaries to increase my motivation to keep me and you out of them.)
As I read how Dr. Starzl saved so many lives, I lamented that he is not a more recognized name.
By the time of his death, Thomas Starzl, M.D. Ph.D. had a towering reputation in the field of transplant medicine, yet sports stars of his era are whom most people recognize and idolize.
Critics called Dr. Starzl reckless. Yet his relentless exploration and clinical implementation changed the course of transplantation medicine forever.
Liver Transplant Complexities
A patient with a failing liver is put on a waiting list and told to be available on a moment’s notice.
The liver-failure patient relies on someone else to tragically die and the deceased individual’s liver to be harvested in a timely fashion and then transported for rapid transplantation.
There is a severe shortage of donor organs. Each year, about 7,000 Americans with failing livers die because a suitable transplant does not become available in time.17
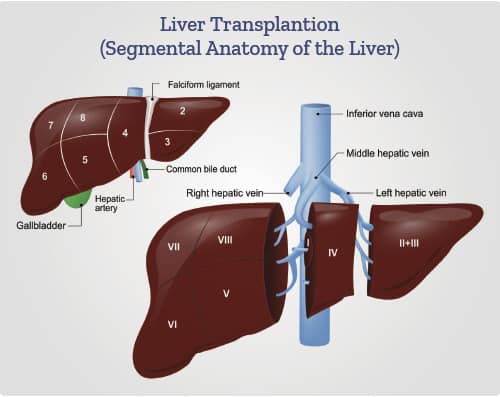
The operation is done through a large incision in the upper abdomen.
The surgical procedure involves severing and reattaching the common bile duct, the hepatic artery, the hepatic vein and the portal vein, as well as ligaments that hold the liver in place.10
Additional vascular surgery involves the inferior vena cava (the largest vein in the body that is located in the thoracic and abdominal regions).10,18
The donor’s blood in the liver is replaced by an ice-cold, organ-storage solution, until the donated liver is implanted into the liver-failure patient’s body.
Implantation involves anastomoses (surgical connections) of the inferior vena cava, portal vein, and hepatic artery. After blood flow is restored to the new liver, the biliary (bile duct) connection is constructed, either to the recipient’s bile duct or small intestine.10
The surgery usually takes between four and eight hours.
During the surgical procedure careful monitoring of the patient is needed as there are many complex challenges (such as coagulation imbalances) that can result in the patient’s death on the operating table.
Precise use of organ-rejection drugs is then needed.
Dr. Starzl pioneered and relentlessly improved all of the above.
Annual Super Sale
For the 31st consecutive year, we are discounting the price of all our advanced nutritional formulas.
Long-time readers take advantage of this annual sale, along with additional discounts to obtain premium-grade nutrients at the year’s best pricing.
This year’s Super Sale ends on Feb. 3, 2020. With the free shipping available to Premier Rewards customers, consider ordering what you need now and then prepare your longer list in January 2020.
As many of you learned decades ago, our commitment to quality is backed by our unrelenting efforts to eradicate degenerative aging.
To order nutrients you need at Super Sale prices, call 1-800-544-4440 (24 hours).
For longer life,
William Faloon, Co-Founder
Life Extension Buyers Club
References
- Available at: http://www.baylortransplant.com/Pages/Burden-of-Genius.aspx. Accessed October 16, 2019.
- Available at: http://www.cell.com/article/S009286741201063X/fulltext. Accessed October 16, 2019.
- Eghtesad B, Fung J. Thomas Earl Starzl, MD, PhD (1926–2017): Father of Transplantation. International Journal of Organ Transplantation Medicine. 2017;8(2):e1.
- Available at: https://www.latimes.com/archives/la-xpm-1992-08-30-mn-8477-story.html. Accessed October 17, 2019.
- Available at: https://www.lifeextension.com/Magazine/2004/2/report_liver. Accessed October 17, 2019.
- Canbay A, Sowa J-P, Syn W-K, et al. NASH Cirrhosis - the New Burden in Liver Transplantation: How Should It Be Managed? Visceral medicine. 2016;32(4):234-8.
- Alkhouri N, Scott A. An Update on the Pharmacological Treatment of Nonalcoholic Fatty Liver Disease: Beyond Lifestyle Modifications. Clin Liver Dis (Hoboken). 2018 Apr;11(4):82-6.
- Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018 Jan;15(1):11-20.
- Available at: https://www.upmc.com/media/news/starzl-obit. Accessed October 17, 2019.
- Available at: https://emedicine.medscape.com/article/431783-treatment#showall. Accessed October 17, 2019.
- Kim S, DeMaria S, Jr., Li J, et al. Persistent acidosis after reperfusion-A prognostic indicator of increased 30-day and in-hospital postoperative mortality in liver transplant recipients. Clin Transplant. 2019 Mar;33(3):e13473.
- Northup P, Reutemann B. Management of Coagulation and Anticoagulation in Liver Transplantation Candidates. Liver Transpl. 2018 Aug;24(8):1119-32.
- Tripodi A, Primignani M, Chantarangkul V, et al. An imbalance of pro- vs anti-coagulation factors in plasma from patients with cirrhosis. Gastroenterology. 2009 Dec;137(6):2105-11.
- Gopal PB, Kapoor D, Raya R, et al. Critical care issues in adult liver transplantation. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2009 Jul-Sep;13(3):113-9.
- Niranjan-Azadi AM, Araz F, Patel YA, et al. Ammonia Level and Mortality in Acute Liver Failure: A Single-Center Experience. Ann Transplant. 2016 Aug 2;21:479-83.
- Olde Damink SW, Deutz NE, Dejong CH, et al. Interorgan ammonia metabolism in liver failure. Neurochem Int. 2002 Aug-Sep;41(2-3):177-88.
- Available at: https://www.americantransplantfoundation.org/about-transplant/facts-and-myths/. Accessed October 17, 2019.
- Available at: https://transplant.surgery.ucsf.edu/conditions--procedures/liver-transplant.aspx. Accessed October 17, 2019.
- Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions. Accessed October 17, 2019.
- Senzolo M, Burra P, Cholongitas E, et al. New insights into the coagulopathy of liver disease and liver transplantation. World journal of gastroenterology. 2006;12(48):7725-36.
- Yamada T, Fukatsu M, Suzuki S, et al. Fatty liver predicts impaired fasting glucose and type 2 diabetes mellitus in Japanese undergoing a health checkup. J Gastroenterol Hepatol. 2010 Feb;25(2):352-6.
- Mohamed J, Nazratun Nafizah AH, Zariyantey AH, et al. Mechanisms of Diabetes-Induced Liver Damage: The role of oxidative stress and inflammation. Sultan Qaboos University medical journal. 2016;16(2):e132-e41.
- Available at: https://www.ncbi.nlm.nih.gov/books/NBK305896/. Accessed,
- Available at: https://www.ncbi.nlm.nih.gov/books/NBK535438/#article-24376.s5. Accessed October 17, 2019.
- Klei TRL, Meinderts SM, van den Berg TK, et al. From the Cradle to the Grave: The Role of Macrophages in Erythropoiesis and Erythrophagocytosis. Frontiers in Immunology. 2017 2017-February-02;8(73).
- Available at: https://www.verywellhealth.com/list-of-approved-hepatitis-c-drugs-3576465. Accessed October 17, 2019.
- Ahmed O, Liu L, Gayed A, et al. The Changing Face of Hepatocellular Carcinoma: Forecasting Prevalence of Nonalcoholic Steatohepatitis and Hepatitis C Cirrhosis. Journal of Clinical and Experimental Hepatology. 2019;9(1):50-5.
- Hassan K, Bhalla V, El Regal ME, et al. Nonalcoholic fatty liver disease: a comprehensive review of a growing epidemic. World J Gastroenterol. 2014 Sep 14;20(34):12082-101.
- Musso G, Gambino R, Cassader M, et al. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011 Dec;43(8):617-49.
- Khoshbaten M, Aliasgarzadeh A, Masnadi K, et al. N-acetylcysteine improves liver function in patients with non-alcoholic Fatty liver disease. Hepat Mon. 2010 Winter;10(1):12-6.
- El-Lakkany NM, Seif El-Din SH, Sabra AA, et al. Co-administration of metformin and N-acetylcysteine with dietary control improves the biochemical and histological manifestations in rats with non-alcoholic fatty liver. Res Pharm Sci. 2016 Oct;11(5):374-82.
- Zhong S, Fan Y, Yan Q, et al. The therapeutic effect of silymarin in the treatment of nonalcoholic fatty disease: A meta-analysis (PRISMA) of randomized control trials. Medicine (Baltimore). 2017 Dec;96(49):e9061.
- Loguercio C, Federico A, Trappoliere M, et al. The effect of a silybin-vitamin e-phospholipid complex on nonalcoholic fatty liver disease: a pilot study. Dig Dis Sci. 2007 Sep;52(9):2387-95.
- Gundermann K-J, Gundermann S, Drozdzik M, et al. Essential phospholipids in fatty liver: a scientific update. Clinical and experimental gastroenterology. 2016;9:105-17.

