Life Extension Magazine®

Back in year 1854, a pioneering physician in London made a heroic effort to demonstrate that drinking feces-laden water was dangerous.1
Contaminated water breeds bacteria like cholera that kill an estimated 95,000 people a year worldwide where feces-ingestion continues.2
Cigarettes caused greater mortality before the lethal dangers were exposed. Tobacco remains a leading reason for premature death.3,4
Sugar may be killing more people than cholera or tobacco.
If history is any guide, the majority will continue to ingest excess glucose-spiking sugars and starches despite the life-shortening impact.
The magnitude of today’s carnage calls for stronger public-health initiatives.
Put simply, there is no reason to add sugar to food or drinks. This includes high-fructose corn syrup, high-fructose juices, sucrose, and starches that spike blood glucose levels.5-8
To better understand today’s epidemic of obesity and diabetes, the chart on the next page reveals the surging increase in human sugar consumption.
From a nutritional standpoint, there is no need for people to consume sugars or starches. While glucose is essential to sustain life, plenty of glucose is synthesized in our liver from protein and fats we ingest. This natural internal production of glucose is called “gluconeogenesis.”
The public has been slow to give up their sugar addiction. What I find interesting are people who would never tolerate tobacco or feces-laden water, but have little concern about their sugar/starch consumption.
This month’s issue describes a major advance in lowering glucose and insulin blood levels. This natural approach applies not only to those with diabetic concerns, but also maturing people seeking to protect against glucose/insulin toxicity.
The take-home message is that sugar is not fit for human consumption. For those unwilling to alter their diet, novel nutrient extracts have been shown to suppress after-meal glucose/insulin blood levels while lowering hemoglobin A1C.
It’s hard to perceive that something you have consumed your entire life is deadly.
Sugar is so ubiquitous that you might assume people always used it.
The reality is that refined sugar consumption has been virtually zero throughout most of human history.
In 1700, for instance, the average person in England is estimated to have consumed about four pounds of refined sugar a year. Annual refined sugar ingestion has now shot up to over 100 pounds.9
Excess sugar ingestion is a factor behind surging rates of obesity,10-12 cancer,13-17 vascular disorders,18-27 dementia,28-31 and type II diabetes.11,32-34
A large part of today’s healthcare cost crisis could be resolved if people went back to ingesting little or no sugar.
How Sugar Addiction Began

over past 300 years. Data from 1700-1978
is from UK and data from 1975-2000 is from
the US. Not reflected are temporary declines
in sugar intake during major wars when food
supplies were disrupted.9
When Europeans colonized the Americas, they transmitted infectious illnesses like smallpox that decimated native populations that lacked natural immunity against these pathogens.
Native Americans in turn taught Europeans about tobacco and sugar cane, which unknowingly began killing off people who began smoking tobacco and eating refined sugar.
Since average lifespans in the 1700s-1800s were so short, the impact of these poisons (tobacco and sugar) went largely unrecognized.
Sugar reached Europeans in the 1200s from South Asia, but it was so expensive that only the wealthy could afford it. As sugar plantations emerged in the Americas, prices plummeted and a sugar craze was ignited in Europe.
The impact of society’s sugar addiction is a global medical crisis that has been centuries in the making.
It’s now time to classify sugar as a toxin analogous to tobacco, with harsh warning labels on high glycemic food/drink, along with restricted sales to children.
Is Sugar a Carcinogen?

tobacco industry
deceived the public
in the 1950s, those
selling glucose-spiking
foods/beverages today
conveniently overlook
the lethal consequences.
The history of sugar and tobacco are closely aligned. Both were initially thought to be harmless. It took centuries for the public to realize the dangers of tobacco.
The scourge of sugar-inflicted disease has yet to be recognized by the medical profession.
We at Life Extension® advise cancer patients to stop all simple sugar consumption and cut back on glucose-spiking starches like rice, bread, and other wheat/corn products.
Excess glucose feeds rapidly dividing malignant cells.35-37 The high insulin release that occurs in response to sugar/starch ingestion promotes cancer cell proliferation.38-40
Researchers at MD Anderson last year uncovered another mechanism by which high sugar intake increases breast cancer risk and facilitates lung cancer metastasis. In the rodent model, high sucrose or fructose intake increases inflammatory pathways involved in cancer initiation and metastasis.41
The volume of data pointing to sugar as a probable carcinogen is frightening in light of today’s excess consumption of high glycemic food/drink.13,14,42,43
Our Bodies do not Need Exogenous Sugar

Glucose is essential to sustaining life. So much so that our bodies have developed efficient mechanisms to ensure most of us always maintain adequate blood glucose levels.
In between meals, glucose is created from the breakdown of glycogen in our liver and muscles. Our liver can also utilize proteins/fats and convert them to glucose via a process called gluconeogenesis.
Just imagine the challenges our ancestors faced in wintry months when the only food source was meat. Without the ability to convert the proteins/fat in meat to glucose, early man would not have survived these long periods without access to carbohydrates.
Move forward to modern times. Sugar/starch ingestion has surged, but our aging cells have lost much of their insulin sensitivity.
So in response to excess sugar-starch ingestion, our cells are unable to fully utilize glucose because they are resistant to insulin. But our liver keeps synthesizing more glucose (via gluconeogenesis) and pouring it into our blood. The result for many aging people is constant glucose/insulin overload.
These facts make it clear that humans should not ingest significant quantities of refined sugars. Even when no simple sugars or starches are consumed, some people still have higher-than-optimal blood glucose/insulin because their livers overproduce glucose.
Those who practice strict calorie restriction maintain low fasting and after-meal glucose/insulin levels.44 Few, however, are willing to chronically under eat.
An urgent need exists to enable typical people to lower their blood glucose and insulin levels. But studies have shown sugar to be addictive in a manner analogous to cocaine, according to one published report.45
Danger of Excess Insulin

promoted the nonexistent
health benefits of cigarettes.
Blood glucose increases in response to sugar/starch ingestion, overproduction of glucose (gluconeogenesis) in our liver, and other factors related to aging.
Our pancreas responds to glucose by secreting lots of insulin, sometimes in a chronic state termed hyperinsulinemia.
The problem is that as aging cells become insulin resistant, glucose blood levels remain high even as the pancreas secretes more insulin in an attempt to drive glucose into cells.
Some prediabetics will maintain normal fasting glucose for years because their pancreas secretes huge amounts of insulin that drive down blood glucose levels.
Elevated insulin has been correlated with virtually every diabetic disorder.46-50
As has been extensively reported for decades in Life Extension Magazine®, those with elevated insulin have sharply higher incidences of degenerative disorders.51-60
The encouraging news is that natural plant extracts have been identified that can lower cell-damaging insulin surges.
Slash Post-Meal Glucose and Insulin

was so ubiquitous,
the public was largely
unaware of the dangers
of tobacco, analogous
to how refined sugar
products are
marketed today.
In youth, our body responds to a meal by secreting enough insulin to drive glucose into cells for energy production or fat storage.
In healthy young individuals, once blood glucose drops to a safe level, insulin production subsides. A delicate balance is then maintained as glucose is modestly released from the liver (gluconeogenesis) along with modest pancreatic insulin secretion.
With aging, our cells become insulin resistant and lose their ability to efficiently take up glucose. This creates a vicious cycle whereby the pancreas over secretes insulin in what can be a futile attempt to drive glucose into cells.
The pathological impact is chronically elevated glucose and insulin levels.
Despite most aging individuals having too much blood glucose and insulin, they continue to gorge on refined sugars and starches. This sets the stage for today’s health crisis of obesity and type II diabetes.61
A novel solution has been discovered utilizing natural plant extracts that slash after-meal insulin by as much as 56% along with impressive reductions in after-meal glucose and a 0.3% drop in hemoglobin A1C (from 5.65% to 5.35%).62,63
The unique mechanisms by which these plants function are described in an article that begins on page 26 of this issue.
I hope people reading this editorial will reduce their simple sugar intake to virtually zero while cutting back on glucose-spiking starches (rice, white bread, potatoes, corn, etc.).
For those unable to achieve optimal glucose/insulin blood levels, the availability of clinically-tested plant extracts should provide welcome respite from the impact of glucose-spiking calories.
For longer life,
William Faloon, Co-Founder
Life Extension Buyers Club
Tribute to a Medical Pioneer—Dr. John Snow (1813-1858)
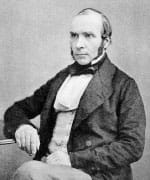 |
John Snow, MD, is the genius who created the modern science of epidemiology.1
Dr. Snow demonstrated that feces-laden water consumed by the people of London in the mid-1800s was causing cholera and other epidemic diseases.1
Physicians at that time had not yet recognized the “germ theory” of disease. Dr. Snow nonetheless concluded that contaminated water was the source of a self-replicating poison that was killing thousands of London residents.
Few people of his day followed Dr. Snow’s admonition to boil drinking water and avoid fluids that emanated from the bowels of cholera patients.
The medical establishment did not agree with Dr. Snow’s admonition to avoid contaminated drinking water.
Physicians in 1854 attributed cholera and other enteric diseases to the foul smelling gases produced by piles of rotting garbage and raw sewage that characterized London at that time.1
Mainstream medicine continues to overlook proven methods to prevent, mitigate, or eradicate chronic disorders. The result is that many Americans today needlessly suffer and die.
A fundamental purpose of Life Extension is to investigate and identify the underlying culprits behind today’s epidemics and devise practical protocols to circumvent them.
Future historians are likely to lump excessive consumption of simple sugars in the same way we view detrimental habits such as tobacco use and unhygienic practices.
References
- Markel H. A piece of my mind. Happy birthday, Dr Snow. Jama. 2013;309(10):995-6.
- Ali M, Nelson AR, Lopez AL, et al. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis. 2015;9(6):e0003832.
- Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Surg Clin. 2013;23(2):103-12.
- Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/. Accessed July 12, 2017.
- Bray GA. Fructose: pure, white, and deadly? Fructose, by any other name, is a health hazard. J Diabetes Sci Technol. 2010;4(4):1003-7.
- Gross LS, Li L, Ford ES, et al. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. The American Journal of Clinical Nutrition. 2004;79(5):774-9.
- Takao T, Ogawa M, Ishii Y, et al. Different glycemic resposes to sucrose and glucose in old and young male adults. J Nutr Food Sci. 2016;6(460):2.
- Lee BM, Wolever TM. Effect of glucose, sucrose and fructose on plasma glucose and insulin responses in normal humans: comparison with white bread. Eur J Clin Nutr. 1998;52(12):924-8.
- Johnson RJ, Segal MS, Sautin Y, et al. Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. Am J Clin Nutr. 2007;86(4):899-906.
- Kuhnle GG, Tasevska N, Lentjes MA, et al. Association between sucrose intake and risk of overweight and obesity in a prospective sub-cohort of the European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk). Public Health Nutr. 2015;18(15):2815-24.
- Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. Jama. 2004;292(8):927-34.
- Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14(8):606-19.
- Stattin P, Bjor O, Ferrari P, et al. Prospective study of hyperglycemia and cancer risk. Diabetes Care. 2007;30(3):561-7.
- Muti P, Quattrin T, Grant BJ, et al. Fasting glucose is a risk factor for breast cancer: a prospective study. Cancer Epidemiol Biomarkers Prev. 2002;11(11):1361-8.
- Sieri S, Muti P, Claudia A, et al. Prospective study on the role of glucose metabolism in breast cancer occurrence. Int J Cancer. 2012;130(4):921-9.
- Schoen RE, Tangen CM, Kuller LH, et al. Increased blood glucose and insulin, body size, and incident colorectal cancer. J Natl Cancer Inst. 1999;91(13):1147-54.
- Yamagata H, Kiyohara Y, Nakamura S, et al. Impact of fasting plasma glucose levels on gastric cancer incidence in a general Japanese population: the Hisayama study. Diabetes Care. 2005;28(4): 789-94.
- Pan WH, Cedres LB, Liu K, et al. Relationship of clinical diabetes and asymptomatic hyperglycemia to risk of coronary heart disease mortality in men and women. Am J Epidemiol. 1986;123(3):504-16.
- Coutinho M, Gerstein HC, Wang Y, et al. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care. 1999;22(2):233-40.
- Bardini G, Dicembrini I, Cresci B, et al. Inflammation markers and metabolic characteristics of subjects with 1-h plasma glucose levels. Diabetes Care. 2010;33(2):411-3.
- Ceriello A. Impaired glucose tolerance and cardiovascular disease: the possible role of post-prandial hyperglycemia. Am Heart J. 2004;147(5):803-7.
- de Vegt F, Dekker JM, Ruhe HG, et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia. 1999;42(8):926-31.
- Beulens JW, de Bruijne LM, Stolk RP, et al. High dietary glycemic load and glycemic index increase risk of cardiovascular disease among middle-aged women: a population-based follow-up study. J Am Coll Cardiol. 2007;50(1):14-21.
- Halton TL, Willett WC, Liu S, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med. 2006;355(19):1991-2002.
- Mirrahimi A, de Souza RJ, Chiavaroli L, et al. Associations of glycemic index and load with coronary heart disease events: a systematic review and meta-analysis of prospective cohorts. J Am Heart Assoc. 2012;1(5):e000752.
- Bjornholt JV, Erikssen G, Aaser E, et al. Fasting blood glucose: an underestimated risk factor for cardiovascular death. Results from a 22-year follow-up of healthy nondiabetic men. Diabetes Care. 1999;22(1):45-9.
- Shaye K, Amir T, Shlomo S, et al. Fasting glucose levels within the high normal range predict cardiovascular outcome. Am Heart J. 2012;164(1):111-6.
- Crane PK, Walker R, Hubbard RA, et al. Glucose levels and risk of dementia. N Engl J Med. 2013;369(6):540-8.
- Pase MP, Himali JJ, Beiser AS, et al. Sugar- and Artificially Sweetened Beverages and the Risks of Incident Stroke and Dementia: A Prospective Cohort Study. Stroke. 2017;48(5):1139-46.
- Kerti L, Witte AV, Winkler A, et al. Higher glucose levels associated with lower memory and reduced hippocampal microstructure. Neurology. 2013;81(20):1746-52.
- Pase MP, Himali JJ, Jacques PF, et al. Sugary beverage intake and preclinical Alzheimer’s disease in the community. Alzheimers Dement. 2017.
- Livesey G, Taylor R, Livesey H, et al. Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies. Am J Clin Nutr. 2013;97(3):584-96.
- Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33(11):2477-83.
- Nichols GA, Hillier TA, Brown JB. Normal fasting plasma glucose and risk of type 2 diabetes diagnosis. Am J Med. 2008;121(6):519-24.
- Onodera Y, Nam JM, Bissell MJ. Increased sugar uptake promotes oncogenesis via EPAC/RAP1 and O-GlcNAc pathways. J Clin Invest. 2014;124(1):367-84.
- Permert J, Ihse I, Jorfeldt L, et al. Pancreatic cancer is associated with impaired glucose metabolism. Eur J Surg. 1993;159(2):101-7.
- Liu H, Huang D, McArthur DL, et al. Fructose induces transketolase flux to promote pancreatic cancer growth. Cancer Res. 2010;70(15):6368-76.
- Tran TT, Naigamwalla D, Oprescu AI, et al. Hyperinsulinemia, but not other factors associated with insulin resistance, acutely enhances colorectal epithelial proliferation in vivo. Endocrinology. 2006;147(4):1830-7.
- Vishnevsky AS, Bobrov Ju F, Tsyrlina EV, et al. Hyperinsulinemia as a factor modifying sensitivity of endometrial carcinoma to hormonal influences. Eur J Gynaecol Oncol. 1993;14(2):127-30.
- Pan F, Hong LQ. Insulin promotes proliferation and migration of breast cancer cells through the extracellular regulated kinase pathway. Asian Pac J Cancer Prev. 2014;15(15):6349-52.
- Jiang Y, Pan Y, Rhea PR, et al. A Sucrose-Enriched Diet Promotes Tumorigenesis in Mammary Gland in Part through the 12-Lipoxygenase Pathway. Cancer Res. 2016;76(1):24-9.
- Higginbotham S, Zhang ZF, Lee IM, et al. Dietary glycemic load and risk of colorectal cancer in the Women’s Health Study. J Natl Cancer Inst. 2004;96(3):229-33.
- Hu J, La Vecchia C, Augustin LS, et al. Glycemic index, glycemic load and cancer risk. Ann Oncol. 2013;24(1):245-51.
- Atkinson RL, Kaiser DL. Effects of calorie restriction and weight loss on glucose and insulin levels in obese humans. J Am Coll Nutr. 1985;4(4):411-9.
- Lenoir M, Serre F, Cantin L, et al. Intense sweetness surpasses cocaine reward. PLoS One. 2007;2(8):e698.
- Goldstein BJ. Insulin resistance as the core defect in type 2 diabetes mellitus. Am J Cardiol. 2002;90(5a):3g-10g.
- Modan M, Halkin H, Almog S, et al. Hyperinsulinemia. A link between hypertension obesity and glucose intolerance. J Clin Invest. 1985;75(3):809-17.
- Bonner G. Hyperinsulinemia, insulin resistance, and hypertension. J Cardiovasc Pharmacol. 1994;24 Suppl 2:S39-49.
- Abel ED. Myocardial insulin resistance and cardiac complications of diabetes. Curr Drug Targets Immune Endocr Metabol Disord. 2005;5(2):219-26.
- Laakso M, Kuusisto J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol. 2014;10(5):293-302.
- Salonen JT, Lakka TA, Lakka HM, et al. Hyperinsulinemia is associated with the incidence of hypertension and dyslipidemia in middle-aged men. Diabetes. 1998;47(2):270-5.
- Despres JP, Lamarche B, Mauriege P, et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Engl J Med. 1996;334(15):952-7.
- Gerstein HC, Pais P, Pogue J, et al. Relationship of glucose and insulin levels to the risk of myocardial infarction: a case-control study. J Am Coll Cardiol. 1999;33(3):612-9.
- Hosszúfalusi N, Pánczél P, Jánoskuti L. Hyperinsulinemia Predicts Coronary Heart Disease Risk in Healthy Middle-Aged Men. Circulation. 1999;100(24):e118-e.
- Luchsinger JA, Tang MX, Shea S, et al. Hyperinsulinemia and risk of Alzheimer disease. Neurology. 2004;63(7):1187-92.
- Fishel MA, Watson GS, Montine TJ, et al. Hyperinsulinemia provokes synchronous increases in central inflammation and beta-amyloid in normal adults. Arch Neurol. 2005;62(10):1539-44.
- Willette AA, Xu G, Johnson SC, et al. Insulin resistance, brain atrophy, and cognitive performance in late middle-aged adults. Diabetes Care. 2013;36(2):443-9.
- Willette AA, Johnson SC, Birdsill AC, et al. Insulin resistance predicts brain amyloid deposition in late middle-aged adults. Alzheimers Dement. 2015;11(5):504-10.e1.
- Nilsen TI, Vatten LJ. Prospective study of colorectal cancer risk and physical activity, diabetes, blood glucose and BMI: exploring the hyperinsulinaemia hypothesis. Br J Cancer. 2001;84(3):417-22.
- Balkau B, Kahn HS, Courbon D, et al. Hyperinsulinemia predicts fatal liver cancer but is inversely associated with fatal cancer at some other sites: the Paris Prospective Study. Diabetes Care. 2001;24(5):843-9.
- Selvin E, Parrinello CM, Sacks DB, et al. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med. 2014;160(8):517-25.
- Alvarado J, Schoenlau F, Leschot A, et al. Delphinol(R) standardized maqui berry extract significantly lowers blood glucose and improves blood lipid profile in prediabetic individuals in three-month clinical trial. Panminerva Med. 2016;58(3 Suppl 1):1-6.
- Hidalgo J, Flores C, Hidalgo MA, et al. Delphinol(R) standardized maqui berry extract reduces postprandial blood glucose increase in individuals with impaired glucose regulation by novel mechanism of sodium glucose cotransporter inhibition. Panminerva Med. 2014;56(2 Suppl 3):1-7.

