Life Extension Magazine®
For many people, strict adherence to brushing and flossing twice daily may not be enough. The consequence is deterioration of gums and teeth with invariable periodontal disease.1,2
Researchers have discovered a unique solution to ensure healthier gums and teeth as we age. It comes in the form of a targeted probiotic that has been found to work specifically in the mouth. This unique probiotic helps destroy disease-causing bacteria and replaces them with beneficial bacteria that protect teeth and gums.
In a revealing human study, subjects receiving the oral probiotic showed an impressive reduction in indicators of plaque buildup, gingivitis, bleeding gums, and pocket depth between gums and tooth roots.3
Americans have an alarmingly high rate of gum disease. Beyond the potential for tooth loss, gum disease is associated with health problems throughout the entire body, including cardiovascular, brain, kidney, and bone diseases.4-10
A major factor in the development of tooth and gum disease is an imbalance in the normal oral microbial community of the mouth, in which disease-causing organisms overwhelm those that contribute to good health.
Researchers have discovered a targeted oral probiotic that is able to “safeguard” the oral cavity, help minimize bad bacteria, and replace it with beneficial bacteria instead.
Studies have shown that oral probiotics improve gum health and reduce risk factors for dangerous periodontal (gum) disease. That risk reduction, in turn, translates into substantially lower risk for a host of systemic disease processes commonly associated with aging.11
How Oral Health Impacts the Entire Body

Disorders involving the teeth are among the most common health problems in US adults, with 96% of those 65 and older having cavities in their permanent teeth and about 20% of adults 65 and older having untreated tooth decay.12
Periodontal (gum) disease is an even more serious and potentially dangerous problem in aging adults.13 More than 70% of adults 65 and older have periodontitis, a term that includes a range of conditions from simple gingivitis (inflammation of the gums without destruction of bone or tooth structures) to aggressive periodontitis, which can lead to bone loss, weakening of the ligaments that hold teeth in place, and eventual tooth loss.
The consequences of periodontal disease are grave, and considerably more threatening than dental cavities. And, while many have to face the expense of dental work or dentures, tooth loss alone can lead to serious malnutrition as the act of chewing becomes increasingly difficult.14,15
What many people might not know is that periodontal disease is a major threat to health throughout the body.10,16
The degree of periodontal inflammation and the presence of pathogenic bacteria has long been linked to coronary artery disease and atherosclerosis.4,17-19 Periodontal pathology also contributes to:
- Cancers of the oral cavity and other regions caused chronic infections and inflammation.5-6
- Alzheimer’s disease and other forms of dementia as a result of inflammatory changes. Accumulation of neuron-destroying amyloid beta increases in adults with periodontal disease.16,20
- A variety of lung disorders, which are associated with periodontal disease, including pneumonia and chronic obstructive pulmonary disease (COPD).21-23
- Nonalcoholic fatty liver disease (NAFLD) and viral hepatitis, which are likely to be associated with inflammatory periodontal disease.24,25
- Kidney diseases, including renal insufficiency and chronic kidney disease, show close associations with periodontal problems.26,27
The Underlying Cause of Gum Disease
How can something as seemingly simple as gum disease have such potentially drastic health effects throughout the body? The answer comes down to one of the underlying causes of gum disease, which is the excessive growth of pathogenic (disease-causing) organisms in the oral cavity. This creates the twin threats of infection and inflammation, which feed on each other in a vicious cycle and can have disastrous effects on many body systems.28
Present in everyone, the oral microbiome, is a complex set of interacting microbial populations, which when in a healthy balance, support and protect the delicate mucous membranes as well as the surfaces of the teeth themselves.29
Shifts in the normal microbial community, however, lead to a host of problems, ranging from dental caries (“cavities”) that arise from excessive acid-producing bacteria, to gum disease that contributes to tooth loss and diseases in parts of the body far removed from the mouth itself.30
Our growing recognition of both the severity of periodontal disease and its relationship to an imbalance in the oral microbial populations have led to calls for use of oral probiotics as effective preventive measures, in an effort to re-establish a healthy microbial community in the mouth.30,31 The results are extremely promising.
What You Need to Know
 |
Oral Probiotic for Gum Disease
- Poor oral health is common among US adults, with the bulk of the impact on older adults.
- Poor oral hygiene leaves individuals vulnerable to an imbalance of the billions of microbes living in our mouths, allowing formation of plaque, development of inflammation, and eventually gum disease and tooth loss.
- As gum disease (periodontitis) progresses, it can have disastrous effects on other organ systems, including the heart, brain, lungs, kidneys, and bones, as a result of the chronic, low-grade inflammation it causes.
- Rebalance oral microbial population through the use of a novel probiotic bacterial strain, S. salivarius BLIS M18.
- Studies show that regular supplementation with S. salivarius BLIS M18 results in significant improvements in measures of oral and gum health.
- The addition of a second probiotic organism, Bacillus coagulans GBI-30, 6086, provides extra support against the germ most commonly associated with dental caries.
- Oral health is much more than a cosmetic consideration. To sustain healthy teeth, gums, and total body health, it’s time to include a daily supplement with these powerful beneficial probiotic organisms.
Beneficial Organisms Destroy Dangerous Germs
The principle behind all probiotics is simple: Replace unhealthful or dangerous organisms with those that contribute directly or indirectly to human health. The end result should be a reduction in the population of the “bad guys,” and the establishment of a more protective environment.
S. salivarius strain BLIS M18 is one of the “good guys.” It competes with dangerous oral bacteria that cause or exacerbate periodontal disease, and has been shown to prevent and improve parameters of gingivitis and periodontitis.9 It accomplishes this through numerous mechanisms of action.
First, S. salivarius produces enzymes that help break down dental plaque, which is a major threat to both tooth and gum health.32 Plaque is the sticky film of bacteria that forms on teeth, and it’s the main cause of tooth decay and gum disease. When plaque hardens, it becomes tartar, a mineralized substance with a rough surface that can become home to still more plaque and more dangerous microbes.
Another benefit of S. salivarius is that it has been shown to neutralize acids to maintain a healthy oral pH. A healthy oral pH is important because having a low pH demineralizes teeth, which creates an environment in which bad bacteria thrive.32,33
Unlike many other probiotic formulations, S. salivarius is capable of colonizing the mouth and gums (rather than simply sticking around until the entire applied dose is gone).32,34 Once it has established its colonies in the mouth, S. salivarius competes with the harmful bacteria that cause tooth decay and periodontal disease to reduce their relative abundance.
It accomplishes this as a result of its ability to secrete bacteriocin-like inhibitory substances (BLIS) known as lantibiotics. Technically, lantibiotics are bacterially produced antimicrobial substances that kill competing organisms, but think of them as the weapons the bacterium uses to keep less savory organisms at bay.35 And although S. salivarius is a common bacteria in the mouth, the more beneficial BLIS strains are only found in 2% of individuals.36
Laboratory studies show that colonies of S. salivarius-producing lantibiotics can inhibit the growth of oral disease-causing bacteria associated with periodontitis.37-39
One important study showed that in addition to inhibiting the growth of dangerous bacteria, S. salivarius BLIS M18 can also reduce levels of inflammatory cytokines associated with gingivitis and periodontitis.41 This is an important characteristic in breaking the infection-inflammation-infection cycle that accelerates gum disease and threatens the rest of the body.
 |
Systemic Disease Can Emanate in the Mouth
In many ways, the mouth is the first line of defense against disease. According to the National Institutes of Health:
“The mouth is also a portal of entry for pathogens and toxins, which can affect the mouth and, if not cleared by the many defense mechanisms that have evolved to protect the oral cavity, may spread to the rest of the body.”40
Oral Probiotic Improves Gum Disease
Once scientists knew that oral probiotics produced such beneficial antibacterial actions in lab and preclinical studies, they were ready to test their effects in real life. A number of human trials have now been completed, with exciting results that demonstrate the positive impact of regular supplementation with an oral probiotic.
A randomized, controlled clinical trial was conducted to determine the effects of S. salivarius BLIS M18 on a number of the most important clinical parameters of periodontal health. This study evaluated indicators that dental hygienists use to determine the health of gums:3
- Plaque index score: a 0-to-3 scale ranging from no plaque to an abundance of soft matter within the gingival pocket (the pocket of soft tissue between gum and tooth).42
- Gingival index score: a 0-to-3 scale ranging from normal gingiva (gums) to severe inflammation with marked redness and swelling, including ulceration and tendency of spontaneous bleeding.43
- Sulcular bleeding index: a 0-to-5 score grading tendency of the gums to bleed on probing, ranging from healthy-looking gums with no bleeding on probing to spontaneous bleeding, change in color, and marked swelling.43
- Probing pocket depth: the depth to which a dental probe can be passed between the inner margin of the gum and the tooth root. The deeper the pocket depth, the worse the evidence of periodontal disease.44
The study involved both male and female patients with moderate and severe gingivitis (scores of 2 or 3 on gingival index score), and moderate periodontitis (probing pocket depth of up to 6 mm). In order to optimize the subjects’ periodontal health, subjects underwent a thorough cleaning and scraping of the teeth to remove plaque and tartar at the outset of the study.
After the initial visit, half of the subjects received a lozenge containing S. salivarius BLIS M18, while the other half received no treatment, acting as a control group. The subjects took lozenges daily for 30 days, though the researchers observed them for a total of 60 days in order to determine if the supplement would continue to have beneficial effects after subjects stopped taking it.
In all four parameters measured, the supplemented group showed improvement over the control group at 30 days—with continued benefits even at 60 days.
- The plaque index score was reduced by 44% by day 30, and by 37% at day 60.
- The gingival index score was reduced by 42% by day 30, and by 35% at day 60.
- The sulcular bleeding index score was reduced by 53% at day 30, and by 51% at day 60.
- The probing pocket depth decreased by 20% by day 30, and by 22% at day 60.
This study demonstrated the ability of the probiotic lozenge to significantly improve all four of the commonly used assessments of periodontal health. S. salivarius BLIS M18’s ability to colonize the oral cavity contributed to the sustained benefits seen even after the supplementation period ended.
Don’t Stop Brushing and Flossing
 |
Most people find it difficult to comply with the American Dental Association’s recommendation for twice-daily brushing and at least once daily interdental cleansing (using floss or a water flosser), even though adherence to these recommendations has been shown to support better tooth and gum health.47
That’s why the advent of a powerful oral probiotic lozenge to sustain and improve the health of the oral microbial community is a genuine breakthrough in medical and dental care.
But don’t stop aggressive oral cleansing with a brush, and continue or increase the use of an interdental cleaner. These activities can work in tandem with the new, healthier oral microbial community to suppress plaque and maintain healthy gums.
Further Reduce Tooth Decay and Inflammation
A companion organism has been identified that provides additional oral health support to S. salivarius BLIS M18.
This probiotic strain called Bacillus coagulans has been shown to competitively inhibit the growth of Streptococcus mutans, a bacterium that contributes to tooth decay.45
A patented strain of this organism, GBI-30, 6086 (GanedenBC30®) helps increase the body’s natural resistance to pathogenic organisms by boosting the immune system and reducing production of inflammatory cytokines that promote the inflammatory response.46
Suggested Usage
 |
To emulate the successful clinical findings described in this article, make an appointment with your dentist for a thorough cleaning and scraping of your teeth to remove plaque and tartar. This will help reduce colonies of dangerous bacteria your mouth harbors.
Then immediately initiate daily use of a lozenge containing S. salivarius and Bacillus coagulans.
Based on the clinical study results, some people may only need to use this lozenge every other month.
Those with serious oral health issues should consider using the lozenge continuously at least until clinical and symptomatic improvements in oral health manifest.
The objective is to rebalance the communities of bacteria that live in your mouth, promoting not just improved oral health, but the health of the entire body.
Summary
Poor oral health is widespread among maturing individuals, with the highest rates of gum disease prevailing among older adults. Gum disease leads to tooth loss and expenses related to dental work and dentures.
Worse than tooth loss, however, are the total body health implications of gum disease. The chronic presence of inflamed tissue contributes to the chronic, low-grade inflammation associated with so many of the disorders we associate with aging, including cancer, cardiovascular, brain, kidney, and bone diseases.
A major factor in the development of tooth and gum disease is an imbalance in the normal oral microbial community of the mouth, in which disease-causing organisms predominate and sideline those that contribute to good health.
By rebalancing the oral microbial community with S. salivarius strain BLIS M18, individuals can turn the tables on the pathogens in the mouth, marginalizing them and allowing healthy organisms to predominate. This natural probiotic strain produces powerful lantibiotics, which are germ-killing molecules that act locally within the mouth to suppress more harmful germs.
Studies show that regular supplementation with S. salivarius BLIS M18 can improve multiple measures of gum health and reduce inflammation in the oral cavity. Further inflammation control is provided by addition of beneficial Bacillus coagulans another probiotic strain that inhibits the germs that cause dental caries and helps to reduce the inflammatory response.
If you have any questions on the scientific content of this article, please call a Life Extension® Health Advisor at 1-866-864-3027.
Healthy and Diseased Teeth and Gums
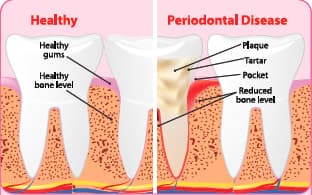 |
Left: Healthy teeth and gums, with a “bud” of robust, gum tissue rising above a strong, healthy bone. Note the absence of a “pocket” adjacent to the tooth, indicating a strong attachment. Right: Teeth and gums in periodontal disease. Note accumulated plaque (a biofilm containing protein and infectious microbes), tartar (hardened plaque), and a periodontal pocket where diseased gum tissue is pulled away from the tooth root. Inflamed gums bleed readily, and their attachment to the tooth root weakens. Still worse, chronic inflammation at the site causes bone resorption, leading to reduced bone level around the tooth root. Studies show that periodontitis leads to diseases associated with aging throughout the body.
References
- Ramsay DS. Patient compliance with oral hygiene regimens: a behavioural self-regulation analysis with implications for technology. Int Dent J. 2000;Suppl Creating A Successful:304-11.
- Bakdash B. Oral hygiene and compliance as risk factors in periodontitis. J Periodontol. 1994 May;65(5 Suppl):539-44.
- Scariya L, Nagarathna DV, Varghese M. Probiotics in periodontal therapy. Int J Pharm Bio Sci. 2015 Jan;6(1):242-50.
- Yu YH, Chasman DI, Buring JE, et al. Cardiovascular risks associated with incident and prevalent periodontal disease. J Clin Periodontol. 2015 Jan;42(1):21-8.
- Ahmed U, Tanwir F. Association of periodontal pathogenesis and cardiovascular diseases: a literature review. Oral Health Prev Dent. 2015;13(1):21-7.
- Yao QW, Zhou DS, Peng HJ, et al. Association of periodontal disease with oral cancer: a meta-analysis. Tumour Biol. 2014 Jul;35(7):7073-7.
- Rajesh KS, Thomas D, Hegde S, et al. Poor periodontal health: A cancer risk? J Indian Soc Periodontol. 2013 Nov;17(6):706-10.
- Bascones-Martinez A, Gonzalez-Febles J, Sanz-Esporrin J. Diabetes and periodontal disease. Review of the literature. Am J Dent. 2014 Apr;27(2):63-7.
- Stanko P, Izakovicova Holla L. Bidirectional association between diabetes mellitus and inflammatory periodontal disease. A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(1):35-8.
- Nagpal R, Yamashiro Y, Izumi Y. The Two-Way Association of Periodontal Infection with Systemic Disorders: An Overview. Mediators Inflamm. 2015;2015:793898.
- Zarco MF, Vess TJ, Ginsburg GS. The oral microbiome in health and disease and the potential impact on personalized dental medicine. Oral Dis. 2012 Mar;18(2):109-20.
- Dye B, Thornton-Evans G, Li X, et al. Dental caries and tooth loss in adults in the United States, 2011-2012. NCHS Data Brief. 2015 May;(197):197.
- Thornton-Evans G, Eke P, Wei L, et al. Periodontitis among adults aged ≥30 years - United States, 2009-2010. MMWR Surveill Summ. 2013 Nov 22;62 Suppl 3:129-35.
- Andreas Zenthöfer A, Rammelsberg P, Cabrera T, et al. Prosthetic rehabilitation of edentulism prevents malnutrition in nursing home residents. Int J Prosthodont. 2015 Mar-Apr;28(2):198-200.
- Poisson P, Laffond T, Campos S, et al. Relationships between oral health, dysphagia and undernutrition in hospitalised elderly patients. Gerodontology. 2014 Mar 11.
- Watts A, Crimmins EM, Gatz M. Inflammation as a potential mediator for the association between periodontal disease and Alzheimer’s disease. Neuropsychiatr Dis Treat. 2008 Oct;4(5):865-76.
- Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015 Jan;15(1):30-44.
- Saffi MA, Furtado MV, Polanczyk CA, et al. Relationship between vascular endothelium and periodontal disease in atherosclerotic lesions: Review article. World J Cardiol. 2015 Jan 26;7(1):26-30.
- Suwandecha T, Srichana T, Balekar N, et al. Novel antimicrobial peptide specifically active against Porphyromonas gingivalis. Arch Microbiol. 2015 Sep;197(7):899-909.
- Kamer AR, Pirraglia E, Tsui W, et al. Periodontal disease associates with higher brain amyloid load in normal elderly. Neurobiol Aging. 2015 Feb;36(2):627-33.
- Prasanna SJ. Causal relationship between periodontitis and chronic obstructive pulmonary disease. J Indian Soc Periodontol. 2011 Oct;15(4):359-65.
- Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann Periodontol. 2003 Dec;8(1):54-69.
- Liu Z, Zhang W, Zhang J, et al. Oral hygiene, periodontal health and chronic obstructive pulmonary disease exacerbations. J Clin Periodontol. 2012 Jan;39(1):45-52.
- Nagao Y, Kawahigashi Y, Sata M. Association of periodontal diseases and liver fibrosis in patients with HCV and/or HBV infection. Hepat Mon. 2014 Dec;14(12):e23264.
- Yoneda M, Naka S, Nakano K, et al. Involvement of a periodontal pathogen, Porphyromonas gingivalis on the pathogenesis of non-alcoholic fatty liver disease. BMC Gastroenterol. 2012;12:16.
- Kshirsagar AV, Moss KL, Elter JR, et al. Periodontal disease is associated with renal insufficiency in the Atherosclerosis Risk In Communities (ARIC) study. Am J Kidney Dis. 2005 Apr;45(4):650-7.
- Fisher MA, Taylor GW, West BT, et al. Bidirectional relationship between chronic kidney and periodontal disease: a study using structural equation modeling. Kidney Int. 2011 Feb;79(3):347-55.
- Mawardi HH, Elbadawi LS, Sonis ST. Current understanding of the relationship between periodontal and systemic diseases. Saudi Med J. 2015 Feb;36(2):150-8.
- Zaura E, Nicu EA, Krom BP, et al. Acquiring and maintaining a normal oral microbiome: current perspective. Front Cell Infect Microbiol. 2014;4:85.
- Bizzini B, Pizzo G, Scapagnini G, et al. Probiotics and oral health. Curr Pharm Des. 2012;18(34):5522-31.
- Saha S, Tomaro-Duchesneau C, Tabrizian M, et al. Probiotics as oral health biotherapeutics. Expert Opin Biol Ther. 2012 Sep;12(9):1207-20.
- Burton JP, Drummond BK, Chilcott CN, et al. Influence of the probiotic Streptococcus salivarius strain M18 on indices of dental health in children: a randomized double-blind, placebo-controlled trial. J Med Microbiol. 2013 Jun;62(Pt 6):875-84.
- Loesche WJ. Microbiology of Dental Decay and Periodontal Disease. Medical Microbiology. 4th edition. Galveston (TX):University of Texas Medical Branch at Galveston; 1996.
- Heng NC, Haji-Ishak NS, Kalyan A, et al. Genome sequence of the bacteriocin-producing oral probiotic Streptococcus salivarius strain M18. J Bacteriol. 2011 Nov;193(22):6402-3.
- Wescombe PA, Upton M, Renault P, et al. Salivaricin 9, a new lantibiotic produced by Streptococcus salivarius. Microbiology. 2011 May;157(Pt 5):1290-9.
- Burton J, Chilcott C, Wescombe P, et al. Extended Safety for the Oral Cavity Probiotic Streptococcus Salivarius K12. Probiotics & Antimicro Prot. 2010;2:135-44.
- Barbour A, Philip K, Muniandy S. Enhanced production, purification, characterization and mechanism of action of salivaricin 9 lantibiotic produced by Streptococcus salivarius NU10. PLoS One. 2013;8(10):e77751.
- Fiedler T, Riani C, Koczan D, et al. Protective mechanisms of respiratory tract Streptococci against Streptococcus pyogenes biofilm formation and epithelial cell infection. Appl Environ Microbiol. 2013 Feb;79(4):1265-76.
- Santagati M, Scillato M, Patane F, et al. Bacteriocin-producing oral streptococci and inhibition of respiratory pathogens. FEMS Immunol Med Microbiol. 2012 Jun;65(1):23-31.
- Available at: http://www.nidcr.nih.gov/datastatistics/surgeongeneral/sgr/part3.htm. Accessed October 2, 2015.
- Adam E JM, Seney S, Summers K, et al. Streptococcus salivarius K12 and M18 probiotics reduce periodontal pathogen-induced inflammation. IADR/AADR/CADR 89th General Session and Exhibition, 16-19 March 2011. Vol San Diego, CA, USA.2011.
- Available at: https://www.mah.se/capp/methods-and-indices/oral-hygiene-indices/silness-loe-index. Accessed October 5, 2015.
- Available at: http://www.intechopen.com/books/gingival-diseases-their-aetiology-prevention-and-treatment/gingival-indices-state-of-art. Accessed October 5, 2015.
- Available at: http://www1.umn.edu/perio/dds6112/02b-probe.pdf. Accessed October 5, 2015.
- Jindal G, Pandey RK, Agarwal J, et al. A comparative evaluation of probiotics on salivary mutans streptococci counts in Indian children. Eur Arch Paediatr Dent. 2011 Aug;12(4):211-5.
- Baron M. A patented strain of Bacillus coagulans increased immune response to viral challenge. Postgrad Med. 2009 Mar;121(2):114-8.
- Available at: http://www.ada.org/en/press-room/news-releases/2013-archive/august/american-dental-association-statement-on-regular-brushing-and-flossing-to-help-prevent-oral. Accessed October 5, 2015.

