Life Extension Magazine®
People often think of bone loss as something that happens mostly to elderly women.
The reality is that more than half of adults over age 50 in the United States—including men—have bone loss or osteoporosis.1,2
Up to one-quarter of men over 50 will suffer an osteoporosis-related fracture. Men who suffer from a major fracture are more likely than women to die from the same injury.3
Poor bone health predisposes us to fractures. A bone fracture not only creates painful loss of mobility, but is also life-threatening.
In older adults with hip fractures who are bedridden, risk of pneumonia and formation of deadly clots skyrockets.4-6
Osteoporosis is associated with an increased risk of other age-related conditions, including cancer,7 atherosclerosis,8 dementia,9,10 and depression.11
This makes it essential for men and women to take active steps to prevent bone loss.
In addition to calcium and vitamin D, researchers have identified other key nutrients that promote bone formation, including magnesium, silicon, and boron.12-14
We need to be sure we’re getting these nutrients to optimize bone density—and overall health—as we age.
Calcium Stops Bone Loss

Most people associate calcium with bone health, and for good reason. Adequate calcium intake is needed for the proper mineralization, strength, and structure of bones.15 Despite this common knowledge, most Americans fail to get enough calcium in their diets.16
Studies show that supplementation with calcium (in the form of calcium citrate or calcium carbonate) makes a substantial difference in the rate at which bone breakdown and loss of minerals occurs.16-18
In multiple studies of early- and mid-postmenopausal women, supplementing with 800 mg-1,000 mg of calcium citrate daily was shown to effectively stop bone loss in the lower vertebrae and forearm, two common fracture sites in older adults. It also significantly improved bone density at other sites, including the hip and total body, compared to placebo recipients.19,20
Research has also shown that several markers of bone resorption, or breakdown, decreased in the patients supplementing with calcium citrate.21,22
A 2014 comparison study found that calcium citrate and calcium carbonate are effective in raising serum calcium levels and reducing markers of bone loss.23
Ample calcium intake is a prerequisite for good bone health, but bones are made of more than calcium. They rely on a variety of nutritional and lifestyle factors to support their health.
One key nutrient that works in conjunction with calcium is vitamin D.
Vitamin D’s Bone Health Benefits
Most people don’t get anywhere near the recommended intake of vitamin D.24
This is a major concern because vitamin D insufficiency (below 20 ng/mL) can accelerate osteoporosis, especially in aging men and women.25
Current recommendations are that people with vitamin D levels below 20 ng/mL should supplement with 800-1,000 IU/day, along with adequate calcium intake.25
Life Extension believes people should strive for precise individualized dosing (5,000-8,000 IU/day) to achieve optimal blood levels in the range of 50-80 ng/mL.
Vitamin D works hand-in-hand with calcium to reduce the risk of osteoporosis. It promotes intestinal absorption of calcium and helps direct how calcium is incorporated into bone.26,27 It also facilitates the transfer of calcium from the blood and other extracellular fluids to the surface of bones, where it makes them stronger and less likely to break.28 Vitamin D helps the body absorb zinc and manganese as well, which are trace elements essential for bone metabolism.29
A 2017 study demonstrated that three years of calcium and vitamin D supplementation powerfully influenced both the mineral and the organic protein matrix of bone.30
In a 2016 meta-analysis of eight studies involving nearly 31,000 subjects, supplementation with calcium plus vitamin D was found to reduce the risk of fractures. Together, these two nutrients produced a 15% reduction in the risk of any fracture, and a significant 30% reduction in the risk of hip fractures,31 which are so often the beginning of the end for frail, elderly people.
Calcium and vitamin D are especially important for people taking prescription drugs for osteoporosis.
One study found that up to 30% of those taking bone-protective bisphosphonate drugs did not respond well to treatment, which could be a result of low vitamin D levels. Non-responders tended to have low vitamin D and higher loss of a marker of bone loss.32
This study showed that people with vitamin D levels lower than 30 ng/ml were more than four times as likely to fail to respond to drug treatment for osteoporosis.32
Despite the consistency of these findings, many physicians who prescribe bisphosphonate drugs fail to supplement their patients with these critical nutrients.33,34
What You Need to Know
 |
Key Nutrients for Bone Health
- Osteoporosis is a growing problem in the aging population for both men and women.
- In addition to causing bone loss and increasing the risk for fractures, osteoporosis can lead to many other conditions.
- Osteoporosis is at least partially preventable by careful and appropriate use of nutritional supplements.
- While calcium and vitamin D remain the mainstays of bone nutrition, they cannot fully optimize bone health by themselves.
- Additional minerals are required for overall bone strength and mineralization, including magnesium, zinc, manganese, silicon, and boron.
- For the best bone-maintenance, osteoporosis-prevention program, it’s important to include the full profile of bone nutrients.
Magnesium Slows Bone Turnover
Magnesium is another essential component of the bone mineral matrix. About half of all magnesium in the body is stored in bone.35
It’s not surprising that animal studies show a positive correlation between magnesium intake and bone mineral density. Magnesium deficiency has been shown to reduce the number of osteoblasts (cells that build new bone) and increase the number of osteoclasts (cells that break down bone).35
The good news is that in animal models of post-menopause, restoring magnesium levels improved bone formation, reduced breakdown, and ultimately improved bone strength.35 Other studies have shown similar results in male animals as well.36,37
Human studies support these findings, demonstrating significant reductions in bone turnover rates—particularly in markers of bone resorption—in both men and women who took magnesium daily.38,39
Zinc Promotes New Bone Formation
Zinc is another key nutrient that is essential for bone health. Research shows that higher levels of zinc correlate with better bone mineral density, while lower blood levels have been associated with osteoporosis.40
That may be because zinc stimulates the activity of bone-forming osteoblasts, while suppressing bone-resorbing osteoclasts.41,42 Zinc also suppresses the bone-destroying effects of inflammatory compounds by modulating activity of the “master regulator of inflammation” nuclear factor-kappaB (NF-kB).41,42
In an animal study of postmenopause, zinc supplementation led to potent increases in bone mineralization as well as improvements in overall bone structure.43 In humans, oral supplementation of zinc prevented significant decreases in whole-body bone density and bone mineralization in women with low zinc consumption.44
Manganese Inhibits Postmenopausal Bone Loss
Manganese is a trace element with numerous properties that promote healthy bones.
In a rat model of postmenopause, manganese supplementation significantly improved both bone mineral content and bone mineral density in the femur, the large bone in the thigh.45
And in a study of postmenopausal women, combination of manganese, zinc and copper with calcium stopped bone loss in its tracks.46
Understanding Osteoporosis and Loss of Bone Mineral Density
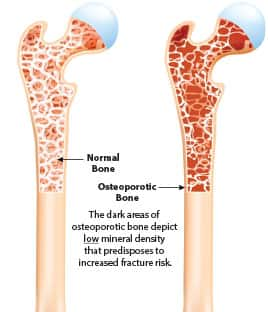 |
We typically think of bones as solid, static structures. In reality, they are living tissues that are constantly changing and responding to environmental stresses and other factors. With movement, exercise, weight gain, and other changes, bones grow stronger in some sections, while thinning in others.
Think of this process like a bank account. Cells called osteoblasts make deposits (leading to new bone formation and increased mineral density), while osteoclasts make withdrawals (leading to bone resorption and loss of mineral density).62,63
In healthy adult bones, this process is kept in balance. But as we age, the withdrawals start to outweigh the deposits, which reduces bone-mineral density and increases osteoporosis and fracture risks.64
Sex hormones like testosterone and estrogen are critical for maintaining this balance because they inhibit osteo clast activity (bone breakdown), and promote osteo blast activity (new bone formation).62,65
The problem is that sex hormones decrease starting in midlife, and this decline accelerates at menopause and andropause—which means they’re not able to preserve and maintain bone strength and quality as well as they should.64 The result is an overdraft in the bone mineralization “bank account,” ultimately leading to thinner bones and a higher risk of fractures.
These hormonal changes are a critical and too often overlooked factor in the rising osteoporosis risk we face as we age.64
But beware, many common drugs can also contribute to osteoporosis risk. Take a look:
• Cancer-fighting drugs that inhibit sex hormones, such as anti-androgen therapy (which reduces levels of testosterone) and aromatase inhibitors (which reduce estrogen activity), cause or contribute to bone loss, osteoporosis, and fracture risk.66,67
• Corticosteroids (prednisone, hydrocortisone, dexamethasone, and many others) have a clear and important association with bone loss and increased fracture risk.68,69
• Warfarin (Coumadin®) inhibits calcium from being incorporated into bone protein. At the same time, it also increases the risk of mineral deposits precisely where we don’t want them: in arterial walls.70-72
• Proton-pump inhibitors (e.g., Nexium®, Prilosec®, Prevacid®) can slow calcium absorption from the stomach, depriving the bone matrix of the minerals it needs to support a positive bone mineral balance.73
People taking any of these drugs may want to monitor their bone mineral status, as may people concerned about the impact of aging on their bones.
The most common bone mineral density test is DEXA. A problem with DEXA is that it can pick up calcification of blood vessels and arthritic regions and report this as bone density that does not exist. Life Extension® has long advocated for QCT (quantitative computerized tomography) bone mineral density testing. The challenge with QCT is it is not widely available like DEXA is.
Biological Silicon Promotes New Bone Formation
Silicon is the second most abundant element in the Earth’s crust.47 Most people think of this element in terms of its role in computers and engineering applications, but it plays a significant role in a number of life-science areas, including bone mineralization.
Animal studies of postmenopause show that silicon supplementation stops bone loss both in the vertebral column and in the femur (upper leg), while promoting bone growth and mineral density in the femur and tibia (lower leg).48,49 Closer examination in one animal model of postmenopause showed that silicon improved bone quality by reducing bone resorption—especially in those with low calcium intake.50
Human and animal studies indicate that silicon improves bone quality and strength and increases bone mineral density.12 Our bodies don’t absorb silicon very well in its elemental form. Fortunately, animal and human studies show that bioavailable silicon effectively promotes bone formation.49,51-53
Deadly Link between Osteoporosis and Heart Disease
A destructive effect of osteoporosis is the loss of the calcium from bone tissues, which leaves bones susceptible to fractures.
But where does the calcium go?
Discoveries over two decades show it often winds up in a bad place: the linings of blood vessels.
Lower bone densities (a measure of calcium content in the bones) are strongly associated with higher levels of dangerous arterial calcification, which occurs when calcium is deposited in the walls of blood vessels that supply blood to the body and the brain.74-79
This can be clearly seen on standard X-rays of the lower spine, where dense calcium mineral deposits in the aorta lie immediately next to shadowy, calcium-depleted vertebrae.77
In some instances, the calcification may form around valves.80 This can lead to narrowing of important heart valves, such as the aortic valve, leading to decreased blood flow, unhealthy thickening of the walls of the heart, and in later stages symptoms including fatigue and shortness of breath with mild exertion, and chest pain (angina).81
These are not theoretical risks. Studies show that the severity of osteoporosis is closely correlated with the severity of atherosclerosis.
• For example, one study showed that patients with osteoporosis had a disturbing 5.6-fold greater odds of having coronary artery disease than those without osteoporosis.78
• Men with low bone-mineral density in the spine have up to 36% greater risk of cardiovascular disease than those with normal density.76
• Among women, the risk of heart disease rises by as much as 28% with each incremental loss of bone-mineral density.76
The relationship between bone-mineral density and coronary heart disease works in the other direction as well. In one study, women with coronary heart-disease risks of 20% or more were at a 73% greater risk for thinning bones than were women whose heart-disease risk was less than 10%.75
Keeping calcium in the bone (which is what vitamin K2 helps facilitate) can provide the added benefit of reducing vascular calcium deposits, thereby simultaneously fighting two destructive pathologies of aging.
Boron Supports Bone Health
Boron is a component of the Earth’s crust that plays an underappreciated part in human health.54
Boron works with magnesium, calcium, and vitamin D to support bone metabolism and bone health.55-57
Clinical studies show that when people don’t get enough boron, they experience signs of bone loss resembling those seen in older men and in postmenopausal women with osteoporosis.55
Supplementation with boron has been shown to improve bone health specifically in diabetic mice, an important finding since diabetes is associated with lower bone density, bone quality, and fracture risk.58-60
A human study of a multi-nutrient supplement containing boron, calcium, vitamin D3, magnesium, zinc, copper, and manganese improved hip-bone mineral density in postmenopausal women, while also relieving back and joint pain.61
Supplementation with at least 3 mg/day of boron is recommended for anyone at risk of osteoporosis, or for those who don’t consume a lot of fruits and vegetables.54
Lifestyle Tips for Better Bone Health
While a certain amount of bone loss may occur with aging, developing osteoporosis is not inevitable. Regardless of genetic risks, most of us can maintain strong, fracture-resistant bones by exercising regularly, receiving preventive health check-ups, and nourishing our bone-building cells with bioavailable calcium and other supportive nutrients.
• Both men and women should follow a program of regular weight-bearing exercise to strengthen their bones. Join a gym or consult with a physical trainer.
• Avoid smoking and excess alcohol.
• Request a bone density test from your physician. QCT is superior to DEXA when measuring bone mineral density, but DEXA is often the only test available in many regions.
• Eat foods that are rich in calcium, other minerals, vitamins, and that are relatively low in phosphorus. Pay special attention to dark leafy vegetables, legumes, whole grains and, in moderation, milk products.
• Regardless of your gender, consider natural hormone replacement from midlife onward with appropriate hormones, under medical guidance.
Summary
Osteoporosis is a threat to all aging adults—including up to one-quarter of men.
Osteoporosis threatens not only bone strength, but also health throughout the body.
Ample calcium and vitamin D intake are essential for supporting good bone health as we age, but we also need sufficient amounts of other nutrients in order to optimize both skeletal and whole-body wellbeing.
Studies show that magnesium, zinc, manganese, silicon, and boron contribute to increased new bone formation and reduced bone resorption (or both), while also promoting calcium and vitamin D effectiveness.
The best bone-maintenance, osteoporosis-prevention program includes the full profile of bone nutrients.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Wright NC, Looker AC, Saag KG, et al. The Recent Prevalence of Osteoporosis and Low Bone Mass in the United States Based on Bone Mineral Density at the Femoral Neck or Lumbar Spine(). J Bone Miner Res. 2014;29(11):2520-6.
- Available at: https://www.iofbonehealth.org/facts-statistics. Accessed August 17, 2017.
- Sidlauskas KM, Sutton EE, Biddle MA. Osteoporosis in men: epidemiology and treatment with denosumab. Clin Interv Aging. 2014;9:593-601.
- Hannan EL, Magaziner J, Wang JJ, et al. Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. Jama. 2001;285(21):2736-42.
- Mehta KV, Lee HC, Loh JS. Mechanical thromboprophylaxis for patients undergoing hip fracture surgery. J Orthop Surg (Hong Kong). 2010;18(3):287-9.
- Available at: http://www.webmd.com/osteoporosis/osteoporosis-complications. Accessed August 17, 2017.
- Sun LM, Liang JA, Lin CL, et al. Cancer risk in patients with osteoporosis: a population-based cohort study. Curr Med Res Opin. 2017;33(4):733-9.
- Ye C, Xu M, Wang S, et al. Decreased Bone Mineral Density Is an Independent Predictor for the Development of Atherosclerosis: A Systematic Review and Meta-Analysis. PLoS One. 2016;11(5):e0154740.
- Amouzougan A, Lafaie L, Marotte H, et al. High prevalence of dementia in women with osteoporosis. Joint Bone Spine. 2016.
- Chang KH, Chung CJ, Lin CL, et al. Increased risk of dementia in patients with osteoporosis: a population-based retrospective cohort analysis. Age (Dordr). 2014;36(2):967-75.
- Drosselmeyer J, Rapp MA, Hadji P, et al. Depression risk in female patients with osteoporosis in primary care practices in Germany. Osteoporos Int. 2016;27(9):2739-44.
- Price CT, Koval KJ, Langford JR. Silicon: a review of its potential role in the prevention and treatment of postmenopausal osteoporosis. Int J Endocrinol. 2013;2013:316783.
- Ishimi Y. [Nutrition and bone health. Magnesium and bone]. Clin Calcium. 2010;20(5):762-7.
- Palacios C. The role of nutrients in bone health, from A to Z. Crit Rev Food Sci Nutr. 2006;46(8):621-8.
- Faine MP. Dietary factors related to preservation of oral and skeletal bone mass in women. J Prosthet Dent. 1995;73(1):65-72.
- Straub DA. Calcium supplementation in clinical practice: a review of forms, doses, and indications. Nutr Clin Pract. 2007;22(3):286-96.
- Bischoff-Ferrari HA, Rees JR, Grau MV, et al. Effect of calcium supplementation on fracture risk: a double-blind randomized controlled trial. Am J Clin Nutr. 2008;87(6):1945-51.
- Kalluru R, Ames R, Mason B, et al. Bone density in healthy men after cessation of calcium supplements: 20-month follow-up of a randomized controlled trial. Osteoporos Int. 2015;26(1):173-8.
- Ruml LA, Sakhaee K, Peterson R, et al. The effect of calcium citrate on bone density in the early and mid-postmenopausal period: a randomized placebo-controlled study. Am J Ther. 1999;6(6):303-11.
- Reid IR, Mason B, Horne A, et al. Randomized controlled trial of calcium in healthy older women. Am J Med. 2006;119(9):777-85.
- Weisman SM, Matkovic V. Potential use of biochemical markers of bone turnover for assessing the effect of calcium supplementation and predicting fracture risk. Clin Ther. 2005;27(3):299-308.
- Kenny AM, Prestwood KM, Biskup B, et al. Comparison of the effects of calcium loading with calcium citrate or calcium carbonate on bone turnover in postmenopausal women. Osteoporos Int. 2004;15(4):290-4.
- Bristow SM, Gamble GD, Stewart A, et al. Acute and 3-month effects of microcrystalline hydroxyapatite, calcium citrate and calcium carbonate on serum calcium and markers of bone turnover: a randomised controlled trial in postmenopausal women. Br J Nutr. 2014;112(10):1611-20.
- Newmark HL, Heaney RP, Lachance PA. Should calcium and vitamin D be added to the current enrichment program for cereal-grain products? Am J Clin Nutr. 2004;80(2):264-70
- Rizzoli R, Boonen S, Brandi ML, et al. Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Curr Med Res Opin. 2013;29(4):305-13.
- Quesada Gomez JM, Blanch Rubio J, Diaz Curiel M, et al. Calcium citrate and vitamin D in the treatment of osteoporosis. Clin Drug Investig. 2011;31(5):285-98.
- Bikle DD. Vitamin D and bone. Curr Osteoporos Rep. 2012;10(2):151-9.
- Schild A, Herter-Aeberli I, Fattinger K, et al. Oral Vitamin D Supplements Increase Serum 25-Hydroxyvitamin D in Postmenopausal Women and Reduce Bone Calcium Flux Measured by 41Ca Skeletal Labeling. J Nutr. 2015;145(10):2333-40.
- Claro da Silva T, Hiller C, Gai Z, et al. Vitamin D3 transactivates the zinc and manganese transporter SLC30A10 via the Vitamin D receptor. J Steroid Biochem Mol Biol. 2016;163:77-87.
- Paschalis EP, Gamsjaeger S, Hassler N, et al. Vitamin D and calcium supplementation for three years in postmenopausal osteoporosis significantly alters bone mineral and organic matrix quality. Bone. 2017;95:41-6.
- Weaver CM, Alexander DD, Boushey CJ, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27(1):367-76.
- Peris P, Martinez-Ferrer A, Monegal A, et al. 25 hydroxyvitamin D serum levels influence adequate response to bisphosphonate treatment in postmenopausal osteoporosis. Bone. 2012;51(1):54-8.
- Reymondier A, Caillet P, Abbas-Chorfa F, et al. MENOPOST-calcium and vitamin D supplementation in postmenopausal osteoporosis treatment: a descriptive cohort study. Osteoporos Int. 2013;24(2):559-66.
- Boonen S, Bouillon R, Haentjens P, et al. Optimizing the benefits of bisphosphonates in osteoporosis : the importance of appropriate calcium intake. Treat Endocrinol. 2006;5(6):375-83.
- Matsuzaki H. Prevention of osteoporosis by foods and dietary supplements. Magnesium and bone metabolism. Clin Calcium. 2006;16(10):1655-60.
- Matsuzaki H, Fuchigami M, Miwa M. Dietary magnesium supplementation suppresses bone resorption via inhibition of parathyroid hormone secretion in rats fed a high-phosphorus diet. Magnes Res. 2010;23(3):126-30.
- Katsumata SI, Matsuzaki H, Uehara M, et al. Effect of dietary magnesium supplementation on bone loss in rats fed a high phosphorus diet. Magnes Res. 2005;18(2):91-6.
- Dimai HP, Porta S, Wirnsberger G, et al. Daily oral magnesium supplementation suppresses bone turnover in young adult males. J Clin Endocrinol Metab. 1998;83(8):2742-8.
- Aydin H, Deyneli O, Yavuz D, et al. Short-term oral magnesium supplementation suppresses bone turnover in postmenopausal osteoporotic women. Biol Trace Elem Res. 2010;133(2):136-43.
- Hyun TH, Barrett-Connor E, Milne DB. Zinc intakes and plasma concentrations in men with osteoporosis: the Rancho Bernardo Study. Am J Clin Nutr. 2004;80(3):715-21.
- Yamaguchi M. Role of nutritional zinc in the prevention of osteoporosis. Mol Cell Biochem. 2010;338(1-2):241-54.
- Yamaguchi M, Weitzmann MN. Zinc stimulates osteoblastogenesis and suppresses osteoclastogenesis by antagonizing NF-kappaB activation. Mol Cell Biochem. 2011;355(1-2):179-86.
- Bhardwaj P, Rai DV, Garg ML. Zinc as a nutritional approach to bone loss prevention in an ovariectomized rat model. Menopause. 2013;20(11):1184-93.
- Nielsen FH, Lukaski HC, Johnson LK, et al. Reported zinc, but not copper, intakes influence whole-body bone density, mineral content and T score responses to zinc and copper supplementation in healthy postmenopausal women. Br J Nutr. 2011;106(12):1872-9.
- Rico H, Gomez-Raso N, Revilla M, et al. Effects on bone loss of manganese alone or with copper supplement in ovariectomized rats. A morphometric and densitomeric study. Eur J Obstet Gynecol Reprod Biol. 2000;90(1):97-101.
- Strause L, Saltman P, Smith KT, et al. Spinal bone loss in postmenopausal women supplemented with calcium and trace minerals. J Nutr. 1994;124(7):1060-4.
- Luyckx M, Hausman JF, Lutts S, et al. Silicon and Plants: Current Knowledge and Technological Perspectives. Front Plant Sci. 2017;8:411.
- Rico H, Gallego-Lago JL, Hernandez ER, et al. Effect of silicon supplement on osteopenia induced by ovariectomy in rats. Calcif Tissue Int. 2000;66(1):53-5.
- Bae YJ, Kim JY, Choi MK, et al. Short-term administration of water-soluble silicon improves mineral density of the femur and tibia in ovariectomized rats. Biol Trace Elem Res. 2008;124(2):157-63.
- Kim MH, Bae YJ, Choi MK, et al. Silicon supplementation improves the bone mineral density of calcium-deficient ovariectomized rats by reducing bone resorption. Biol Trace Elem Res. 2009;128(3):239-47.
- Jugdaohsingh R. Silicon and bone health. J Nutr Health Aging. 2007;11(2):99-110.
- Schiano A, Eisinger F, Detolle P, et al. [Silicon, bone tissue and immunity]. Rev Rhum Mal Osteoartic. 1979;46(7-9):483-6.
- Eisinger J, Clairet D. Effects of silicon, fluoride, etidronate and magnesium on bone mineral density: a retrospective study. Magnes Res. 1993;6(3):247-9.
- Pizzorno L. Nothing Boring About Boron. Integr Med (Encinitas). 2015;14(4):35-48.
- Nielsen FH. Studies on the relationship between boron and magnesium which possibly affects the formation and maintenance of bones. Magnes Trace Elem. 1990;9(2):61-9.
- Volpe SL, Taper LJ, Meacham S. The relationship between boron and magnesium status and bone mineral density in the human: a review. Magnes Res. 1993;6(3):291-6.
- Schaafsma A, de Vries PJ, Saris WH. Delay of natural bone loss by higher intakes of specific minerals and vitamins. Crit Rev Food Sci Nutr. 2001;41(4):225-49.
- Available at: https://www.niams.nih.gov/Health_Info/Bone/ Osteoporosis/Conditions_Behaviors/diabetes.asp. Accessed August 28, 2017.
- Chau DL, Edelman SV. Osteoporosis and Diabetes. Clinical Diabetes. 2002;20(3):153-7.
- Dessordi R, Spirlandeli AL, Zamarioli A, et al. Boron supplementation improves bone health of non-obese diabetic mice. J Trace Elem Med Biol. 2017;39:169-75.
- Benevolenskaia LI, Toroptsova NV, Nikitinskaia OA, et al. Vitrum osteomag in prevention of osteoporosis in postmenopausal women: results of the comparative open multicenter trial Ter Arkh. 2004;76(11):88-93.
- Lerner UH. Bone remodeling in post-menopausal osteoporosis J Dent Res. 2006;85(7):584-95.
- Tanaka Y, Nakayamada S, Okada Y. Osteoblasts and osteoclasts in bone remodeling and inflammation. Curr Drug Targets Inflamm Allergy. 2005;4(3):325-8.
- Demontiero O, Vidal C, Duque G. Aging and bone loss: new insights for the clinician. Ther Adv Musculoskelet Dis. 2012;4(2): 61-76.
- Riggs BL, Khosla S, Melton LJ, 3rd. Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002;23(3):279-302.
- Lumachi F, Luisetto G, Basso SM, et al. Endocrine therapy of breast cancer. Curr Med Chem. 2011;18(4):513-22.
- Mazziotti G, Canalis E, Giustina A. Drug-induced osteoporosis: mechanisms and clinical implications. Am J Med. 2010;123(10):877-84.
- Briot K, Roux C. Drug-induced osteoporosis: beyond glucocorticoids. Curr Rheumatol Rep. 2008;10(2):102-9.
- Mirza F, Canalis E. Management of endocrine disease: Secondary osteoporosis: pathophysiology and management. Eur J Endocrinol. 2015;173(3):R131-51.
- Cranenburg EC, Schurgers LJ, Vermeer C. Vitamin K: the coagulation vitamin that became omnipotent. Thromb Haemost. 2007;98(1):120-5.
- Namba S, Yamaoka-Tojo M, Hashikata T, et al. Long-term warfarin therapy and biomarkers for osteoporosis and atherosclerosis. BBA Clin. 2015;4:76-80.
- Namba S, Yamaoka-Tojo M, Kakizaki R, et al. Effects on bone metabolism markers and arterial stiffness by switching to rivaroxaban from warfarin in patients with atrial fibrillation. Heart Vessels. 2017.
- Kopic S, Geibel JP. Gastric acid, calcium absorption, and their impact on bone health. Physiol Rev. 2013;93(1):189-268.
- Barengolts EI, Berman M, Kukreja SC, et al. Osteoporosis and coronary atherosclerosis in asymptomatic postmenopausal women. Calcif Tissue Int. 1998;62(3):209-13.
- Broussard DL, Magnus JH. Coronary heart disease risk and bone mineral density among U.S. women and men. J Womens Health (Larchmt). 2008;17(3):479-90.
- Farhat GN, Strotmeyer ES, Newman AB, et al. Volumetric and areal bone mineral density measures are associated with cardiovascular disease in older men and women: the health, aging, and body composition study. Calcif Tissue Int. 2006;79(2):102-11.
- Kiel DP, Kauppila LI, Cupples LA, et al. Bone loss and the progression of abdominal aortic calcification over a 25 year period: the Framingham Heart Study. Calcif Tissue Int. 2001;68(5):271-6.
- Marcovitz PA, Tran HH, Franklin BA, et al. Usefulness of bone mineral density to predict significant coronary artery disease Am J Cardiol. 2005;96(8):1059-63.
- Tanko LB, Bagger YZ, Christiansen C. Low bone mineral density in the hip as a marker of advanced atherosclerosis in elderly women. Calcif Tissue Int. 2003;73(1):15-20.
- Pfister R, Michels G, Sharp SJ, et al. Inverse association between bone mineral density and risk of aortic stenosis in men and women in EPIC-Norfolk prospective study. Int J Cardiol. 2015;178:29-30.
- Available at: https://medlineplus.gov/ency/article/000178.htmAccessed August 28, 2017.

