Life Extension Magazine®
Mainstream medicine can do little to treat arthritis other than reduce the pain, often with huge safety risks.
A mixture of herbs has been shown to improve the integrity of cartilage in affected joints.1 These herbs work to slow the progression of cartilage degeneration.
A new study adds to prior work on use of botanical agents in human and animal studies of osteoarthritis, which is the most common joint disorder in the United States.2
This article reviews key botanical agents that can prevent osteoarthritis-associated joint damage, plus an herb that performed comparably with naproxen, and better than celecoxib (Celebrex®) in relieving pain and stiffness.
Three botanical extracts –Scutellaria baicalensis, Acacia catechu, and Morus alba can enable a significant reduction in the progression of arthritis.
These herbs have been shown to reduce destruction of cartilage and bone in arthritis-afflicted joints, and to significantly reduce pain and inflammation.1,3,4
These botanical extracts may also act as the disease-modifying agents so eagerly sought for many years by scientists and physicians.
Mainstream medicine has yet to find true disease-modifying drugs for osteoarthritis,5,6 leaving us mainly with drugs in the class called non-steroidal anti-inflammatory drugs (NSAIDs, like ibuprofen), or with painkillers in the opioid narcotic category.
White Mulberry and Cutch Tree Extracts Restore Joint Integrity

The combination of Morus alba (white mulberry) and Acacia catechu (cutch tree) extracts is the result of a research program that began with 12,000 plant samples known to be used in human food or medical traditions.4 The winning combination has been extensively evaluated in human, animal, and basic laboratory studies for its ability to fight the inflammation, pain, and joint degradation seen in osteoarthritis.4
The most recent advance with this natural supplement mixture came in early 2017, with the release of a rat study, where conditions can be carefully controlled and all variables isolated.
In this study, scientists first examined the impact of the formulation on degradation of proteoglycans, essential components of the cartilage matrix. Here, they demonstrated that the formulation reduced cartilage breakdown by 31.5% to 54.8%, depending on the dose used.1 This was a powerful demonstration of the mixture’s cartilage-protecting abilities.
Next, the scientists created a rat model of osteoarthritis by injecting the animals’ joints with a chemical known to induce the inflammatory changes that produce arthritis.1 Administering the combination supplement and measuring the animals’ pain sensitivity weekly, the researchers detected reductions in pain sensitivity of 17.5% in the first week, which rose steadily through week five to 40.9%.1
In addition to this reduction in pain sensitivity in the living animals, significant improvements in joint cartilage integrity were recorded, and bone damage below the protective cartilage layer in joints was found to be minimal.1
The finding of reduced bone and cartilage destruction in arthritis joints, by direct examination of the affected joints, represents a disease-modifying effect that has never been shown with any pain-relieving drug (NSAIDs or opiates) commonly used to treat osteoarthritis. This represents a novel advance in the management of arthritis, making it a potentially reversible disorder.
Some additional work sheds light on the mechanisms involved.
The same scientists carried out a study using a well-established rat model of pain: injection of a compound, carrageenan, into the paw, which induces temporary pain and swelling. The results of that study confirmed that the combined extracts were superior to no treatment in improving pain and reducing swelling, while the highest dose tested proved similar to ibuprofen for those effects.7
That study and others also showed this herbal combination inhibition of the enzymes COX-1, COX-2, and 5-LOX, which produce pro-inflammatory signaling molecules.4,7 Suppressing these pro-inflammatory enzymes is an essential mechanism when seeking to protect against joint cartilage destruction.
Human Studies on these Herbs

The most compelling studies are those in which supplements show meaningful effects in humans, where we cannot impose pain deliberately, nor can we expose joints and look inside.
A study completed in 2015 evaluated 135 adults between the ages of 35 and 75 who had knee pain and arthritis. The study subjects were randomly assigned to receive 200 mg twice daily of the herbal combination supplement, a glucosamine 750 mg/chondroitin 600 mg combination twice daily, or an inactive placebo.4
A main outcome measure in this study was urinary levels of C-terminal crosslinking telopeptide of type II collagen (CTX-II), a breakdown product of collagen that serves as a useful indirect biomarker of joint destruction.
Levels of urinary CTX-II dropped from baseline in the patients receiving the herbal combination, while rising dramatically in placebo-treated patients, producing a significant difference between the drug and herb-extract treatments. No significant changes were seen in the glucosamine/chondroitin group.4
In summary, the combination of Morus alba and Acacia catechu reduces joint destruction in both human and animal studies, doing so in large part by inhibition of pro-inflammatory signaling molecule production.4,8
Human studies have also demonstrated a good safety record, showing mild side effects comparable to those seen in placebo subjects.4,8
Chinese Skullcap and Cutch Tree Extracts Outperform Standard Pain Relievers

Chinese skullcap (Scutellaria baicalensis) is rich in a compound called baicalin, with known anti-inflammatory properties that complement those in cutch tree (Acacia catechu).9,10
Animal and basic lab studies have established that the combination of these two herbs acts as a dual inhibitor of inflammatory signaling molecule production and activity, and is capable of significantly reducing pain and swelling.3,8,11-14
Two important human randomized, controlled trials have emerged, demonstrating that, in people with osteoarthritis, the Scutellaria/Acacia extract combination performs as well, or better, than the NSAID pain relievers most commonly used to treat osteoarthritis.
One study, conducted by pain relief experts in Montreal, included 52 subjects (40-75 years old) with osteoarthritis of the knee or hip severe enough to require treatment.15
Subjects were randomly assigned a placebo, 200 mg/day of the celecoxib, or one of two doses of the combination herbal supplement (250 or 500 mg/day). Study subjects were followed-up at 30, 60, and 90 days for pain, stiffness, functional impairment, and physical function using standard measurement scales.
Study results were impressive, showing that at days 30 and 90, both doses of the dual-action supplement were significantly more effective at reducing pain than celecoxib. The higher, 500-mg/day herbal dose proved superior to celecoxib already at day 30, and was superior to placebo by the 90-day endpoint of the study. By contrast, celecoxib was not significantly more effective than placebo at days 30 or 90.
For reducing stiffness, both herbal supplement doses were effective at all time points compared with baseline measures.15 Similarly, both doses were superior to placebo for stiffness relief at 30 and 90 days, while no changes compared with baseline stiffness were seen in either the placebo or the celecoxib groups.
Functional impairment was significantly better in the 500 mg herb-supplement group compared to celecoxib or placebo at all time points, with a significant improvement compared with baseline as well, an effect not seen in either the celecoxib or placebo groups.
Finally, scores for physical function were significantly improved compared to baseline for both doses of the herb-supplement combination and for celecoxib at all time points, while by day 90, the supplement was superior to celecoxib.
No significant adverse events were reported, and screening blood tests showed no abnormalities in any of the groups.
What is Osteoarthritis?
 |
Arthritis is an imprecise term, meaning simply “inflammation of a joint.” Types of arthritis include osteoarthritis (formerly called “degenerative arthritis”) and rheumatoid arthritis, which is an autoimmune disease in which the body attacks and destroys its own joints.
A thick layer of cartilage lines the surfaces of the bones that form a normal healthy joint, providing lubrication and protection against wear and tear from everyday movement.
Cartilage is made up of extracellular material, primarily water, collagen, and specialized proteins called proteoglycans, which break apart over time.4
For many years, scientists and physicians thought that inflammation was a key feature only of rheumatoid arthritis, and that osteoarthritis was a simple, natural, and inevitable degeneration of joint components, primarily cartilage and bone.
That simplistic picture has changed.
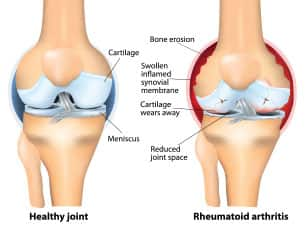 |
Scientists now recognize that inflammation does indeed play a crucial role in osteoarthritis, contributing directly to the loss of cushioning cartilage, and eventually bone, that we see in this debilitating and potentially crippling condition.
Signs and symptoms of osteoarthritis are consistent with progressive, inflammation-promoted loss of cartilage, eventually leading to pain, stiffness, and loss of mobility.1 As the collagen matrix that makes up cartilage becomes disorganized, bits of collagen enter the joint space, where they induce a further inflammatory reaction.17-19
Osteoarthritis can become severe enough that cartilage thins to become virtually absent, leading to bone grinding directly on bone, producing severe pain and ultimately leading to joint destruction and immobility.
Scientists can now measure products of cartilage degradation that are excreted in the urine—a molecule called C-terminal crosslinking telopeptide of type II collagen (CTX-II) is a valid indicator of the degree of collagen loss, and therefore a useful measure of disease progression.20
CTX-II is therefore a useful standard by which to measure the disease-modifying potential of any drug, supplement, or other therapeutic intervention. As shown in this article, the combination of Morus alba and Acacia catechu extracts significantly reduced urinary concentrations of CTX-II in subjects with knee osteoarthritis, indicating a disease-modifying capability.
Follow-Up Second Human Study

A second study extended these impressive findings, comparing a daily 500 mg-dose of the combined herbal supplement with the NSAID naproxen, 440 mg/day, in 79 adults aged 40-90 years, with mild to moderate osteoarthritis.16
This study lasted just one week to evaluate the short-term effects of this supplement combination.
Results showed that, for pain, the Scutellaria/Acacia supplement significantly reduced pain scores from baseline to end of study, with no significant reduction seen in the naproxen recipients.16
Both herbal- and naproxen-treated patients had significant reductions of stiffness from baseline to final values, whereas the herbal group, but not the naproxen group, had significant improvements in joint range of motion compared with baseline. Naproxen recipients had an insignificant decrease in range of motion.
These two studies, combined with the wealth of lab and animal data, establishes a role for Scutellaria baicalensis and Acacia catechu extracts in combination for reductions in the pain, stiffness, and loss of mobility seen in patients with osteoarthritis, and strongly suggest its superiority to existing NSAID drugs.
Summary

Osteoarthritis is a potentially crippling joint condition suffered by millions of Americans, for whom pain relief has only been possible through the use of damaging NSAID drugs or opioid narcotics, none of which make any difference in severity or progression of the disease.
Three herbal extracts have been shown to reduce the destruction of cartilage and bone in osteoarthritis, while outperforming two popular NSAID drugs at relieving pain, stiffness, and loss of mobility.
Now available in a single convenient supplement, standardized extracts Acacia catechu, Morus alba, and Scutellaria baicalensis can bring significant pain relief to osteoarthritis sufferers, while exerting a true disease-modifying effect unlike any existing pain medication.
People with moderate to severe osteoarthritis should consider trying this herbal combination in an effort to avoid the potentially destructive long-term effects of NSAID and narcotic drugs.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Yimam M, Lee YC, Wright L, et al. A Botanical Composition Mitigates Cartilage Degradations and Pain Sensitivity in Osteoarthritis Disease Model. J Med Food. 2017;20(6):568-76.
- Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355-69.
- Yimam M, Brownell L, Pantier M, et al. UP446, analgesic and anti-inflammatory botanical composition. Pharmacognosy Res. 2013;5(3):139-45.
- Unigen Inc. Amlexin: A New Approach to Joint Protection. Unpublished data.2015.
- Dar QA, Schott EM, Catheline SE, et al. Daily oral consumption of hydrolyzed type 1 collagen is chondroprotective and anti-inflammatory in murine posttraumatic osteoarthritis. PLoS One. 2017;12(4):e0174705.
- Skrepnik N, Spitzer A, Altman R, et al. Assessing the Impact of a Novel Smartphone Application Compared With Standard Follow-Up on Mobility of Patients With Knee Osteoarthritis Following Treatment With Hylan G-F 20: A Randomized Controlled Trial. JMIR Mhealth Uhealth. 2017;5(5):e64.
- Yimam M, Lee YC, Jiao P, et al. UP1306, a Botanical Composition with Analgesic and Anti-inflammatory Effect. Pharmacognosy Res. 2016;8(3):186-92.
- Burnett BP, Jia Q, Zhao Y, et al. A medicinal extract of Scutellaria baicalensis and Acacia catechu acts as a dual inhibitor of cyclooxygenase and 5-lipoxygenase to reduce inflammation. J Med Food. 2007;10(3):442-51.
- Dinda B, Dinda S, DasSharma S, et al. Therapeutic potentials of baicalin and its aglycone, baicalein against inflammatory disorders. Eur J Med Chem. 2017;131:68-80.
- Yang X, Yang J, Zou H. Baicalin inhibits IL-17-mediated joint inflammation in murine adjuvant-induced arthritis. Clin Dev Immunol. 2013;2013:268065.
- Altavilla D, Squadrito F, Bitto A, et al. Flavocoxid, a dual inhibitor of cyclooxygenase and 5-lipoxygenase, blunts pro-inflammatory phenotype activation in endotoxin-stimulated macrophages. Br J Pharmacol. 2009;157(8):1410-8.
- Tseng-Crank J, Sung S, Jia Q, et al. A medicinal plant extract of Scutellaria Baicalensis and Acacia catechu reduced LPS-stimulated gene expression in immune cells: a comprehensive genomic study using QPCR, ELISA, and microarray. J Diet Suppl. 2010;7(3):253-72.
- Yimam M, Brownell L, Hodges M, et al. Analgesic effects of a standardized bioflavonoid composition from Scutellaria baicalensis and Acacia catechu. J Diet Suppl. 2012;9(3):155-65.
- Unigen Inc. Univestin: Advanced Joint Comfort. Unpublished data.2015.
- Sampalis JS, Brownell LA. A randomized, double blind, placebo and active comparator controlled pilot study of UP446, a novel dual pathway inhibitor anti-inflammatory agent of botanical origin. Nutr J. 2012;11:21.
- Arjmandi BH, Ormsbee LT, Elam ML, et al. A combination of Scutellaria baicalensis and Acacia catechu extracts for short-term symptomatic relief of joint discomfort associated with osteoarthritis of the knee. J Med Food. 2014;17(6):707-13.
- Bollet AJ, Nance JL. Biochemical Findings in Normal and Osteoarthritic Articular Cartilage. II. Chondroitin Sulfate Concentration and Chain Length, Water, and Ash Content. J Clin Invest. 1966;45(7):1170-7.
- Chou MC, Tsai PH, Huang GS, et al. Correlation between the MR T2 value at 4.7 T and relative water content in articular cartilage in experimental osteoarthritis induced by ACL transection. Osteoarthritis Cartilage. 2009;17(4):441-7.
- Madry H, Luyten FP, Facchini A. Biological aspects of early osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):407-22.
- Charni N, Juillet F, Garnero P. Urinary type II collagen helical peptide (HELIX-II) as a new biochemical marker of cartilage degradation in patients with osteoarthritis and rheumatoid arthritis. Arthritis Rheum. 2005;52(4):1081-90.

