Life Extension Magazine®
The Centers for Disease Control and Prevention say that more than 1 in 3 American adults have blood sugar levels that are too high.1
The condition they are referring to is prediabetes. It occurs when blood sugar markers are elevated, but have not yet reached the diabetic threshold.
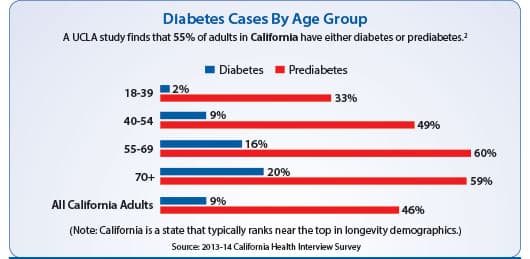
In 2016, UCLA reported that 46% of California adults are either prediabetic or have undiagnosed type II diabetes.2 The severity of this health crisis cannot be overstated.
Diabetic pathologies develop during the prediabetic phase.3 So by the time type II diabetes manifests, patients already confront complications that include kidney impairment,4,5 vision loss,6-8 neuropathy,9 atherosclerosis,10-12 and cancer.13-15
Despite these risks, populations around the world increasingly gorge on deadly foods/drinks that spike blood sugar levels. Not only does this increase disease risk, it accelerates aging by shortening telomeres.16,17
We at Life Extension® have warned of this catastrophic epidemic since the early 1980s. Back in those days, what authorities now recognize as dangerously high glucose levels were considered safe by the medical mainstream.
An abundance of published findings support our recommendation to keep blood sugar at the low end of the normal reference range.18-21
Despite these conclusive data, the medical community has failed to wake up to the life-shortening impact of prediabetes. It is thus up to individuals to take charge and make the appropriate adjustments.
There are a variety of methods to maintain healthier glucose levels. It all begins with proper blood testing.
Standard blood tests often miss identifying early-stage prediabetes and diabetes. That’s because the last marker to elevate in patients with poor glycemic control is often fasting glucose.
The reason for this is that blood sugar problems in the early stages can be covered up by excess secretion of insulin from the pancreas.
As long as there is a reasonable degree of cellular insulin sensitivity and loads of insulin being produced, a fasting glucose blood test may appear in a safe range, which by today’s standards is under 100 mg/dL.
What few understand is that excess insulin contributes to disease states even before fasting glucose raises to prediabetic levels. Doctors suspect prediabetes when fasting glucose is in the range of 100 to 125 mg/dL.
Life Extension vehemently disagrees with conventional medicine and advocates people strive to achieve fasting glucose below 86 mg/dL. We know this is not always possible, but we want our readers to know what optimal glucose levels are based on science as opposed to obsolete “reference ranges.”
More Accurate Blood Test

The hemoglobin A1c blood test provides a better picture of glycemic control than fasting glucose.22 It is the standard used by doctors to ascertain the efficacy of various treatments for type II diabetes, but it is underutilized in identifying prediabetes.
The safe upper limit for hemoglobin A1c is 5.6%, though lower ranges have been shown to be healthier.23
The American Diabetes Association says if your hemoglobin A1c is 5.7%-6.4%, you have prediabetes.24 This nonprofit group recommends metformin for prevention of type II diabetes in people with hemoglobin A1c levels of 5.7%-6.4%.25
Metformin enhances insulin sensitivity and functions via several mechanisms to improve glycemic control.26-30 The ability of metformin to delay or prevent onset of diabetes has been proven in large, well-designed, randomized clinical trials.31-35
Yet recent surveys reveal a shocking shortfall in the prescribing of metformin. Studies published in 2015 show that metformin was only prescribed to 3.7% to 8.1% of prediabetics.35-37
I hope you can relate to my outrage over this! We at Life Extension have urged healthy individuals to boost cellular AMPK activity to protect against degenerative aging. We listed metformin (which activates AMPK) as an anti-aging drug beginning in 1995.
The fact that more than 90% of prediabetics are not prescribed metformin represents medical malpractice in our opinion. It provides a stark example of why health-conscious people need to take matters into their own hands, order their own blood tests, and embark on a glycemic control program if need be, in coordination with a progressive physician.
Glucose Levels in Calorie Restrictors
 |
Calorie restriction remains an important standard by which longevity factors can be measured.79-82
Those who practice calorie restriction often achieve very low blood glucose levels.83-85
In a study group of people who drastically reduced their food intake, fasting glucose declined to an average of 74 mg/dL.83
This corresponds to animal studies in which caloric restriction induced significant reductions in blood glucose in conjunction with dramatic increases in lifespan.86-88
These studies provide a strong incentive to keep glucose in the low normal range.
Deadly Impact of Prediabetes
Even modestly elevated glucose levels inflict microvascular damage that resembles the long-term complications of type II diabetes.38,39
Excess glucose converts in the body to triglycerides that are stored as fat and contribute to atherosclerosis.40-42
A myriad of published studies shows that even high normal blood sugar levels increase risk of degenerative disorders.4-15,20,43-51
Researchers have been startled by data showing higher rates of diseases that were not previously associated with glucose, such as dementia and cancer.52-55
Those with glucose above 85 mg/dL are at increased risk of heart attack.18 This was shown in a study of nearly 2,000 men where fasting blood glucose levels were measured over a 22-year period. The results showed that men with fasting glucose over 85 mg/dL had a 40% increased risk of death from cardiovascular disease. These researchers stated:
“Fasting blood glucose values in the upper normal range appears to be an important independent predictor of cardiovascular death in nondiabetic apparently healthy middle-aged men.”18
Studies show that after-meal glucose levels are an even stronger predictor of disease risk.56-58 This is why we advocate that most people now consider having their blood drawn after a normal meal.
Prediabetes Should Be Classified as Diabetes
The term prediabetes is both an accurate and misleading term.
About 70% of prediabetics will develop type II diabetes in their lifetime.59,60 So if one wants to construe prediabetes as a state that exists before type II diabetes is diagnosed, that is accurate.
What is misleading is thinking that prediabetes means before diabetic damage is inflicted. Quite the opposite is true. During the prediabetic period, tremendous microvascular injury occurs that can lead to kidney failure,61,62 blindness,6-8 stroke,63 and heart disease.19,20,49
We at Life Extension have long argued that any level of excess glucose predisposes to greater disease risk and therefore should be classified as type II diabetes.
When human lifespans were shorter, our opposition argued that aging people with slightly elevated blood glucose were likely to perish from some other cause. That was a false assumption back then and certainly not true today when age reversal technology is being aggressively pursued.
A vivid example of why there may be no difference in prediabetes versus type II diabetes can be seen in a study involving 1,800 people over a 10-year period.49 This study found that coronary heart disease risk was similar between prediabetics and type II diabetics. The authors commented that impaired fasting glucose significantly increased coronary risk in comparison with the normal glucose group. The researchers concluded:
“Early control of blood glucose is essential to prevention and control of CHD [coronary heart disease].”49
One advantage of detecting prediabetes early is there is a greater likelihood of reversing it before it progresses to type II diabetes. Until physicians start taking the lead in aggressively treating even high normal glucose levels, large numbers of aging Americans will prematurely suffer horrific degenerative conditions from blood sugar levels that could have been prevented.
Doctors should not wait until fasting glucose exceeds 125 mg/dL or hemoglobin A1c reaches 6.5% before initiating treatment. They should initiate glucose-lowering approaches when fasting glucose exceeds 85 mg/dL or hemoglobin A1c exceeds 5.5%.
Lung Cancer and Sugar

Lung cancer remains the leading cause of cancer death, and you don’t have to smoke to contract it.64 Cure rates remain abysmally low, though newer immune-modulating drugs are enabling some patients to survive longer.65
Researchers at the University of Texas MD Anderson Cancer Center analyzed the dietary habits and health history of over 4,000 people. Those who ingested a high glycemic diet had 49% increased odds of having lung cancer regardless of smoking habits compared to those with the lowest glycemic diet.66
For nonsmokers in this study, the odds of having lung cancer were more than double in those who ingested a high glycemic index diet compared to those with the lowest glycemic index diet. Foods that rank high on the glycemic scale include starches like white bread and rice along with any sugar/starch laden food/drink that spikes after-meal glucose levels.
Up to 25% of people who contract lung cancer don’t smoke.67,68 Many of these individuals would never touch a cigarette because of cancer risk, yet don’t know that high blood glucose is also a major risk factor.
Glucose provides fuel for rapidly dividing cancer cells, while insulin is a hormonal stimulator for cellular proliferation.69-73 Those who consume high glycemic diets sharply increase their odds of contracting many forms of cancer,74-76 yet the public remains largely unaware.
High Glucose Shrinks Your Brain!
 |
More than 1 in 3 adults have glucose levels that put them at increased risk of heart disease, stroke, dementia, and cancer.49,91-93
Recent findings show blood glucose at the high end of normal resulted in significant brain shrinkage, particularly in the regions of the brain (hippocampus and amygdala) involved in memory and other critical functions.94
Reducing ingestion of simple sugars and starches helps control blood sugar levels.
The key to optimal glucose control is to cut back on calories, increase physical activities, and utilize nutrients/drugs that inhibit absorption of ingested carbohydrates, suppress glucose production in the liver, and improve glucose utilization in tissues via enhanced insulin sensitivity.
Normal Blood Sugar Levels Increase Breast Cancer Risk
Life Extension researchers conducted an analysis of the scientific literature to ascertain if there was a connection between higher “normal” blood glucose and breast cancer risk. Our analysis revealed compelling data suggesting increased breast cancer risk amongst women with so-called “normal” blood glucose levels.
One study found that premenopausal women with fasting blood sugar above 84 mg/dL had more than two-times the risk of developing breast cancer compared to those with lower levels.44
Another study compared women with fasting glucose under 100 mg/dL to those whose blood glucose was between 100-125 mg/dL. Women with the higher glucose readings had a 23% increased risk of breast cancer after multivariate analysis.77
A study of over 10,000 women in Italy found those in the highest glucose quartile (median 96 mg/dL) had a 63% increased risk for breast cancer compared to those in the lowest quartile (median 73 mg/dL) after being “fully adjusted” for multiple variables. The authors stated in the discussion:
“…we found that elevated fasting glucose levels were significantly associated with subsequent occurrence of BC [breast cancer]. The association was significant both in pre and postmenopausal women.”78
Note that studies showing the greatest increase in breast cancer risk occur when glucose levels exceed midrange normal levels. These consistent findings are published in medical journals, yet most practicing physicians do not treat blood sugar until readings exceed 125 mg/dL!
For breast cancer risk reduction, keep glucose at the lowest normal range that appears optimal.
Know Your Glucose and Hemoglobin A1c
The amount of sugars and starches consumed in the modern world exceeds the body’s capacity to utilize the excess blood glucose they produce. As people age, their glycemic regulatory controls often fail. Surveys reveal many adults suffer dangerously high glucose levels.89,90
Readers of this magazine take nutrients that help lower glycemic markers and protect against glucose-induced toxicities.
It is imperative, however, that health conscious individuals have proper blood tests to ensure they are not anywhere close to a prediabetic state. While some in the mainstream are finally treating patients with glucose between 100-125 mg/dL (prediabetic), we at Life Extension continue to urge far lower glucose levels for optimal health and longevity.
Once a year we offer a comprehensive panel of blood tests at the discounted price of $199. Commercial labs charge higher prices and oftenfail to include blood biomarkers such as C-reactive protein, homocysteine, hemoglobin A1c, lipids, and hormones that all represent manageable longevity factors.
I hope you will have these blood tests performed to enable risk factors to be reversed before it results in permanent illness.
Turn this page to see the many blood tests included in the popular Male and Female Panels.
References
- Available at: https://www.cdc.gov/features/diabetesfactsheet. Accessed March 16, 2017.
- Babey SH, Wolstein J, Diamant AL, et al. Prediabetes in California: Nearly Half of California Adults on Path to Diabetes. Policy Brief UCLA Cent Health Policy Res. 2016(Pb2016-1):1-8.
- Tabak AG, Herder C, Rathmann W, et al. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279-90.
- Plantinga LC, Crews DC, Coresh J, et al. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clin J Am Soc Nephrol. 2010;5(4):673-82.
- Hoehner CM, Greenlund KJ, Rith-Najarian S, et al. Association of the insulin resistance syndrome and microalbuminuria among nondiabetic native Americans. The Inter-Tribal Heart Project. J Am Soc Nephrol. 2002;13(6):1626-34.
- Gabir MM, Hanson RL, Dabelea D, et al. Plasma glucose and prediction of microvascular disease and mortality: evaluation of 1997 American Diabetes Association and 1999 World Health Organization criteria for diagnosis of diabetes. Diabetes Care. 2000;23(8):1113-8.
- Algvere P, Efendic S, Luft R, et al. Retinal microangiopathy and pigment epithelial lesions in subjects with normal, borderline, and decreased oral glucose tolerance. Br J Ophthalmol. 1985;69(6):416-9.
- Tapp RJ, Tikellis G, Wong TY, et al. Longitudinal association of glucose metabolism with retinopathy: results from the Australian Diabetes Obesity and Lifestyle (AusDiab) study. Diabetes Care. 2008;31(7):1349-54.
- Sumner CJ, Sheth S, Griffin JW, et al. The spectrum of neuropathy in diabetes and impaired glucose tolerance. Neurology. 2003;60(1):108-11.
- Redgrave JN, Lovett JK, Syed AB, et al. Histological features of symptomatic carotid plaques in patients with impaired glucose tolerance and diabetes (oxford plaque study). Cerebrovasc Dis. 2008;26(1):79-86.
- Kurihara O, Takano M, Yamamoto M, et al. Impact of prediabetic status on coronary atherosclerosis: a multivessel angioscopic study. Diabetes Care. 2013;36(3):729-33.
- Kramer D, Raji A, Plutzky J. Prediabetes mellitus and its links to atherosclerosis. Curr Diab Rep. 2003;3(1):11-8.
- Huang Y, Cai X, Qiu M, et al. Prediabetes and the risk of cancer: a meta-analysis. Diabetologia. 2014;57(11):2261-9.
- Salinas-Martinez AM, Flores-Cortes LI, Cardona-Chavarria JM, et al. Prediabetes, diabetes, and risk of breast cancer: a case-control study. Arch Med Res. 2014;45(5):432-8.
- Onitilo AA, Stankowski RV, Berg RL, et al. Breast cancer incidence before and after diagnosis of type 2 diabetes mellitus in women: increased risk in the prediabetes phase. Eur J Cancer Prev. 2014;23(2):76-83.
- Leung CW, Laraia BA, Needham BL, et al. Soda and cell aging: associations between sugar-sweetened beverage consumption and leukocyte telomere length in healthy adults from the National Health and Nutrition Examination Surveys. Am J Public Health. 2014;104(12):2425-31.
- Adaikalakoteswari A, Balasubramanyam M, Ravikumar R, et al. Association of telomere shortening with impaired glucose tolerance and diabetic macroangiopathy. Atherosclerosis. 2007;195(1):83-9.
- Bjornholt JV, Erikssen G, Aaser E, et al. Fasting blood glucose: an underestimated risk factor for cardiovascular death. Results from a 22-year follow-up of healthy nondiabetic men. Diabetes Care. 1999;22(1):45-9.
- Selvin E, Coresh J, Golden SH, et al. Glycemic control and coronary heart disease risk in persons with and without diabetes: the atherosclerosis risk in communities study. Arch Intern Med. 2005;165(16):1910-6.
- Levitan EB, Song Y, Ford ES, et al. Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med. 2004;164(19):2147-55.
- Held C, Gerstein HC, Yusuf S, et al. Glucose levels predict hospitalization for congestive heart failure in patients at high cardiovascular risk. Circulation. 2007;115(11):1371-5.
- Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362(9):800-11.
- Matsushita K, Blecker S, Pazin-Filho A, et al. The association of hemoglobin a1c with incident heart failure among people without diabetes: the atherosclerosis risk in communities study. Diabetes. 2010;59(8):2020-6.
- Available at: http://www.diabetesforecast.org/2010/jan/new-guidelines-aim-to-help-doctors-achieve-better-diabetes-care.html. Accessed March 20, 2017.
- Standards of Medical Care in Diabetes—2014. Diabetes Care. 2014;37(Supplement 1):S14-S80.
- Giannarelli R, Aragona M, Coppelli A, et al. Reducing insulin resistance with metformin: the evidence today. Diabetes Metab. 2003;29(4 Pt 2):6s28-35.
- Malin SK, Gerber R, Chipkin SR, et al. Independent and combined effects of exercise training and metformin on insulin sensitivity in individuals with prediabetes. Diabetes Care. 2012;35(1):131-6.
- Hundal RS, Krssak M, Dufour S, et al. Mechanism by which metformin reduces glucose production in type 2 diabetes. Diabetes. 2000;49(12):2063-9.
- Caton PW, Nayuni NK, Kieswich J, et al. Metformin suppresses hepatic gluconeogenesis through induction of SIRT1 and GCN5. J Endocrinol. 2010;205(1):97-106.
- Hostalek U, Gwilt M, Hildemann S. Therapeutic Use of Metformin in Prediabetes and Diabetes Prevention. Drugs. 2015;75(10):1071-94.
- Available at: https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp/pages/default.aspx. Accessed March 20, 2017.
- Available at: http://www.diabetes.org/newsroom/press-releases/2014/long-term-follow-up-of-diabetes-prevention-program-shows-reduction-in-diabetes-development.html. Accessed March 20, 2017.
- Lily M, Godwin M. Treating prediabetes with metformin: systematic review and meta-analysis. Can Fam Physician. 2009;55(4):363-9.
- Salpeter SR, Buckley NS, Kahn JA, et al. Meta-analysis: metformin treatment in persons at risk for diabetes mellitus. Am J Med. 2008;121(2):149-57.e2.
- Moin T, Li J, Duru OK, et al. Metformin prescription for insured adults with prediabetes from 2010 to 2012: a retrospective cohort study. Ann Intern Med. 2015;162(8):542-8.
- Stirling DL, Onor I, Sarpong D, et al. Prescribing Patterns of Metformin in High-risk Patients with Prediabetes. J La State Med Soc. 2015;167(6):257-62.
- Goldberg T, Kroehl ME, Suddarth KH, et al. Variations in Metformin Prescribing for Type 2 Diabetes. J Am Board Fam Med. 2015;28(6):777-84.
- Milman S, Crandall JP. Mechanisms of vascular complications in prediabetes. Med Clin North Am. 2011;95(2):309-25, vii.
- Sprague RS, Ellsworth ML. Vascular disease in pre-diabetes: new insights derived from systems biology. Mo Med. 2010;107(4):265-9.
- Ebenbichler CF, Kirchmair R, Egger C, et al. Postprandial state and atherosclerosis. Curr Opin Lipidol. 1995;6(5):286-90.
- Jacobson TA, Miller M, Schaefer EJ. Hypertriglyceridemia and cardiovascular risk reduction. Clin Ther. 2007;29(5): 763-77.
- Welin L, Eriksson H, Larsson B, et al. Triglycerides, a major coronary risk factor in elderly men. A study of men born in 1913. Eur Heart J. 1991;12(6):700-4.
- Stattin P, Bjor O, Ferrari P, et al. Prospective study of hyperglycemia and cancer risk. Diabetes Care. 2007;30(3):561-7.
- Muti P, Quattrin T, Grant BJ, et al. Fasting glucose is a risk factor for breast cancer: a prospective study. Cancer Epidemiol Biomarkers Prev. 2002;11(11):1361-8.
- Cust AE, Kaaks R, Friedenreich C, et al. Metabolic syndrome, plasma lipid, lipoprotein and glucose levels, and endometrial cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Endocr Relat Cancer. 2007;14(3):755-67.
- Schoen RE, Tangen CM, Kuller LH, et al. Increased blood glucose and insulin, body size, and incident colorectal cancer. J Natl Cancer Inst. 1999;91(13):1147-54.
- Coutinho M, Gerstein HC, Wang Y, et al. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care. 1999;22(2):233-40.
- Lamblin N, Cuvelier E, Gonin X, et al. Abstract 2372: Hemoglobin A1c Levels are Associated with Severity and Prognosis of Systolic Chronic Heart Failure in Non Diabetic Patients. Circulation. 2006;114(Suppl 18):II_486-II_7.
- Li Q, Chen AH, Song XD, et al. Analysis of glucose levels and the risk for coronary heart disease in elderly patients in Guangzhou Haizhu district. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30(6):1275-8.
- Pereg D, Elis A, Neuman Y, et al. Cardiovascular risk in patients with fasting blood glucose levels within normal range. Am J Cardiol. 2010;106(11):1602-5.
- Bitra VR, Rapaka D, Akula A. Prediabetes and Alzheimer’s Disease. Indian J Pharm Sci. 2015;77(5):511-4.
- Available at: https://www.lifeextension.com/magazine/2014/ce/ce_when-will-doctors-recognize-this-leading-cause-of-death/page-01. Accessed March 20, 2017.
- Available at: https://www.lifeextension.com/magazine/2013/2/elevated-glucose-increases-incidence-of-breast-cancer-and-brain-shrinkage/page-01. Accessed March 20, 2017.
- Available at: https://www.lifeextension.com/magazine/2012/2/doctors-overlook-leading-cause-premature-death/page-01. Accessed March 20, 2017.
- Available at: https://www.lifeextension.com/magazine/2012/2/proven-methods-reduce-fasting-postprandial-glucose-levels/page-01. Accessed March 20, 2017.
- Moebus S, Gores L, Losch C, et al. Impact of time since last caloric intake on blood glucose levels. Eur J Epidemiol. 2011;26(9):719-28.
- Onat A, Can G, Cicek G, et al. Fasting, non-fasting glucose and HDL dysfunction in risk of pre-diabetes, diabetes, and coronary disease in non-diabetic adults. Acta Diabetol. 2013;50(4):519-28.
- Sacks DB. A1C versus glucose testing: a comparison. Diabetes Care. 2011;34(2):518-23.
- Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753-9.
- Eikenberg JD, Davy BM. Prediabetes: a prevalent and treatable, but often unrecognized, clinical condition. J Acad Nutr Diet. 2013;113(2):213-8.
- Melsom T, Schei J, Stefansson VT, et al. Prediabetes and Risk of Glomerular Hyperfiltration and Albuminuria in the General Nondiabetic Population: A Prospective Cohort Study. Am J Kidney Dis. 2016;67(6):841-50.
- Fox CS, Larson MG, Leip EP, et al. Glycemic status and development of kidney disease: the Framingham Heart Study. Diabetes Care. 2005;28(10):2436-40.
- Mijajlovic MD, Aleksic VM, Sternic NM, et al. Role of prediabetes in stroke. Neuropsychiatr Dis Treat. 2017;13:259-67.
- Available at: https://www.cdc.gov/cancer/lung. Accessed March 20, 2017.
- Massarelli E, Papadimitrakopoulou V, Welsh J, et al. Immunotherapy in lung cancer. Transl Lung Cancer Res. 2014;3(1):53-63.
- Melkonian SC, Daniel CR, Ye Y, et al. Glycemic Index, Glycemic Load, and Lung Cancer Risk in Non-Hispanic Whites. Cancer Epidemiol Biomarkers Prev. 2016;25(3):532-9.
- Couraud S, Zalcman G, Milleron B, et al. Lung cancer in never smokers--a review. Eur J Cancer. 2012;48(9):1299-311.
- Samet JM, Avila-Tang E, Boffetta P, et al. Lung cancer in never smokers: clinical epidemiology and environmental risk factors. Clin Cancer Res. 2009;15(18): 5626-45.
- Arcidiacono B, Iiritano S, Nocera A, et al. Insulin resistance and cancer risk: an overview of the pathogenetic mechanisms. Exp Diabetes Res. 2012;2012:789174.
- Dang CV. Links between metabolism and cancer. Genes Dev. 2012;26(9):877-90.
- Burnol AF, Morzyglod L, Popineau L. Cross-talk between insulin signaling and cell proliferation pathways. Ann Endocrinol (Paris). 2013;74(2):74-8.
- Koenuma M, Yamori T, Tsuruo T. Insulin and insulin-like growth factor 1 stimulate proliferation of metastatic variants of colon carcinoma 26. Jpn J Cancer Res. 1989;80(1):51-8.
- Perseghin G, Calori G, Lattuada G, et al. Insulin resistance/hyperinsulinemia and cancer mortality: the Cremona study at the 15th year of follow-up. Acta Diabetol. 2012;49(6):421-8.
- Sieri S, Krogh V, Agnoli C, et al. Dietary glycemic index and glycemic load and risk of colorectal cancer: results from the EPIC-Italy study. Int J Cancer. 2015;136(12):2923-31.
- Gnagnarella P, Gandini S, La Vecchia C, et al. Glycemic index, glycemic load, and cancer risk: a meta-analysis. Am J Clin Nutr. 2008;87(6):1793-801.
- Turati F, Galeone C, Gandini S, et al. High glycemic index and glycemic load are associated with moderately increased cancer risk. Mol Nutr Food Res. 2015;59(7):1384-94.
- Mink PJ, Shahar E, Rosamond WD, et al. Serum insulin and glucose levels and breast cancer incidence: the atherosclerosis risk in communities study. Am J Epidemiol. 2002;156(4):349-52.
- Sieri S, Muti P, Claudia A, et al. Prospective study on the role of glucose metabolism in breast cancer occurrence. Int J Cancer. 2012;130(4):921-9.
- Heilbronn LK, de Jonge L, Frisard MI, et al. Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: a randomized controlled trial. Jama. 2006;295(13): 1539-48.
- Lefevre M, Redman LM, Heilbronn LK, et al. Caloric restriction alone and with exercise improves CVD risk in healthy non-obese individuals. Atherosclerosis. 2009;203(1):206-13.
- Weindruch R. Effect of caloric restriction on age-associated cancers. Exp Gerontol. 1992;27(5-6):575-81.
- Colman RJ, Anderson RM, Johnson SC, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325(5937):201-4.
- Walford RL, Harris SB, Gunion MW. The calorically restricted low-fat nutrient-dense diet in Biosphere 2 significantly lowers blood glucose, total leukocyte count, cholesterol, and blood pressure in humans. Proc Natl Acad Sci U S A. 1992;89(23):11533-7.
- Kemnitz JW, Roecker EB, Weindruch R, et al. Dietary restriction increases insulin sensitivity and lowers blood glucose in rhesus monkeys. Am J Physiol. 1994;266(4 Pt 1):E540-7.
- Martins C, Morgan LM, Robertson MD. Effects of restrained eating behaviour on insulin sensitivity in normal-weight individuals. Physiol Behav. 2009;96(4-5):703-8.
- Bluher M, Kahn BB, Kahn CR. Extended longevity in mice lacking the insulin receptor in adipose tissue. Science. 2003;299(5606):572-4.
- Lane MA, Ingram DK, Roth GS. Calorie restriction in nonhuman primates: effects on diabetes and cardiovascular disease risk. Toxicol Sci. 1999;52(2 Suppl):41-8.
- Ugochukwu NH, Figgers CL. Modulation of the flux patterns in carbohydrate metabolism in the livers of streptozoticin-induced diabetic rats by dietary caloric restriction. Pharmacol Res. 2006;54(3):172-80.
- Available at: http://www.diabetes.org/diabetes-basics/statistics. Accessed March 20, 2017.
- Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31-40.
- Nichols GA, Hillier TA, Brown JB. Normal fasting plasma glucose and risk of type 2 diabetes diagnosis. Am J Med. 2008;121(6):519-24.
- Ott A, Stolk RP, van Harskamp F, et al. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999;53(9):1937-42.
- Volkers N. Diabetes and cancer: scientists search for a possible link. J Natl Cancer Inst. 2000;92(3):192-4.
- Cherbuin N, Sachdev P, Anstey KJ. Higher normal fasting plasma glucose is associated with hippocampal atrophy: The PATH Study. Neurology. 2012;79(10):1019-26.

