Life Extension Magazine®

Homocysteine was discovered in 1932, but its role in promoting atherosclerosis went largely unrecognized until 1969.1
For many decades, conventional medicine was so focused on cholesterol that homocysteine went unnoticed.
We helped ignite the debate with our 1981 publication showing high homocysteine blood levels increase heart attack and stroke risk. Since then, we’ve published dozens of articles about the life-shortening impact of excess homocysteine, and how easy it is to lower it.
New studies link high homocysteine to degenerative brain disorders. These reports yield critical pieces of data that explain why some homocysteine-lowering studies do not yield expected benefits.2-4
For example, a group of researchers found that people using B vitamins to lower homocysteine must also have sufficient omega-3s to protect brain function.5
Brain cells require DHA (an omega-3 fat) for structure and function. It is not surprising that some clinical trials using B vitamins to improve neurological status show benefits only in people with higher omega-3 levels.6
Additional findings reveal how much more effective “activated” B vitamins such as 5-MTHF (folate) are at pushing down elevated homocysteine, especially in elderly individuals.7,8
This issue of Life Extension Magazine® reviews startling new findings about the pathological role of homocysteine in degenerative brain aging.
In the January 2017 issue of this magazine, we described how abnormal clotting inside blood vessels (thrombosis) is the leading cause of disability and death in people over age 50.9
Those with atrial fibrillation (irregular rhythm in upper heart chambers) are at a five-fold increased risk for stroke.10
Anticoagulant drugs (such as warfarin or Eliquis®) reduce thrombotic stroke risk by about 60% in atrial fibrillation cases.11,12 So what about the 40% of atrial fibrillation patients that do not respond to anticoagulant drugs?
One solution is to suppress their elevated homocysteine.
Excess homocysteine contributes to thrombotic events. In a study of atrial fibrillation patients, high homocysteine quadrupled risk of stroke.13
Homocysteine increases as we age. One study found elevated homocysteine levels (defined as greater than 14 µmol/L) in almost 30% of people older than 65 years, a figure that rose to more than 40% in those aged 80 years and older. Having dangerously high homocysteine increases the incidence of stroke and other vascular disorders.14,15
Considering how easy it is to bring homocysteine into safer ranges, it is regrettable that the medical establishment does not focus more attention on this common disease risk factor.
Cognitive Impairment in Parkinson’s Disease

Parkinson’s disease not only causes loss of motor control, but a high percentage of patients develop serious cognitive impairment.
A study published in January 2017 showed that Parkinson’s patients with cognitive dysfunction were more likely to have five-point higher homocysteine levels.16
Just imagine how easy it might be to restore cognition in these individuals by giving them high-potency activated B vitamins like 5-MTHF (folic acid) and methylcobalamin (vitamin B12).
Why Conventional Folate Supplements Do Not Optimally Lower Homocysteine
 |
Homocysteine is decreased in the body by 5-methyltetrahydrofolate (5-MTHF).7
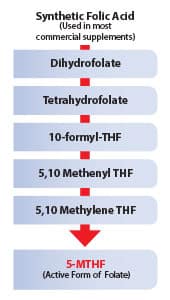
When folic acid is taken, it must go through several enzymatic changes to convert to 5-MTHF.
A surprising number of people, especially as they age, lack the enzymes needed to convert folic acid into metabolically active 5-MTHF.17 These individuals need to take a 5-MTHF supplement to directly supply their body with the form of folate that reduces homocysteine.
This chart shows the many steps required by the body to convert folic acid to 5-MTHF.
If one is supplementing with folic acid yet still suffers higher-than-optimal homocysteine, they should add 1 mg (1,000 micrograms) to 10 mg (10,000 micrograms) of 5-MTHF to their daily supplement regimen. This higher potency 5-MTHF supplement is now available without a prescription.
Low-Potency Folate Supplements Often Ineffective
Most conventional physicians are not trained on the optimal use of folate supplements. As a result, they inadvertently design clinical trials using low potencies of the least effective forms of folic acid.
The chart on this page shows the many enzymatic steps required to convert the folic acid found in commercial supplements into activated 5-MTHF.
Some people only need commercial folic acid to lower their homocysteine since they have high enzymatic activity to convert it to 5-MTHF. Many others lack the ability to convert folic acid to its active form (5-MTHF), especially as they age.17,18 These individuals often suffer disorders related to excess homocysteine.19-22
There are studies where folic acid potencies of 400-800 mcg are used with little benefit derived. We know from decades of experience in working with our supporters that higher doses of folate and other B vitamins are often needed to drop homocysteine into safer ranges.
For instance, when a blood test reveals elevated homocysteine, we suggest that 1,000 mcg of 5-MTHF be taken once or twice daily in addition to the 400 mcg of 5-MTHF included in our multivitamin formulas.
If this dose fails to sufficiently reduce homocysteine, we then suggest 5,000 mcg of 5-MTHF once or twice daily, along with higher potencies of the methylcobalamin form of vitamin B12 and higher doses of pyridoxal-5-phosphate, which is an “activated” form of vitamin B6.
Compared to poorly designed trials where 400-800 mcg potencies of folic acid are used along with less active forms of B12 and B6, we are suggesting higher doses of more effective forms of B vitamins.
Based on very recent studies, anyone with elevated homocysteine should also consider taking an omega-3 supplement in order to derive brain-health benefits.5,6,23
Omega-3s and B Vitamins Prevent Brain Atrophy
As we age, our brain literally shrivels in size. As this happens, we experience a wide range of neurological disorders.
A study was done on elderly people with mild cognitive impairment who were randomly assigned to receive folic acid (800 mcg), vitamin B6 (20 mg), and B12 (500 mcg) or placebo.5
The study authors described these potencies as “high-dose,” whereas for many people with elevated homocysteine, these are insufficient potencies of less active forms of B vitamins. This study nonetheless revealed some intriguing new findings.
Both groups (B-vitamin supplemented and placebo) underwent MRI brain imaging at baseline and two years later.
In the B-vitamin group that had high baseline omega-3 blood levels, the mean brain atrophy rate was slowed by a remarkable 40% compared to placebo.5 There was no significant benefit amongst the B-vitamin group with low baseline omega-3 blood levels.
In the placebo arm of the study, there was no slowdown of brain shrinkage (atrophy) even in the presence of higher omega-3s.
This study provides intriguing new data on the importance of consuming B vitamins and omega-3s to protect against brain atrophy.
Another recent study showed B vitamins plus omega-3s enhanced the mental performance benefits in elderly people with mild cognitive impairment. Among those with good omega-3 status, B-vitamin treatment resulted in 63% more elderly subjects deriving cognitive benefits.6
As with the brain atrophy study, this trial showed there was no effect of B vitamins when omega-3 levels are low, but significant benefit when B vitamins were given to elderly subjects whose omega-3 status was in the upper-normal range.
Take-home lesson:
- B vitamins + omega-3s =
- Delayed Brain Aging.
Postmenopausal Mental Decline

Postmenopausal women are prone to accelerated loss of a wide range of cognitive functions. Until recently, this was blamed on lack of estrogen, progesterone and testosterone brought about by menopause.
A study was done using a battery of tests of neurological functions in postmenopausal women and found that those with elevated homocysteine suffered the greatest percentage of cognitive decline. Here is the study author’s conclusion:
“In summary, hyperhomocysteinemia was related with increased risk of decline in executive functioning, complex attention, cognitive flexibility, and memory in postmenopausal women.”24
Record Number of Centenarians
According to the Centers for Disease Control and Prevention, the number of people in the United States age 100 and older has increased by 43.6% since year 2000.25
Whether people are demented by the time they reach 100 years has a lot to do with their behavior in earlier years, and genetic factors.
A recent study on centenarians evaluated a number of parameters and found dementia to be associated with higher blood levels of homocysteine and proinflammatory factors like C-reactive protein.26
Both of these blood markers are modifiable, meaning they can be brought down to safer ranges.
Protection against Non-Alzheimer’s Dementia
A number of studies have sought to assess the effectiveness of nutrients like vitamin E (alpha tocopherol) and risk of dementia. Some studies indicate benefits to antioxidant nutrients while others fail to show a protective effect.
A study evaluated blood levels of vitamin A, vitamin E, and homocysteine in elderly persons with and without dementia. The findings showed decreased risk of non-Alzheimer’s dementia in those with higher blood levels of vitamins A and E and lower levels of homocysteine.27
Reference Ranges Need to be Revised
A deficiency of vitamin B12 alone can cause mild cognitive impairment (and dementia).
A study looked at blood (serum) concentrations of vitamin B12 in a group of people suffering typical age-related neurological dysfunctions.
The findings showed that people with vitamin B12 in the “low” normal reference ranges showed significantly poorer learning ability and performance than did patients with “high” normal vitamin B12 status.28
The implications from this study are that reference ranges need to be amended so that today’s “low normal” B12 results are redefined as “deficient.”
Of interest are results of standard B12 blood tests that some of our supporters get. They often show B12 levels far above “normal” reference ranges. We get calls from people asking if they are taking too much vitamin B12. Our response is that virtually all of our customers have these higher B12 readings and this may be a good indicator of optimal B12 status.
Even Fetuses Need Protection
A number of previous studies associate prenatal maternal folate deficiency with reduced prenatal brain growth in offspring. Little is known about the longer-term impact.
A study of Dutch children aged 6-8 years was done utilizing MRI brain scans and other measures of intelligence. Children of mothers with insufficient folate showed poorer performance on language and visuospatial scores. The authors concluded:
“Our findings suggest that folate insufficiency in early pregnancy has a long-lasting, global effect on brain development and is, together with homocysteine levels, associated with poorer cognitive performance.”29
Young Adults may Benefit From B Vitamins

A study of people aged 18-40 years was done to compare the effects of a multivitamin supplement on mood.
In response to the multivitamin, homocysteine levels dropped significantly with a corresponding improvement in mood as measured by a recognized score of mental depression.30
Younger people respond well to standard B vitamins because their enzymatic conversion systems function at a high level, meaning they readily convert folate into 5-MTHF.
As people age, their ability to absorb and enzymatically metabolize folic acid is compromised, which is why homocysteine levels surge higher with age. The solution is to use the 5-MTHF form of folate that requires no enzymatic conversion to reduce homocysteine.
What are “High” Homocysteine Levels?
When Life Extension® evaluated homocysteine toxicity in the mid-1990s, we found persuasive evidence that optimal levels were below 8 µmol/L of blood.
The medical establishment has never been able to agree on what a “safe” homocysteine level really is, and there are many contradictory findings in the published literature.
Research has demonstrated that homocysteine levels above 10 µmol/L are associated with increased heart-attack risk.31 Another study showed an increased cardiac risk with homocysteine levels above 9 µmol/L and that the risk increased sharply as levels rise to 15 µmol/L or greater.32
A recent study found that homocysteine levels higher than 15 µmol/L were associated with almost double the prevalence of dementia, along with cognitive and functional impairment.33
These variations are commonly found across the different published studies and explain why conventional medicine has not been able to reach a consensus as to what optimal homocysteine levels should be.
From a practical standpoint, many aging individuals will be challenged to bring their homocysteine levels to below 8 µmol/L because of impaired B vitamin-dependent detoxification systems. That does not mean, however, that there is not a significant benefit to lowering homocysteine to, let’s say, below 12 µmol/L, as opposed to letting it stay at 15 µmol/L or higher.
Impact of Homocysteine on Cardiac-Stenting Patients
In response to narrowing or blockage of a coronary artery, most patients today have a metal stent inserted into the occluded artery to restore blood flow to the affected heart muscle. This eliminates the need for open-chest coronary bypass surgery and its many complications.
The concern is how long the stenting of one or multiple arteries will last and whether there will be long term cardiovascular problems.
A study was done on patients who underwent coronary-artery stenting to investigate whether elevated homocysteine at admission predicted long-term outcomes.
The subjects were divided into a group whose homocysteine blood levels were under 12 µmol/L compared to those 12 µmol/L and over.
After a mean follow-up of almost five years, rates of major adverse cardiac events were 30% higher in the group whose homocysteine was 12 µmol/L and above compared to those whose homocysteine was under 12 µmol/L.34
The most striking variable was cardiac death. Stent patients with homocysteine of 12 µmol/L and above were more than twice as likely to die from cardiac death over the study period compared to those whose admission homocysteine readings were below 12 µmol/L.
Homocysteine Blood Testing
 |
One reason we initiated direct-to-consumer testing 20 years ago was that many doctors refused to prescribe homocysteine blood tests when our members requested them.
We thought this to be highly inappropriate, considering there was no risk to someone merely checking their homocysteine blood levels. We are confident that our offering homocysteine blood tests saved lives based on surprisingly high levels that some people have and are able to lower by taking more B vitamins.
If you have not had your homocysteine checked recently, you can order it today and have your blood drawn at your convenience at a blood-draw station near you.
Our regular discount price to test homocysteine levels is $54, but if you order before August 31, 2017, we will include our CBC/Chemistry blood panel at no charge ($35 value). Page 15 itemizes the many important tests included in our CBC/Chemistry panel.
To order a homocysteine blood test for $54 and receive a complimentary CBC/Chemistry panel, call 1-800-208-3444 or log on to LifeExtension.com/homocysteine
Erectile Dysfunction
An early sign of vascular disease in men can be erectile dysfunction, which is the topic of endless television advertisements promoting expensive drugs like Cialis® and Viagra®.
A study comparing men with erectile dysfunction with controls found significantly reduced penile blood flow velocity in men with homocysteine levels above 12.65 µmol/L. This led the researchers to suggest that “elevation of homocysteine levels was associated with an increased risk of ED.”35
Stroke Induced by Homocysteine
A number of studies have looked at homocysteine blood levels and stroke, with inconsistent findings reported.
One reason is that the many independent risk factors for stroke (such as hypertension, glucose, inflammation, and lipids) make it difficult to pinpoint homocysteine as a specific independent causation factor.
A study published at the end of 2016 looked at stroke patients treated with the clot-busting drug tPA and found poorer outcomes in acute stroke patients with high homocysteine.
A striking finding from this study was that mean homocysteine levels in these ischemic stroke cases was 22.62 µmol/L, which is high by everyone’s standards.36
Yet most doctors today are not checking their elderly patients’ homocysteine blood levels, leaving a correctable risk factor unmeasured that is of importance to older people.
Individual Variation of Blood-Homocysteine Levels

Life Extension informs readers of novel methods to counteract age-related diseases that are overlooked by the medical mainstream.
We gauge efficacy based on peer-reviewed published findings, along with real-world interactions with physicians and our loyal supporters.
Over the past 37 years, we’ve reviewed thousands of homocysteine blood-test results and observed a wide variation.
Some people with healthy detoxification systems present with low homocysteine (under 8 µmol/L), while other similarly situated individuals have strikingly higher levels.
Folic acid and vitamin B12 detoxify homocysteine via the “methylation”37 pathway, whereas vitamin B6 detoxifies homocysteine via the “transsulfuration”38 pathway. Activated forms of these vitamins (such as 5-MTHF, methylcobalamin, and pyridoxal-5-phosphate) provide direct maintenance of these two homocysteine-detoxification pathways.
As humans age, homocysteine levels tend to rise, necessitating more aggressive use of proven homocysteine-lowering nutrients.
Many of you have recently had your homocysteine levels tested and can easily see where your level is.
If you have used our convenient blood-testing service, we keep your records on file back to year 2012. To receive a free copy of your blood results, call 1-800-208-3444 or send us an email to customer service@lifeextension.com
No More Need for Prescription B Vitamins
Nearly two decades ago, pharmaceutical companies obtained patents for B-vitamin formulas that contained the metabolically active 5-MTHF form of folate.
These prescription drug B-vitamin formulas are still sold at prices that exceed $200 a month. Now that patents have expired, consumers have access to superior formulas that provide high-potency 5-MTHF along with bioactive forms of vitamins B6 and B12 for a fraction of the prescription-drug price.
A large number of adults suffer the toxic effects of high homocysteine, which steadily increases as a consequence of normal aging.
If your homocysteine levels are higher than optimal, which we opine is any blood reading significantly greater than 8 µmol/L, please consider using the appropriate B vitamins to reduce it to safer ranges.
As we’ve advocated for the past four decades, reducing excess homocysteine will likely result in substantive public-health benefits in elderly population groups.
For longer life,
William Faloon,
Co-Founder, Life Extension®
References
- McCully KS. Homocysteine, vitamins, and prevention of vascular disease. Mil Med. 2004;169(4):325-9.
- ikonomidi A, Lewczuk P, Kornhuber J, et al. Homocysteine metabolism is associated with cerebrospinal fluid levels of soluble amyloid precursor protein and amyloid beta. J Neurochem. 2016;139(2):324-32.
- Smith AD, Refsum H. Homocysteine, B Vitamins, and Cognitive Impairment. Annu Rev Nutr. 2016;36:211-39.
- Dam K, Fuchtemeier M, Farr TD, et al. Increased homocysteine levels impair reference memory and reduce cortical levels of acetylcholine in a mouse model of vascular cognitive impairment. Behav Brain Res. 2017;321:201-8.
- Jerneren F, Elshorbagy AK, Oulhaj A, et al. Brain atrophy in cognitively impaired elderly: the importance of long-chain omega-3 fatty acids and B vitamin status in a randomized controlled trial. Am J Clin Nutr. 2015;102(1):215-21.
- ulhaj A, Jerneren F, Refsum H, et al. Omega-3 Fatty Acid Status Enhances the Prevention of Cognitive Decline by B Vitamins in Mild Cognitive Impairment. J Alzheimers Dis. 2016;50(2):547-57.
- Caruso R, Campolo J, Sedda V, et al. Effect of homocysteine lowering by 5-methyltetrahydrofolate on redox status in hyperhomocysteinemia. J Cardiovasc Pharmacol. 2006;47(4):549-55.
- Venn BJ, Green TJ, Moser R, et al. Comparison of the effect of low-dose supplementation with L-5-methyltetrahydrofolate or folic acid on plasma homocysteine: a randomized placebo-controlled study. Am J Clin Nutr. 2003;77(3):658-62.
- Available at: http://www.lifeextension.com/Magazine/2017/1/As-We-See-It/Page-01. Accessed May 15, 2017.
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983-8.
- Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857-67.
- Available at: http://secure.medicalletter.org/w1492a. Accessed May 15, 2017.
- Spence JD. Homocysteine-lowering therapy: a role in stroke prevention? Lancet Neurol. 2007;6(9):830-8.
- Selhub J, Jacques PF, Wilson PW, et al. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. Jama. 1993;270(22):2693-8.
- Selhub J. The many facets of hyperhomocysteinemia: studies from the Framingham cohorts. J Nutr. 2006;136(6 Suppl):1726s-30s.
- Xie Y, Feng H, Peng S, et al. Association of plasma homocysteine, vitamin B12 and folate levels with cognitive function in Parkinson’s disease: A meta-analysis. Neurosci Lett. 2017;636:190-5.
- Prinz-Langenohl R, Bramswig S, Tobolski O, et al. [6S]-5-methyltetrahydrofolate increases plasma folate more effectively than folic acid in women with the homozygous or wild-type 677C-->T polymorphism of methylenetetrahydrofolate reductase. Br J Pharmacol. 2009;158(8):2014-21.
- Jacques PF, Bostom AG, Williams RR, et al. Relation between folate status, a common mutation in methylenetetrahydrofolate reductase, and plasma homocysteine concentrations. Circulation. 1996;93(1):7-9.
- McLean RR, Jacques PF, Selhub J, et al. Homocysteine as a predictive factor for hip fracture in older persons. N Engl J Med. 2004;350(20):2042-9.
- Li P, Qin C. Methylenetetrahydrofolate reductase (MTHFR) gene polymorphisms and susceptibility to ischemic stroke: a meta-analysis. Gene. 2014;535(2):359-64.
- Abd El-Aziz TA, Mohamed RH. Influence of MTHFR C677T gene polymorphism in the development of cardiovascular disease in Egyptian patients with rheumatoid arthritis. Gene. 2017;610:127-32.
- Moll S, Varga EA. Homocysteine and MTHFR Mutations. Circulation. 2015;132(1):e6-e9.
- Rathod R, Kale A, Joshi S. Novel insights into the effect of vitamin B(1)(2) and omega-3 fatty acids on brain function. J Biomed Sci. 2016;23:17.
- Raszewski G, Loroch M, Owoc A, et al. Homocysteine and cognitive disorders of postmenopausal women measured by a battery of computer tests--central nervous system vital signs. Arch Womens Ment Health. 2015;18(4):623-30.
- “Mortality Among Centenarians in the United States 2000-2014”; Centers for Disease Control and Prevention; January/July 2016. Available at: https://www.cdc.gov/nchs/data/databriefs/db233.pdf. Accessed May 16, 2017.
- Duarte PO, Duarte MG, Pelichek A, et al. Cardiovascular risk factors and inflammatory activity among centenarians with and without dementia. Aging Clin Exp Res. 2016.
- Raszewski G, Chwedorowicz R, Chwedorowicz A, et al. Homocysteine, antioxidant vitamins and lipids as biomarkers of neurodegeneration in Alzheimer’s disease versus non-Alzheimer’s dementia. Ann Agric Environ Med. 2016;23(1):193-6.
- Kobe T, Witte AV, Schnelle A, et al. Vitamin B-12 concentration, memory performance, and hippocampal structure in patients with mild cognitive impairment. Am J Clin Nutr. 2016;103(4):1045-54.
- Ars CL, Nijs IM, Marroun HE, et al. Prenatal folate, homocysteine and vitamin B12 levels and child brain volumes, cognitive development and psychological functioning: the Generation R Study. Br J Nutr. 2016:1-9.
- White DJ, Cox KH, Peters R, et al. Effects of Four-Week Supplementation with a Multi-Vitamin/Mineral Preparation on Mood and Blood Biomarkers in Young Adults: A Randomised, Double-Blind, Placebo-Controlled Trial. Nutrients. 2015;7(11):9005-17.
- Stampfer MJ, Malinow MR, Willett WC, et al. A prospective study of plasma homocyst(e)ine and risk of myocardial infarction in US physicians. Jama. 1992;268(7):877-81.
- Nygard O, Nordrehaug JE, Refsum H, et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997;337(4):230-6.
- Bonetti F, Brombo G, Magon S, et al. Cognitive Status According to Homocysteine and B-Group Vitamins in Elderly Adults. J Am Geriatr Soc. 2015;63(6):1158-63.
- Yeh JK, Chen CC, Hsieh MJ, et al. Impact of Homocysteine Level on Long-term Cardiovascular Outcomes in Patients after Coronary Artery Stenting. J Atheroscler Thromb. 2016.
- Zhang Z, Xu Z, Dai Y, et al. Elevated serum homocysteine level as an independent risk factor for erectile dysfunction: a prospective pilot case-control study. Andrologia. 2016.
- Yao ES, Tang Y, Xie MJ, et al. Elevated Homocysteine Level Related to Poor Outcome After Thrombolysis in Acute Ischemic Stroke. Med Sci Monit. 2016;22:3268-73.
- Brosnan JT, Jacobs RL, Stead LM, et al. Methylation demand: a key determinant of homocysteine metabolism. Acta Biochim Pol. 2004;51(2):405-13.
- Selhub J. Homocysteine metabolism. Annu Rev Nutr. 1999;19:217-46.

