Life Extension Magazine®

Most people associate heart attack with coronary artery blockage. Yet 50% of cardiovascular deaths originate from a condition called sudden cardiac arrest, which is the unexpected acute loss of heart function.1
Sudden cardiac arrest is usually caused by an electrical disturbance that disrupts the heart’s rhythmic pumping action. When cardiac arrest happens, blood flow to the entire body stops.2
If not immediately treated, sudden cardiac arrest results in cessation of life. Survival rates remain low despite modern resuscitation attempts.3
In a groundbreaking 2014 study, researchers measured testosterone and estrogen levels to correlate risk of sudden cardiac arrest. The findings revealed that lower levels of testosterone or higher levels of estrogen in men were strongly associated with greater risk of sudden cardiac arrest.4
These revelations are significant because they provide a basis to identify men at risk for sudden cardiac arrest and implement preventative treatments, such as boosting deficient testosterone and suppressing excess estrogen.
Life Extension® members should not be surprised at these findings. They know we’ve been testing testosterone and estradiol blood levels in men for the past 19 years.
Standing in our way of saving more lives is the FDA, who continues to discourage hormone balance in aging men despite overwhelming data showing reduction in heart attack risk.4,5
What the FDA and conventional medical community still do not comprehend is that when natural testosterone is administered to men, it is imperative that estradiol blood levels be tested to ensure that the testosterone is not converting to excess estrogen. Failure to grasp this simple blood testing concept may be causing over 100,000 needless American deaths each year.
Each year in the United States, out-of-hospital sudden cardiac arrest strikes more than 350,000 people, or about 1,000 per day.6 Men account for 75% of these cases. Only 5% of those stricken survive.1,7
Magnesium and potassium are critically involved in regulating the heart’s electrical signaling.
Deficiency of these minerals (magnesium or potassium) predisposes humans to sudden cardiac arrest.8-11
Each heartbeat is controlled by the opening and closing of mineral “channels” in cardiac cells.12
Testosterone plays a role in modulating potassium channels, which regulate the flow of potassium between the bloodstream and cardiac cells.13 Testosterone regulates calcium channels, preventing too much blood calcium from entering cardiac cells.14 Magnesium also protects against excess calcium channel infiltration.15,16
Low
testosterone
is associated with abnormal EKG readings that predispose people to
sudden
cardiac arrest
.17-20
In a first-of-its-kind study, men with higher testosterone were found to be 25% less likely to suffer sudden cardiac arrest. This same study found that men with higher estradiol levels suffered twice the risk of sudden cardiac arrest.4
The significance of this landmark study is that it ties together a puzzle that has baffled conventional cardiology for decades. To put the data from the study in perspective, a mere 23% increase in median testosterone level was associated with a 25% reduction in sudden cardiac arrest. Just a 31% increase in median level of estradiol doubled risk of sudden cardiac arrest.
This data corroborates a large body of previously published research linking low testosterone and/or excess estrogen21 to sharply higher rates of overall cardiovascular disease.22-29
What Happens In Cardiac Arrest?

Coronary artery disease is associated with the majority of sudden cardiac arrests.1 Even temporary blockage of a coronary artery can create an electrical disruption that results in acute heart failure.
While the term “arrest” implies stoppage of the heart, what usually happens first in sudden cardiac arrest is that the heart loses its rhythmic ability to pump blood, which is medically termed ventricular fibrillation.30 The result of ventricular fibrillation is uncoordinated rapid beating of the hearts chambers, loss of blood flow and blood pressure. Death quickly follows unless a defibrillator timely restores normal heart rhythm.
If cardiac arrest is caused by a blocked coronary artery, emergency surgery is required to insert a stent or bypass the occluded artery.
Conclusions From The Testosterone Review Published By The American Heart Association
 |
The American Heart Association commissioned a review of previously published studies to evaluate the role that testosterone might play on cardiovascular disease risk. Here are excerpts from the Concluding Summary of the American Heart Association’s review:31
“Low endogenous bioavailable testosterone levels have been shown to be associated with higher rates of all cause and cardiovascular-related mortality. Patients suffering from coronary artery disease, congestive heart failure, type II diabetes, and obesity have all been shown to have lower levels of endogenous testosterone compared with those in healthy controls. In addition, the severity of coronary artery disease and congestive heart failure correlates with the degree of testosterone deficiency."
“Testosterone replacement therapy has also been shown to improve the homeostatic model of insulin resistance and hemoglobin A1c in diabetics and to lower the BMI in obese patients."
“These findings suggest that men with lower levels of endogenous testosterone may be at a higher risk of
developing atherosclerosis."
“This review article has demonstrated that normal testosterone levels play an important role in maintaining cardio-vascular health, and testosterone replacement therapy in men with hypogonadism improves obesity, type II diabetes, myocardial ischemia, exercise capacity, and QTc length.”
American Heart Association Analysis
At the end of 2013, a meticulous examination of studies relating to testosterone and cardiovascular disease was published in the Journal of the American Heart Association.
The findings from this analysis corroborate much of what you’ve read in Life Extension® magazine over the past three decades.
According to this review conducted on behalf of the American Heart Association, low levels of testosterone in men are associated with:31
- Greater risk of developing coronary artery disease
- More severe atherosclerosis
- Type II diabetes
- Increased visceral adiposity (belly fat)
- Metabolic syndrome
- Insulin resistance
- Carotid artery stenosis (narrowing)
- Obesity
- Abnormal EKG (electrocardiogram) tests
- Angina pectoris (chest pain caused by reduced blood flow to the heart)32
- Reduced arterial dilation (caused by impairment of calcium and potassium channels)
- Increased body mass index
- More severe congestive heart failure
- Higher rates of all-cause and cardiac mortality (death)
What impressed me about this American Heart Association analysis is that it also reviewed studies that failed to show a benefit to testosterone and identified flaws that rendered the findings highly questionable. Life Extension® has previously published many articles exposing similar flaws caused by improper testosterone prescribing practices.33-36
These findings suggest common causes of disability and death in men are related to low testosterone levels. It should be refreshing to longtime Life Extension® supporters that a respected mainstay of conventional medicine, i.e. the American Heart Association, has published this favorable data about testosterone.
You might think this confirmatory report would result in the widespread implementation of testosterone replacement therapy. Instead, an FDA advisory panel is taking steps to restrict the ability of aging men to replenish their testosterone.
Critical Need To Balance Estrogen

The media, FDA, and much of mainstream medicine have misinterpreted the published scientific literature as it relates to testosterone and heart disease risk.37-41 If one looks at studies where testosterone is inappropriately prescribed to men with various cardiovascular risk factors, an increased risk of death has sometimes been observed.42,43
Overlooked is the fact that men at higher risk for vascular disease also have a greater propensity to rapidly convert (aromatize) testosterone to estrogen in their bodies. Excess estrogen in males causes blood platelets to aggregate, which increases the probability of an abnormal blood clot forming in jagged coronary arteries. Heart attacks often occur in response to blood clots that form in coronary arteries44 with unstable atherosclerotic plaque.45-47
A study published in the Journal of the American Medical Association (JAMA) measured blood estradiol (a dominant estrogen) in 501 men with chronic heart failure. Compared to men in the balanced estrogen quintile, men in the lowest estradiol quintile were 317% more likely to die during a three-year follow-up, while men in the highest estradiol quintile were 133% more likely to die.48
The men in the balanced quintile—with the fewest deaths—had serum estradiol levels between 21.80 and 30.11 pg/mL.48 This is virtually the ideal range that Life Extension® has long recommended aging men strive for.
Any man contemplating testosterone restoration or concerned about heart attack risk should test their testosterone and estradiol blood levels. If estradiol levels exceed 30 pg/mL, simple steps can be taken to inhibit the aromatase enzyme that converts testosterone to estrogen. This provides the dual advantage of keeping estrogen levels in optimal ranges while increasing testosterone (since less testosterone is converted to estrogen).
FDA Claims Testosterone May Increase Heart Attack Risk
In early March 2015, the FDA issued an edict regarding testosterone drugs. Labels of testosterone drugs must now carry a warning that testosterone may increase risk of heart attack and stroke.52
This new mandate is based on a FDA advisory panel report that admits there is only a “weak signal of cardiovascular risk” with testosterone use.53
The FDA’s inappropriate new warning will curtail the prescribing of testosterone, limit insurance coverage, and drive up costs to consumers. The consequences to the health and finances of aging men will be devastating (including more sudden cardiac arrests).
The problem we have with the FDA’s findings is that they are based on an egregious misinterpretation of the human data.
An article published in the Journal of the American Medical Association sheds some light on how the FDA advisory committee came to their erroneous conclusion.5 There was not one mention about testing men’s estrogen blood levels prior to prescribing testosterone. In fact, blood tests were omitted so frequently that it comes as no surprise that some men were dangerously overprescribed testosterone.
The FDA advisory panel’s report reveals egregious failures of mainstream physicians to properly prescribe testosterone. According the advisory panel report, 28% of patients were prescribed testosterone without requisite blood testing.5,53
We suspect the number of men being prescribed testosterone without requisite blood testing is substantially higher than the 28% the FDA estimates. This omission by prescribing physicians helps explain why the FDA now wants to curb the use of testosterone. But as you’ll read next, there is a more efficient solution from a cost, safety and practicality standpoint.
Mortality Risks Of Low Testosterone
 |
As men age, testicular production of testosterone markedly declines. This often occurs as aromatase levels increase, especially in the presence of surplus abdominal fat.47 Aromatase is the enzyme that converts testosterone to estrogen.
Low testosterone or excess estrogen in men was shown to elevate risk of sudden cardiac arrest in a recent study.4
The link between low testosterone and cardiovascular disease risk in males was discovered long ago. What follows are descriptions from just a few of many studies supporting this conclusion:
- A study evaluated the relationship between testosterone levels and all-cause mortality over approximately 20 years. Men with low total testosterone levels (under 241 ng/dL) were 40% more likely to die than those with higher levels of testosterone. This finding was consistent regardless of age, lipid levels, and other variables.49
- Another study looked at whether low testosterone levels were associated with an increased risk for mortality in male veterans. Men classified as having a low testosterone level had 88% increased mortality after adjusting for other known mortality factors.50
- A third study examined the relationship between testosterone levels and mortality due to all causes, cardiovascular disease, and cancer. The study included over 11,000 patients aged 40 to 79 years. Low testosterone levels at baseline were significantly associated with increased mortality from cardiovascular disease, cancer, and all causes. After adjustment for variables, an increase of 173 ng/dL of total testosterone was associated with a 19% decreased risk for mortality.51
These studies help corroborate Life Extension®’s long-standing position that low testosterone in males is a significant mortality factor. The take home message is to have one’s blood tested for testosterone and estradiol to enable adjustments to be made based on one’s individual results.
Let Pharmacists Prescribe Testosterone
It never ceases to astound me how backwards conventional doctors are when it comes to prescribing testosterone to their aging male patients.
They almost universally omit testing estradiol, which can place their patients at great risk for heart attack or ischemic stroke.73,74 Many men have found that inches can be taken off their waistline in response to testosterone therapy.75-77 This is important because abdominal (belly) fat secretes lots of aromatase that converts testosterone into estrogens.47,78 Men with estradiol levels over 30 pg/mL should consider a low-dose aromatase-inhibiting drug (like anastrozole) so they can enjoy the benefits of increased testosterone and optimized estradiol.
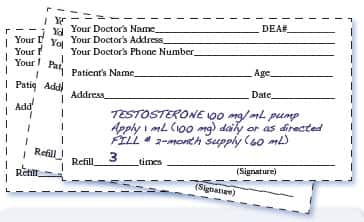
Instead of asking hurried doctors to figure this out, why not let pharmacists review a man’s blood test results and provide the appropriate dose of testosterone cream and an aromatase-inhibiting drug if needed. A pharmacist (or any enlightened individual for that matter) can easily see if red blood cells, PSA, or liver enzymes are excessively elevated and refer the consumer to a physician for additional testing.
This sweeping change would save Americans time and money, and probably spare human lives as pharmacists may wind up doing a better job than untrained physicians that prescribe testosterone with no blood testing. (No one questions the value of having access to a physician with expertise in the prescribing of natural hormones.)
Hormone Balance Requires Proper Blood Tests
Maintaining youthful balance of testosterone, estrogen, progesterone, and DHEA can help forestall the diminished quality of life humans face as they age.
Prescribing testosterone without blood testing exposes men to the following problems:
- Too much or too little testosterone
- Too much or too little estrogen
- Excess red blood cell formation
- Liver injury
- Clinically relevant pre-existing prostate cancer
Testosterone promotes healthy red blood cell formation, which is beneficial for the aging men suffering frank or subclinical anemia.54-57 Men with a condition called polycythemia vera,58,59 which is an overproduction of red blood cells, are advised to avoid testosterone replacement, as are men with severe liver impairment.60,61 Blood testing can readily detect liver problems or overproduction of red blood cells.
Men with testosterone-sensitive prostate cancer should avoid testosterone until their malignancy is brought under control.62 Contrary to erroneous reports the media ignorantly disseminates, higher testosterone levels do not increase prostate cancer risk.63-72 PSA blood tests can reveal the status of one’s prostate gland.
Men with high blood estradiol (estrogen) levels should take an aromatase-inhibiting drug like anastrozole (0.5 mg twice a week) to bring estradiol into optimal range (20 to 30 pg/mL). This is critically important even if a man chooses not to initiate testosterone replacement.
Here are the optimal blood levels of testosterone, estradiol and other relevant markers men should strive for:
Total Testosterone: 700-900 ng/dL
Free Testosterone: 20-25 pg/mL
Estradiol: 20-30 pg/mL
PSA: Under 2.5 (the lower the better)
Red Blood Cells: Within normal reference ranges
Liver enzymes: Within normal reference ranges
All of these measurements are included in the comprehensive Male Panel blood test that many Life Extension® members have done annually. (Call 1-800-208-3444 to order.)
How Many Lives Are Being Lost?
Each year, 263,000 men perish from sudden cardiac arrest in America. It remains a leading cause of death.1
A recent finding (corroborated by previous published studies) indicates a substantial percentage of these deaths can be avoided if men just modestly restore youthful hormone balance, i.e. increase deficient testosterone and reduce excess estradiol.4,79-82
Standing in the way of this scientific rationality is a slew of state and federal regulations that drives up costs and creates bureaucratic inefficiencies.
The only way of knowing one’s individual hormone status is to test for it. This is not something that can be guessed, and 95% of those stricken with sudden cardiac arrest don’t get a second chance to take corrective actions.
The financial impediment precluding more men from using topical testosterone cream is its high cost. The most popular name brand of topical testosterone (Androgel®) costs around $430 per month. Fortunately, compounding pharmacies make similar potency testosterone creams for under $35 a month. Both these prices ($430 and $35) are far too high and reflect regulatory costs rather than non-patented testosterone, which costs very little.
Instead of revolting against regulatory burdens that cause drugs to be extortionately overpriced, Americans languish in state of apathy while pharmaceutical companies collude to pillage our finances.
Life Extension® long ago broke down some of these barriers by enabling members to gain direct and convenient access to low-cost blood test panels.
Annual Blood Test Super Sale

High prices charged by commercial labs for comprehensive blood testing preclude most people from having them done. The tragic result is that most aging humans needlessly suffer the ill effects of hormone imbalances.
Life Extension® circumvents these price barriers by offering Male and Female Blood Test Panels at the lowest prices anywhere. Once a year, we discount the popular Male and Female Blood Test Panels to only $199—far less than what commercial labs charge.
The Blood Test Super Sale ends June 1, 2015, so please place your order before then to take advantage of these extra discounted prices. You can have your blood drawn any time after receiving your requisition kit.
The results of your blood tests are rapidly sent directly to you. If you have any questions, you are welcome to call our Health Advisor helpline.
The Most Effective Way To Live Longer
Annual blood testing is the single most effective method of detecting abnormalities before they lead to serious illness or death. A call to 1-800-208-3444 is all you have to do to order these comprehensive tests at extra discounted prices.
For longer life,
William Faloon
P.S.—Sex hormone balance is so critical to the health of aging men that in this issue of Life Extension® magazine, we reprint a rebuttal we published last year to a flawed study being used by the FDA to warn aging men against usingtestosterone.83,84
We also have a chapter from a brand new book on testosterone authored by Harvard professor Abraham Morgantaler, MD, along with a review of another new book on testosterone replacement therapy authored by John Crisler, DO.
References
- Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998 Nov 24;98(21):2334-51. Review.
- Finch NJ, Leman RB. Clinical trials update: sudden cardiac death prevention by implantable device therapy. Crit Care Nurs Clin North Am. 2005 Mar;17(1):33-8.
- Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008 Sep 24;300(12):1423-31.
- Narayanan K, Havmoeller R, Reinier K, et al. Sex hormone levels in patients with sudden cardiac arrest. Heart Rhythm. 2014 Dec;11(12):2267-72.
- Garnick MB. Testosterone replacement therapy faces FDA scrutiny. JAMA. 2015 Feb 10;313(6):563-4.
- Available at: http://www.heart.org/heartorg/cprandecc/whatiscpr/cprfactsandstats/cpr-statistics_ucm_307542_article.jsp. Accessed March 27, 2015.
- Mehra R. Global public health problem of sudden cardiac death. J Electrocardiol. 2007 Nov-Dec;40(6 Suppl):S118-22.
- Johnson CJ, Peterson DR, Smith EK. Myocardial tissue concentrations of magnesium and potassium in men dying suddenly from ischemic heart disease. Am J Clin Nutr. 1979 May;32(5):967-70.
- Fiset C, Kargacin ME, Kondo CS, Lester WM, Duff HJ. Hypomagnesemia: characterization of a model of sudden cardiac death. J Am Coll Cardiol. 1996 Jun;27(7):1771-6.
- Dyckner T, Wester PO. Potassium/magnesium depletion in patients with cardiovascular disease. Am J Med. 1987 Mar 20;82(3A):11-7.
- Schulman M, Narins RG. Hypokalemia and cardiovascular disease. Am J Cardiol. 1990 Mar 6;65(10):4E-9E.
- Kebler M, Just S, Rottbauer W. Ion flux dependent and independent functions of ion channels in the vertebrate heart: lessons learned from zebrafish. Stem Cells Int. 2012;2012:462161.
- Jones RD, Pugh PJ, Jones TH, Channer KS. The vasodilatory action of testosterone: a potassium-channel opening or a calcium antagonistic action? Br J Pharmacol. 2003 Mar;138(5):733-44. Review.
- Scragg JL, Jones RD, Channer KS, Jones TH, Peers C. Testosterone is a potent inhibitor of L-type Ca(2+) channels. Biochem Biophys Res Commun. 2004 May 28;318(2):503-6.
- Mert T, Gunes Y, Guven M, Gunay I, Ozcengiz D. Effects of calcium and magnesium on peripheral nerve conduction. Pol J Pharmacol. 2003 Jan-Feb;55(1):25-30.
- Altura BM, Altura BT. Microcirculatory actions and uses of naturally occurring (magnesium) and novel synthetic calcium channel blockers. Microcirc Endothelium Lymphatics. 1984 Apr;1(2):185-220. Review.
- Zhang Y, Ouyang P, Post WS, et al. Sex-steroid hormones and electrocardiographic QT-interval duration: findings from the third National Health and Nutrition Examination Survey and the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2011 Aug 15;174(4):403-11.
- Pecori Giraldi F, Toja PM, Filippini B, et al. Increased prevalence of prolonged QT interval in males with primary or secondary hypogonadism: a pilot study. Int J Androl. 2010 Feb;33(1):e132-8.
- Chugh SS, Reinier K, Singh T, et al. Determinants of prolonged QT interval and their contribution to sudden death risk in coronary artery disease: the Oregon Sudden Unexpected Death Study. Circulation. 2009 Feb 10;119(5):663-70.
- Straus SM, Kors JA, De Bruin ML, et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol . 2006 Jan 17; 47(2):362-7.
- Phillips GB, Castelli WP, Abbott RD, McNamara PM. Association of hyperestrogenemia and coronary heart disease in men in the Framingham cohort. Am J Med. 1983 May;74(5):863-9.
- Hak AE, Witteman JC, de Jong FH, et al. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab. 2002 Aug;87(8):3632-9.
- Dobrzycki S, Serwatka W, Nadlewski S, et al. An assessment of correlations between endogenous sex hormone levels and the extensiveness of coronary heart disease and the ejection fraction of the left ventricle in males. J Med Invest. 2003 Aug;50(3-4):162-9.
- Jones RD, Nettleship JE, Kapoor D, Jones HT, Channer KS. Testosterone and atherosclerosis in aging men: purported association and clinical implications. Am J Cardiovasc Drugs. 2005 5(3):141-54.
- Traish AM, Haider A, Doros G, Saad F. Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study. Int J Clin Pract. 2014 Mar;68(3):314-29.
- Malkin CJ, Pugh PJ, West JN, van Beek EJ, Jones TH, Channer KS. Testosterone therapy in men with moderate severity heart failure: a double-blind randomized placebo controlled trial. Eur Heart J. 2006 Jan;27(1):57-64.
- Aversa A, Bruzziches R, Francomano D, et al. Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 24-month, randomized, double-blind, placebo-controlled study.J Sex Med . 2010 Oct;7(10):3495-503.
- Toma M, McAlister FA, Coglianese EE, et al. Testosterone supplementation in heart failure: a meta-analysis. Circ Heart Fail. 2012 May 1;5(3):315-21.
- Mathur A, Malkin C, Saeed B, Muthusamy R, Jones TH, Channer K. Long-term benefits of testosterone replacement therapy on angina threshold and atheroma in men. Eur J Endocrinol. 2009 Sep;161(3):443-9.
- Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/scda/causes. Accessed March 27, 2015.
- Oskui PM, French WJ, Herring MJ, Mayeda GS, Burstein S, Kloner RA. Testosterone and the cardiovascular system: a comprehensive review of the clinical literature. J Am Heart Assoc. 2013 Nov 15;2(6):e000272.
- Hu X, Rui L, Zhu T, et al. Low testosterone level in middle-aged male patients with coronary artery disease. Eur J Intern Med. 2011 Dec;22(6):e133-6.
- Available at: https://www.lifeextension.com//magazine/2014/3/response-to-media-reports-associating-testosterone-treatment-with-greater-heart-attack-risk/page-01. Accessed January 27, 2015.
- Available at: https://www.lifeextension.com//magazine/2012/ce/testosterone-controversy/page-01. Accessed January 27, 2015.
- Available at: https://www.lifeextension.com//magazine/2008/6/rebuttal-to-attack-against-bioidentical-hormones/page-01. Accessed January 27, 2015.
- Available at: https://www.lifeextension.com/magazine/2004/2/cover_test/page-01. Accessed January 27, 2015.
- Available at: http://abcnews.go.com/blogs/health/2013/11/05/testosterone-supplements-tied-to-heart-attacks-strokes-early-death. Accessed January 27, 2015.
- Available at: http://www.usatoday.com/story/news/nation/2014/01/29/testosterone-heart-risks/4967795. Accessed January 27, 2015.
- Cappola AR. Testosterone therapy and risk of cardiovascular disease in men. JAMA. 2013 Nov 6;310(17):1805-6. Editorial
- Available at: http://truttmd.com/testosterone-cause-heart-attacks-response-jama. Accessed January 27, 2015.
- Available at: http://open.salon.com/blog/jeffrey_dach_md/2014/06/23/testosterone_found_to_cause_heart_attacks. Accessed January 27, 2015.
- Finkle WD, Greenland S, Ridgeway GK, et al. Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men. PLoS One. 2014 Jan 29;9(1):e85805.
- Vigen R, O’Donnell CI, Barón AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013 Nov 6;310(17):1829-36.
- Harrington RA, Hodgson PK, Larsen RL. Cardiology patient page. Antiplatelet therapy. Circulation. 2003 Aug 19;108(7):e45-7.
- Phillips GB, Pinkernell BH, Jing TY. The association of hyperestrogenemia with coronary thrombosis in men. Arterioscler Thromb Vasc Biol. 1996 Nov;16(11):1383-7.
- Jasuja GK, Travison TG, Davda M, et al. Age trends in estradiol and estrone levels measured using liquid chromatography tandem mass spectrometry in community-dwelling men of the Framingham Heart Study. J Gerontol A Biol Sci Med Sci. 2013 Jun;68(6):733-40.
- Vermeulen A, Kaufman JM, Goemaere S, van Pottelberg I. Estradiol in elderly men. Aging Male. 2002 Jun;5(2):98-102.
- Jankowska EA, Rozentryt P, Ponikowska B, et al. Circulating estradiol and mortality in men with systolic chronic heart failure. JAMA. 2009 May 13;301(18):1892-901.
- Laughlin GA, Barrett-Connor E, Bergstrom J. Low serum testosterone and mortality in older men. J Clin Endocrinol Metab. 2008 Jan;93(1):68-75.
- Shores MM, Matsumoto AM, Sloan KL, Kivlahan DR. Low serum testosterone and mortality in male veterans. Arch Intern Med. 2006 Aug 14-28;166(15):1660-5.
- Khaw KT, Dowsett M, Folkerd E, et al. Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) Prospective Population Study. Circulation. 2007 Dec 4;116(23):2694-701.
- Available at: http://www.fda.gov/safety/medwatch/safetyinformation/safetyalertsforhumanmedicalproducts/ucm436280.htm. Accessed March 10, 2015.
- Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ ReproductiveHealthDrugsAdvisoryCommittee/UCM418144.pdf. Accessed Mar 10, 2015.
- Beggs LA, Yarrow JF, Conover CF, et al. Testosterone alters iron metabolism and stimulates red blood cell production independently of dihydrotestosterone. Am J Physiol Endocrinol Metab. 2014 Sep 1;307(5):E456-61.
- Carrero JJ, Bárány P, Yilmaz MI, et al. Testosterone deficiency is a cause of anaemia and reduced responsiveness to erythropoiesis-stimulating agents in men with chronic kidney disease. Nephrol Dial Transplant. 2012 Feb;27(2):709-15.
- Ferrucci L, Maggio M, Bandinelli S, et al. Low testosterone levels and the risk of anemia in older men and women. Arch Intern Med. 2006 Jul 10;166(13):1380-8.
- Kim SW, Hwang JH, Cheon JM, et al. Direct and indirect effects of androgens on survival of hematopoietic progenitor cells in vitro. J Korean Med Sci. 2005 Jun;20(3):409-16.
- Maganty A, Kovac JR, Ramasamy R.The putative mechanisms underlying testosterone and cardiovascular risk. F1000Res. 2014 Apr 4;3:87.
- Surampudi PN, Wang C, Swerdloff R. Hypogonadism in the aging male diagnosis, potential benefits, and risks of testosterone replacement therapy. Int J Endocrinol. 2012;2012:625434.
- Available at: http://www.porphyriafoundation.com/about-porphyria/types-of-porphyria/epp. Accessed January 28, 2015.
- Osterberg EC, Bernie AM, Ramasamy R. Risks of testosterone replacement therapy in men. Indian J Urol. 2014 Jan;30(1):2-7.
- Brawer MK.Testosterone replacement therapy for a man with prostate cancer. Rev Urol. 2004;6 Suppl 6:S35-7.
- Kaplan AL, Lenis AT, Shah A, Rajfer J, Hu JC. Testosterone replacement therapy in men with prostate cancer: a time-varying analysis. J Sex Med. 2015 Feb;12(2):374-80.
- Cui Y, Zong H, Yan H, Zhang Y. The effect of testosterone replacement therapy on prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2014 Jun;17(2):132-43.
- Morgentaler A, Lipshultz LI, Bennett R, Sweeney M, Avila D Jr, Khera M. Testosterone therapy in men with untreated prostate cancer. J Urol. 2011 Apr;185(4):1256-60.
- Vaucher L, Paduch DA, Jichlinski P, Pralong F. Testosterone and prostate. Rev Med Suisse. 2011 Dec 7;7(320):2399-400, 2402-3.
- Marks LS, Mazer NA, Mostaghel E, et al. Effect of testosterone replacement therapy on prostate tissue in men with late-onset hypogonadism: a randomized controlled trial. JAMA. 2006 Nov 15;296(19):2351-61.
- Agarwal PK, Oefelein MG. Testosterone replacement therapy after primary treatment for prostate cancer. J Urol. 2005 Feb;173(2):533-6.
- Rhoden EL, Morgentaler A. Testosterone replacement therapy in hypogonadal men at high risk for prostate cancer: results of 1 year of treatment in men with prostatic intraepithelial neoplasia. J Urol. 2003 Dec;170(6 Pt 1):2348-51.
- Bhasin S, Singh AB, Mac RP, Carter B, Lee MI, Cunningham GR. Managing the risks of prostate disease during testosterone replacement therapy in older men: recommendations for a standardized monitoring plan. J Androl. 2003 May-Jun;24(3):299-311. Review.
- Hoffman MA, DeWolf WC, Morgentaler A. Is low serum free testosterone a marker for high grade prostate cancer? J Urol. 2000 Mar;163(3):824-7.
- Eaton NE, Reeves GK, Appleby PN, Key TJ. Endogenous sex hormones and prostate cancer: a quantitative review of prospective studies. Br J Cancer. 1999 Jun;80(7):930-4.
- Mohamad MJ, Mohammad MA, Karayyem M, Hairi A, Hader AA. Serum levels of sex hormones in men with acute myocardial infarction. Neuro Endocrinol Lett. 2007 Apr;28(2):182-6.
- Abbott RD, Launer LJ, Rodriguez BL, et al. Serum estradiol and risk of stroke in elderly men. Neurology. 2007 Feb 20;68(8):563-8.
- Kalinchenko SY, Tishova YA, Mskhalaya GJ, Gooren LJ, Giltay EJ, Saad F. Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: the double-blinded placebo-controlled Moscow study. Clin Endocrinol (Oxf). 2010 Nov;73(5):602-12.
- Kapoor D, Goodwin E, Channer KS, Jones TH. Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol. 2006 Jun;154(6):899-906.
- Rebuffe-Scrive M, Marin P, Bjorntorp P. Effect of testosterone on abdominal adipose tissue in men. Int J Obes. 1991 Nov;15(11):791-5.
- Lee HK, Lee JK, Cho B. The role of androgen in the adipose tissue of males. World J Mens Health. 2013 Aug;31(2):136-40.
- Araujo AB, Dixon JM, Suarez EA, Murad MH, Guey LT, Wittert GA. Clinical review: Endogenous testosterone and mortality in men: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011 Oct;96(10):3007-19.
- Lerchbaum E, Pilz S, Grammer TB, Boehm BO, März W, Obermayer-Pietsch B. High estradiol levels are associated with increased mortality in older men referred to coronary angiography. Exp Clin Endocrinol Diabetes. 2011 Sep;119(8):490-6.
- Haring R, Völzke H, Steveling A, et al. Low serum testosterone levels are associated with increased risk of mortality in a population-based cohort of men aged 20-79. Eur Heart J. 2010 Jun;31(12):1494-501.
- Tivesten A, Vandenput L, Labrie F, et al. Low serum testosterone and estradiol predict mortality in elderly men. J Clin Endocrinol Metab. 2009 Jul;94(7):2482-8.
- Available at: https://www.lifeextension.com//magazine/2014/3/response-to-media-reports-associating-testosterone-treatment-with-greater-heart-attack-risk/page-01. Accessed March 10, 2015.
- Available at: https://www.lifeextension.com/magazine/2014/6/misguided-medicine/page-01. Accessed March 10, 2015.

