Life Extension Magazine®

More than 2,000 Americans suffer a stroke on an average day.1 Some will recover with minor outward effects, while others who survive endure paralysis and lifelong nursing home confinement.
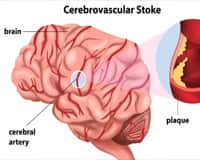
Most strokes happen when a blood clot blocks an artery that feeds a portion of the brain.2 As neurons die from oxygen starvation, the result too often is paralysis, blindness, and cognitive dysfunction.3
Stroke is a leading cause of long-term disability in the United States. It’s also the fifth-leading cause of death.4,5
The tragedy is that many strokes can be reversed if competent arterial intervention is timely delivered.6
Emergency response personnel are dropping the ball when it comes to implementing common-sense procedures to remove blood clots before permanent brain damage occurs.
This article reveals how hundreds of thousands of stroke-induced catastrophes can be prevented each year and what you should do if a stroke symptom ever manifests.

Horrific consequences occur when scientific advances are delayed from entering everyday medical practice.
The term “ischemia” means insufficient blood flow to a body part. This article addresses acute ischemia to the brain, which is commonly referred to as a stroke.7
In the treatment of acute ischemic stroke, significant advances are being made in the re-opening of blocked cerebral arteries. These lifesaving procedures enable blood flow to be restored before permanent brain damage is inflicted.8,9
The problem is that not enough emergency response personnel are trained to properly utilize these brain-saving techniques. The result is nursing homes that are filled with permanently paralyzed stroke victims whose conditions were reversible after they entered the hospital emergency room—if only appropriate procedures were administered.
The economic cost of not prioritizing implementation of even basic cerebral recanalization (re-opening) techniques is staggering. The human toll of needless paralysis, dementia, and death is beyond civil description in the English nomenclature.
Despite a preponderance of favorable data, there is still debate amongst clinicians as to when to employ advanced techniques in attempting to reverse acute ischemic stroke.
Stroke Treatment Breakthroughs
 |
As I was writing this article, new findings were released documenting how many stroke victims could be saved if intra-arterial recanalization procedures were more widely used. Here are the highlights from these clinical trials:
- In patients receiving intra-arterial thrombectomy/tPA within 4.5 hours of stroke symptom manifestation, a median of 100% showed brain reperfusion at 24 hours compared to 37% receiving standard intravenous tPA. The clinical result measured in functional independence was 71% in the thrombectomy/tPA group versus 40% in the standard tPA group.25
- Another clinical study showed that as late as 12 hours after stroke symptoms appeared, a significant improvement in functional outcome was observed in the thrombectomy/tPA group compared to the standard-of-care group (usually tPA alone). This trial also showed that mortality (death) in the thrombectomy/tPA group after 90 days was cut almost in half (10.4% versus 19.0%, p=0.04).24
- In a third study released in early 2015, 60.2% of stroke victims showed a good functional outcome in the thrombectomy/tPA group compared to 35.5% receiving intravenous tPA alone. (Note that poor “functional outcomes” often mean lifelong disability and loss of independence.)26
These remarkable findings, which help corroborate a large 2014 clinical study, provide a clear validation to treat ischemic stroke patients as late as 12 hours after symptoms manifest with intra-arterial tPA/clot-retriever procedures.21
I encourage every member to call their local hospitals now to identify which are “comprehensive stroke centers” with trained medical staff on the use of intra-arterial tPA/advanced stent/clot-retriever procedures. Every minute of delay reduces one’s odds of reversing an acute ischemic stroke. The article on page 88 of this issue provides a listing of comprehensive stroke centers that Life Extension has identified in the United States.
How Larry King Saved Millions Of Lives

Talk show host Larry King is a nonstop workaholic. For most of his life, he smoked three packs of cigarettes a day, ate anything and everything fried, and piled on the desserts. All of this was combined with no exercise and a high level of job-related stress.
In February 1987, as pain ripped through his shoulder and stomach, Larry King headed to the hospital emergency room. It was clear to the staff at George Washington University Hospital that Larry was in the midst of a severe heart attack.10
In order to save his life, the doctors decided to try the then-experimental clot-busting drug called tPA (tissue plasminogen activator).
In early 1987, tPA had not yet been approved by the FDA.11 Before administering tPA to open Larry’s blocked coronary arteries, the doctors placed a clipboard with a release form in front of Larry so he could sign away any liability. Fortunately, he was at one of the few hospitals at the time who were “allowed” to provide this clot-dissolving drug to consenting patients.
Larry King was so impressed by how quickly his crushing pain was alleviated by tPA that he spearheaded a campaign attacking the FDA for not approving widespread use of this drug. The FDA was delaying approval of tPA because the agency wanted proof that tPA benefited heart attack victims in addition to acutely saving lives.12
Back in the mid-1980s, The Wall Street Journal and Life Extension Foundation were challenging the FDA’s delay of tPA. The agency’s reason for not approving tPA is that they did not know if it would prolong the life span of acute heart attack patients who otherwise had only minutes to live.
Larry King tilted the public against the FDA and the merciful result was that tPA gained official approval to treat acute heart attack in November 1987—nine months after it saved Larry King’s life.13
Two years later, the FDA conceded that tPA indeed improved survival in heart attack victims, which had been the agency’s basis for delaying initial approval of the drug.14 It was not until 1996 that tPA was approved to treat acute ischemic stroke.11
Here we are in year 2015, and controversy continues regarding the best protocols to treat acute stroke with clot-dissolving drugs like tPA and/or mechanical recanalization techniques like cerebral artery stenting.
What I find remarkable, however, was the impact that one celebrity activist such as Larry King had in breaking down bureaucratic barriers that had cost so many human lives.
Taking Initiatives To Reduce Stroke Risk
 |
Circulatory deficits are a leading cause of disability and mortality in aging humans.38,39
Conventional medicine views disorders related to blood flow impairment (stroke, heart attack, kidney failure) as inevitable consequences of aging.40
Yet a search on the National Library of Medicine data base entering the term “endothelial dysfunction” reveals over 64,000 published articles. Many of these peer-reviewed scientific findings describe how to prevent or reverse vascular disorders by making healthy lifestyle choices that most Life Extension® members have followed for many decades.41
Why Stroke Treatment Is Challenging
Acute myocardial infarction (heart attack) is relatively easy to diagnose. The heart muscle can also withstand oxygen deprivation far longer than the brain, where neurons die within minutes of blood flow cessation.7 These and other factors make using clot-dissolving drugs like tPA in heart attack patients easier than in those stricken by stroke.
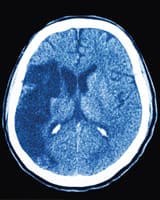
A stroke can be either ischemic (blockage) or hemorrhagic (bleeding). A CT scan or MRI of the brain must be done quickly at a hospital’s emergency department to diagnose what kind of stroke is occurring (about 85% of strokes are ischemic).15,16
Based on brain imaging results, a quick decision must be made whether to implement a clot dissolving drug and/or utilize intracerebral arterial stenting to reverse the blockage causing an ischemic stroke.
The FDA and most medical authorities claim that clot-dissolving therapy must be initiated within 3.0 to 4.5 hours from initial onset of symptoms for the benefits to outweigh the side-effect risks (such as cerebral bleeding).17 New studies indicate that advanced clot-removing therapies are efficacious for a longer period after initial stroke symptoms present.18
For example, technologies have now progressed to a level where a catheter can be inserted into a major artery and threaded directly into the brain’s vasculature. This enables the mechanical removal of a blood clot blocking an artery. The procedure is called a thrombectomy.19
Thrombectomy techniques have advanced to the point where a trained physician utilizing a retrievable stent can re-open a blocked cerebral artery mechanically when a clot-dissolving therapy using a tPA drug is not working.20
The challenge in treating ischemic stroke is that there are many factors that dictate the risk-to-reward ratio of tPA administration
and/or thrombectomy for individual stroke patients. This has caused clot-removing therapies to be
under-
utilized
by emergency physicians, with the tragic result being needless paralysis and death.
The Grim Statistics
 |
Stroke is the fifth-leading cause of death in the US, and also is a major cause of disability and loss of independence and quality of life.4,5
Up to 40% of strokes can be fatal. Prompt treatment can significantly reduce the risk of disability and death.42
Here are some statistics:33
- Approximately 795,000 people suffer a stroke each year. Most, about 600,000 of these, are first attacks, while 185,000 are recurrent attacks.
- Stroke risk more than doubles each decade after age 55. Almost three-fourths of all stroke victims are over age 65.
- However, strokes can and do occur at any age. Almost a quarter of all strokes occur in those under the age of 65.
- African-Americans have a higher stroke death rate than whites, even at a younger age.
- Every 40 seconds on average, someone in the United States suffers a stroke.
- In 2005, stroke mortality was 137,000.
- Current smokers have almost double the risk of nonsmokers of ischemic stroke after adjustment for other risk factors.
- Atrial fibrillation (AF) is an independent risk factor for stroke, increasing risk about 5-fold.
- The top risk factor for stroke is high blood pressure.
Paralysis or the inability of a muscle to move is one of the most common disabilities resulting from stroke. Among people who survive a stroke, as many as nine out of 10 have some degree of paralysis immediately afterwards.44
While mainstream medicine has identified many of the risk factors for stroke, they too often omit other documented risk factors of stroke such as elevated blood levels of homocysteine,35,36,44,45 C-reactive protein,46-49 fibrinogen,49-53 LDL,54-57 and hormone imbalances.58-60
Annual blood testing, along with regular monitoring of blood pressure, are critical elements of a stroke prevention program.
Narrow Window Of Therapeutic Opportunity
Brain cells quickly become impaired and die when oxygen-rich blood flow is interrupted. Even a 15-minute delay in initiating clot-removing therapy reduces the chances that a patient will avoid a stroke-induced disability.21
A consensus today is that in most cases, clot-removing therapy in ischemic stroke patients should commence within one hour of arrival in a hospital’s emergency room.22
With properly trained staff, initiation of tPA within one hour is feasible, yet a 2009 study found that “door-to-needle” for tPA treatment within one hour was occurring in only 29% of cases. This was an improvement compared to 19% in year 2003.23
As you might expect, hospitals treating patients in greater volume are better at meeting the one-hour treatment initiation objective with tPA compared to hospitals treating fewer stroke patients. Patients also have a higher probability of receiving timely tPA treatment if they are younger, male, of white race, had no prior stroke, or if they arrive by ambulance.23
When stroke symptoms initially develop, the patient or a family member is sometimes able to drive to a hospital emergency room. The downside to this is less priority given by the ER staff and the risk that tPA therapy will be delayed.
To clarify this critical point, the therapeutic window of opportunity with tPA drug therapy and/or surgical stenting is time sensitive. The initial protocol was that tPA had to be initiated within three hours of the onset of the first stroke symptom. This was later expanded to 4.5 hours after onset of first indication of ischemic stroke. More recent studies suggest that more advanced clot-removing therapies may be used up to 12 hours after first onset of stroke symptoms.24
The reason it is so critical for emergency physicians to initiate clot-removing therapy within one hour is that there is often a significant delay between the patient realizing they are having a stroke and making it into the hospital.
The sidebar on page 12 lists the most common symptoms of stroke. If any of these symptoms develop in you, don’t hesitate to call an ambulance to be transported to a hospital for immediate evaluation. It could mean the difference in you quickly returning to a normal life or permanent confinement to a nursing home or cemetery.
I suspect most Life Extension® members detest going to a hospital, but when it comes to symptoms of a stroke (or heart attack), any delay can mean permanent institutional confinement.
Stroke Signs And Symptoms
 |
By knowing the signs and symptoms of stroke, you can be prepared to take quick action and perhaps save a life—maybe even your own.60,61
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body.
- Sudden confusion, trouble speaking, or difficulty understanding speech.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
- Sudden severe headache with no known cause.
Call 911 immediately if you or someone else has any of these symptoms.
(This list is repeated on page 15 so it can be cut out and pasted in your home or office.)
Why Clot-Removing Therapies Are Underutilized
Despite stroke being the fifth-leading cause of death and a leading cause of disability in the United States, less than 7% of stroke survivors (as of year 2010) receive tissue plasminogen activator (tPA) as initial treatment.27
A review of two studies, one that examined 45 published articles and one that examined 54 published articles, revealed common barriers to greater tPA use in both pre-hospital and in-hospital settings.29,30
Pre-hospital delays were related to trying to contact primary care physicians instead of immediately rushing to the emergency room, the mode of arrival to the hospital, and patient’s lack of knowledge regarding stroke symptoms.29,30
The causes of in-hospital delays included non-stroke center status, lack of training of emergency department, delays in CT (computed tomography) scans, and poor understanding regarding priority of stroke treatment.29,30
The major issues behind the underutilization of tPA for acute stroke is lack of hospital readiness/preparation, inadequate staff training, and failure to rapidly administer tPA. Patients’ lack of awareness of stroke symptoms is another critical factor that precludes more stroke victims from benefiting from clot-removal therapies.
As a result of these and other factors, some clinicians question the efficacy of tPA and other brain clot-removing procedures. Interpreting sometimes flawed and contradictory clinical studies contributes to confusion and delay in administering tPA in the emergency room setting.
A 2011 study found only 1 to 3% of ischemic stroke patients in community settings receive clot-dissolving therapy.31 While some of these stroke victims were ineligible, others were tPA candidates that were denied for reasons that should not be permitted to continue.
Acting F.A.S.T. Is Key For Stroke
 |
Acting F.A.S.T. can help stroke patients get the treatment they desperately need. The most effective stroke treatments are only available if the stroke is recognized and diagnosed within three hours of the first symptoms. Stroke patients may not be eligible for the most effective treatments if they don’t arrive at the hospital in time.
If you think someone may be having a stroke, act F.A.S.T. and do the following simple test:
- F—Face: Ask the person to smile. Does one side of the face droop?
- A—Arms: Ask the person to raise both arms. Does one arm drift downward?
- S—Speech: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- T—Time: If you observe any of these signs, call 911 immediately.
Note the time when any symptoms first appear. Some treatments for stroke only work if given in the first three to six hours after symptoms appear. Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin lifesaving treatment on the way to the emergency room.
Treating A Transient Ischemic Attack (TIA)
If your symptoms go away after a few minutes,62 you may have had a transient ischemic attack (TIA).63 Although brief, a TIA is indicative of a serious condition that will not go away without medical intervention.61,64,65 Tell your health care team about your symptoms right away.
Unfortunately, because TIAs clear up, many people ignore them.66 Don’t be one of those people. Paying attention to a TIA can save your life by enabling implementation of therapies to restore cerebral circulation before a major stroke develops.65
A Growing Consensus In Favor Of tPA
A study published in 2012 on the use of tPA in the treatment of acute stroke found that:32
“tPA is an effective treatment for stroke when given in prepared stroke centers; emergency physicians and hospitals treating stroke patients with tPA need to have the necessary resources in place and a specific plan for timely care of patients with acute stroke.”
This study found a significant reduction in stroke-induced disability was achieved despite inclusion of patients treated with tPA after 4.5 hours. It also found that the improper use of tPA (such as administering it to patients with hemorrhagic stroke) skewed results in a way that could be interpreted as finding no overall benefit to tPA.31
The study concluded that tPA has demonstrated benefit in “academic centers and organized stroke centers, but the benefit is not established at other types of hospitals.”32
This study clears up a lot of misconceptions and criticisms about the use of tPA in the treatment of acute ischemic stroke. As simple as this may sound, more community hospitals need to upgrade their skill levels to those found in organized stroke centers.
Each year, 795,000 strokes occur in the United States.33 Stroke is not a rare event, yet hospital emergency departments that have skill in treating heart attacks are failing miserably when it comes to reversing acute ischemic stroke, despite there being similarities in the treatment protocols.
Increasing Recognition Of Endovascular Therapy For Stroke
The June 11, 2015, issue of The New England Journal of Medicine published two more studies on the benefits of endovascular treatment for acute stroke:
- During a two-year period, 206 people were randomized to either a standard medical therapy arm (which may include alteplase, a type of recombinant tPA) or medical therapy plus endovascular therapy using the Solitaire stent retriever (thrombectomy). The endovascular group had a 70% reduction in the severity of disability for a predefined disability scale. After 90 days, 43.7% of the endovascular group was able to achieve a predefined level of functional independence as opposed to only 28.2% in the standard medical therapy group. This study intended to enroll more patients (sample size, 690), but favorable results in other clinical studies of endovascular therapy prompted the researchers to end the trial early on the basis of medical ethics (i.e., the evidence of superior efficacy of endovascular therapy from other trials).
- In a study at 39 participating sites, 196 patients were randomized (98 patients in each of two groups) to either tPA alone or tPA plus endovascular therapy within six hours of stroke symptoms manifesting. The rate of substantial reperfusion to the brain in the group receiving tPA plus endovascular therapy was 88%. The rate of functional independence was 60% in the tPA plus endovascular therapy group compared to 35% in the group that only received tPA. The results were so obvious the study was stopped early.1-3
Progressive vascular surgeons have utilized endovascular therapy to treat ischemic stroke since 1999. The title of an editorial in the June 11, 2015, issue of The New England Journal of Medicine was:
“Endovascular Therapy for Stroke — It’s About Time.”
I have two comments about this.
First, it should not have taken 15 years to transform endovascular therapy into “standard” practice when attempting to reverse acute stroke. Over the past 15 years, more than ten million Americans have been stricken with stroke. Millions have died or lie paralyzed in nursing home facilities. Earlier implementation of endovascular therapy could have enabled many stroke victims to regain functional independence.
Second is that even with the best endovascular therapies, too many stroke victims are left with some form of paralysis (or death). Yet the vast majority of strokes are preventable. Articles in this month’s issue of Life Extension magazine provides practical guidance on how to slash your risk of ever developing an acute ischemic stroke. Since these methods have the side benefit of slashing all kinds of disorders such as heart attack, there is no reason to leave yourself vulnerable to the vascular risks posed by endothelial dysfunction and hypertension.
References
- N Eng J Med. 2015 Jun 11;372;2347.
- N Eng J Med. 2015 Jun 11;372:2296-306.
- N Eng J Med. 2015 Jun 11;372:2285-95.
A New Year’s Gift
I was pleased to read the January 1, 2015, edition of The New England Journal of Medicine, where the results from a large study on acute stroke were published.34
This study sought to evaluate whether standard intravenous tPA therapy in addition to aggressive use of targeted intra-arterial delivery of tPA and/or advanced intra-arterial surgical procedures was superior to standard intravenous tPA therapy alone in treating a particularly dangerous type of ischemic stroke within six hours of symptom onset.
The effectiveness of intra-venous tPA is limited by several factors compared to what can be achieved by threading a catheter into the blocked cerebral artery and directly administering tPA to the blood clot causing the ischemic stroke. This intra-arterial catheter can further be used to surgically remove the occluding blood clot or install a retrievable stent to prop open the occluded cerebral artery.34
In this study published on New Year’s Day of this year, patients fortunate enough to be treated with aggressive clot-removing techniques were twice as likely to recover independent living capability without major functional restriction compared to the group receiving standard medical therapies.34
What made this study stand out was that it demonstrated convincing efficacy compared to previous studies that produced only neutral results. Some of the differences were that this latest study included an improved intra-arterial “retrievable stenting” device, proper imaging to identify precise location of the occluded artery, and shorter time interval to treatment (under six hours) compared to previous studies.34,37
Not all findings from this study published on New Year’s Day of this year were positive. Patients requiring mechanical removal of their occluded cerebral artery suffered greater numbers of secondary ischemic events within 90 days, probably due to the physical/mechanical nature of the intervention. Yet in the aggressively treated group there was no significant increase in mortality and no significant increase in serious side effects compared to the control group during the follow-up period.34 The aggressively treated groups showed a consistent trend of benefit that led to a far greater rate of functional recovery.
Said differently, aggressive treatment of this dangerous type of ischemic stroke (proximal arterial occlusion) resulted in significantly more patients avoiding nursing home confinement.
An editorial in this same issue of The New England Journal of Medicine (Jan 1, 2015) posed the question:37
“Is there any doubt left, or should thrombectomy now become the new standard treatment for severe stroke with proximal large-vessel occlusion up to six hours after stroke onset?”
The editor answered his own question by stating he eagerly awaits the results of ongoing trials, but that this latest clinical trial titled MR CLEAN “is the first step in the right direction.”
Stroke Signs And Symptoms
 |
By knowing the signs and symptoms of stroke, you can be prepared to take quick action and perhaps save a life—maybe even your own.60,61
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body.
- Sudden confusion, trouble speaking, or difficulty understanding speech.
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance, or lack of coordination.
- Sudden severe headache with no known cause.
Call 911 immediately if you or someone else has any of these symptoms.
Turning The Tide
A large volume of published clinical data persuasively demonstrates that far more stroke victims could be leaving the hospital and returning to their homes to resume normal independent activities.
Technologies exist today to reverse huge numbers of ischemic strokes. Yet not enough hospital emergency rooms qualify as competent “stroke centers,” with trained personnel and state-of-the-art protocols.
It probably is not necessary for every hospital emergency room to have advanced “stroke center” capabilities, as there are often several hospitals within reasonable reach for ambulances from places where most people live.
Despite the staggering costs of caring for paralyzed stroke victims, priorities aimed at creating competent “stroke centers” within ambulance range of major population centers is sorely lacking. Life Extension is helping to address this problem by compiling a nationwide listing of comprehensive stroke centers. This listing can be reviewed starting on page 88 of this month’s issue.
Those concerned whether their hospital emergency department is utilizing state-of-the-art stroke treatments should consider making an appointment with the hospital administrator in their neighborhood to encourage them to upgrade to “comprehensive stroke center” status, which includes quick turnaround CT or MRI imaging and timely initiation of intra-arterial tPA and intra-arterial (endovascular) clot removing retrievable stent devices.
If your local hospital refuses, shop around and you may find that a qualified “stroke center” exists not that far away. This will enable you to know where to go in case stroke symptoms ever manifest.
On page 88 of this month’s issue is a listing of comprehensive stroke centers in the United States that Life Extension’s staff has been able to identify so far.
For longer life,
William Faloon
To view a video presentation of how intra-arterial clot removal catheter technology can reverse ischemic stroke, log on to:
LifeExtension.com/strokevideo
References
- Available at: http://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_305054.pdf. Accessed March 3, 2015.
- Available at: http://www.cdc.gov/stroketypes_of_stroke.htm. Accessed March 3, 2015.
- Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/stroke/signs. Accessed March 3, 2015.
- Kochanek KD, Xu JQ, Murphy SL, Arias E. Mortality in the United States, 2013. NCHS Data Brief, No. 178. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, US Dept. of Health and Human Services; 2014.
- Available at: http://www.cdc.gov/stroke. Accessed March 3, 2015.
- Available at: http://www.sciencedaily.com/releases/2008/08/080825132115.htm. Accessed March 3, 2015.
- Lee JM, Grabb MC, Zipfel GJ, Choi DW. Brain tissue responses to ischemia. J Clin Invest. 2000 Sep;106(6):723-31.
- Lin MP, Sanossian N. Reperfusion therapy in the acute management of ischemic stroke. Cardiol Clin. 2015 Feb;33(1): 99-109.
- Hasegawa H, Inoue T, Tamura A, Saito I. Emergent intracranial surgical embolectomy in conjunction with carotid endarterectomy for acute internal carotid artery terminus embolic occlusion and tandem occlusion of the cervical carotid artery due to plaque rupture. J Neurosurg. 2015 Jan 9:1-9.
- Available at: http://www.cnn.com/2010/showbiz/tv/02/11/larry.king.stents. Accessed March 3, 2015.
- Zivin JA. Acute stroke therapy with tissue plasminogen activator (tPA) since it was approved by the U.S. Food and Drug Administration (FDA). Ann Neurol. 2009 Jul;66(1):6-10.
- Available at: https://www.lifeextension.com/magazine/2008/2/cover_larry_king/page-01. Accessed March 3, 2015.
- Available at: http://articles.chicagotribune.com/1987-11-13/news/8703250718_1_dr-eugene-braunwald-tpa-blood-clots. Accessed March 3, 2015.
- Available at: http://www.gene.com/media/press-releases/4277/1989-02-27/fda-approves-reduced-mortality-claim-for. Accessed March 3, 2015.
- Available at: http://www.strokeassociation.org/strokeorg/aboutstroke/typesofstroke/types-of-stroke_ucm_308531_subhomepage.jsp. Accessed March 3, 2015.
- Available at: http://www.cdc.gov/stroketypes_of_stroke.htm. Accessed March 3, 2015.
- Lansberg MG, Bluhmki E, Thijs VN. Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a meta analysis. Stroke. 2009 Jul;40(7):2438-41.
- Asadi H, Yan B, Dowling R, Wong S, Mitchell P. Advances in medical revascularization treatments in acute ischemic stroke. Thrombosis. 2014 2014:714218.
- Htyte N, Parto P, Ragbir S, Jaffe L, White CJ. Predictors of outcomes following catheter-based therapy for acute stroke. Catheter Cardiovasc Interv. 2014 Nov 20.
- Smith WS. Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I. AJNR Am J Neuroradiol. 2006 Jun-Jul;27(6):1177-82.
- Meretoja A, Keshtkaran M, Saver JL, et al. Stroke thrombolysis: save a minute, save a day. Stroke. 2014 Apr;45(4):1053-8.
- Greenberg K, Maxwell CR, Moore KD, et al. Improved door-to-needle times and neurologic outcomes when IV tissue plasminogen activator is administered by emergency physicians with advanced neuroscience training. Am J Emerg Med. 2015 Feb;33(2):234-7.
- Fonarow GC, Smith EE, Saver JL, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation 2011 Feb 22;123(7):750-8.
- Goyal M, Demchuk AM, Menon BK, et al. ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015 Mar 12;372(11):1019-30.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015 Mar 12;372(11):1009-18.
- Saver JL, Goyal M, Bonafe A, et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N Engl J Med 2015 Apr 17. [Epub ahead of print].
- Cocho D, Belvis R, Marti-Fabregas J, et al. Reasons for exclusion from thrombolytic therapy following acute ischemic stroke. Neurology. 2005:64(4):719-20.
- Johnson M, Bakas T. A review of barriers to thrombolytic therapy: implications for nursing care in the emergency department. J Neurosci Nurs. 2010 Apr;42(2): 88-94.
- Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004 Mar;33(2):116-21.
- Meurer WJ, Majersik JJ, Frederiksen SM, Kade AM, Sandretto AM, Scott PA. Provider perceptions of barriers to the emergency use of tPA for acute ischemic stroke: a qualitative study. BMC Emerg Med. 2011 May 6;11:5.
- DeMers G, Meurer WJ, Shih R, Rosenbaum S, Vilke GM. Tissue plasminogen activator and stroke: review of the literature for the clinician. J Emerg Med. 2012 Dec;43(6):1149-54.
- Available at: http://www.strokecenter.org/patients/about-stroke/stroke-statistics. Accessed March 12, 2015.
- Berkhemer OA, Fransen PS, Beumer D, et al. MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015 Jan 1;372(1):11-20.
- Vancheri F, Curcio M, Burgio A, et al. Impaired glucose metabolism in patients with acute stroke and no previous diagnosis of diabetes mellitus. QJM. 2005 Dec;98(12):871-8.
- Sacco RL, Anand K, Lee HS, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the NOrthern MAnhattan Study. Stroke. 2004 Oct;35(10):2263-9.
- Hacke W. Interventional thrombectomy for major stroke--a step in the right direction. N Engl J Med. 2015 Jan 1;372(1):76-7.
- Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_04.pdf. Accessed March 16, 2015.
- Available at: http://www.cdc.gov/strokefacts.htm. Accessed March 20, 2015.
- Michael KM, Shaughnessy M. Stroke prevention and management in older adults. J Cardiovasc Nurs. 2006 Sep-Oct;21(5 Suppl 1):S21-6.
- Vilahur G, Padró T, Casaní L, et al. Polyphenol-enriched diet prevents coronary endothelial dysfunction by activating the Akt/eNOS pathway. Rev Esp Cardiol (Engl Ed). 2015 Mar;68(3):216-25.
- Available at: http://www.medicinenet.com/stroke_symptoms/views.htm. Accessed March 16, 2015.
- Available at: http://www.stroke.org/we-can-help/survivors/stroke-recovery/post-stroke-conditions/physical/paralysis. Accessed March 17, 2015.
- Narang AP, Verma I, Kaur S, Narang A, Gupta S, Avasthi G. Homocysteine—risk factor for ischemic stroke? Indian J Physiol Pharmacol. 2009 Jan-Mar;53(1):34-8.
- Wald NJ, Watt HC, Law MR, et al. Homocysteine and ischemic heart disease: results of a prospective study with implications regarding prevention. Arch Intern Med. 1998 Apr 27;158(8):862-7.
- Rost NS, Wolf PA, Kase CS, et al. Plasma concentration of C-reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham study. Stroke. 2001 Nov;32(11):2575-9.
- Di Napoli M, Papa F, Bocola V. C-reactive protein in ischemic stroke: an independent prognostic factor. Stroke. 2001 Apr;32(4):917-24.
- Den Hertog HM, van Rossum JA, van der Worp HB, et al. C-reactive protein in the very early phase of acute ischemic stroke: association with poor outcome and death. J Neurol. 2009 Dec;256(12):2003-8.
- Iyigün I, Bakirci Y. Plasma concentrations of C-reactive protein and fibrinogen in ischaemic stroke. J Int Med Res. 2002 Nov-Dec;30(6):591-6.
- Chuang SY, Bai CH, Chen WH, Lien LM, Pan WH. Fibrinogen independently predicts the development of ischemic stroke in a Taiwanese population: CVDFACTS study. Stroke. 2009 May;40(5):1578-84.
- Bots ML, Elwood PC, Salonen JT, et al. Level of fibrinogen and risk of fatal and non-fatal stroke. EUROSTROKE: a collaborative study among research centres in Europe. J Epidemiol Community Health. 2002 Feb;56 Suppl 1i14-8.
- Kofoed SC, Wittrup HH, Sillesen H, Nordestgaard BG. Fibrinogen predicts ischaemic stroke and advanced atherosclerosis but not echolucent, rupture-prone carotid plaques: the Copenhagen City Heart Study. Eur Heart J. 2003 Mar;24(6):567-76.
- Tracy RP, Arnold AM, Ettinger W, et al. The relationship of fibrinogen and factors VII and VIII to incident cardiovascular disease and death in the elderly: results from the cardiovasculr health study. Arterioscler Thromb Vasc Biol 1999 Jul;19(7):1776-83.
- Zeljkovic A, Vekic J, Spasojevic-Kalimanovska V, et al. LDL and HDL subclasses in acute ischemic stroke: prediction of risk and short-term mortality. Atherosclerosis. 2010 Jun;210(2):548-54.
- Tziomalos K, Athyros VG, Karagiannis A, Mikhailidis DP. Dyslipidemia as a risk factor for ischemic stroke. Curr Top Med Chem. 2009;9(14):1291-7.
- Amarenco P, Goldstein LB, Szarek M, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2007 Dec;38(12):3198-204.
- Amarenco P and Labreuche J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. Lancet Neurol 2009 May;8(5):453-63.
- Abbott RD, Launer LJ, Rodriguez BL, et al. Serum estradiol and risk of stroke in elderly men. Neurology. 2007 Feb 20;68(8):563-8.
- Jeppesen LL, Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS, Winther K. Decreased serum testosterone in men with acute ischemic stroke. Arterioscler Thromb Vasc Biol. 1996 Jun;16(6):749-54.
- Yeap BB, Hyde Z, Almeida OP, et al. Lower testosterone levels predict incident stroke and transient ischemic attack in older men. J Clin Endocrinol Metab 2009 Jul;94(7):2353-9
- Available at: http://www.cdc.gov/strokesigns_symptoms.htm. Accessed March 16, 2015.
- Available at: http://www.ncbi.nlm.nih.gov/pubmedhealth/pmht0024236. Accessed March 14, 2015.
- Available at: http://www.cdc.gov/stroketypes_of_stroke.htm. Accessed March 15, 2015.
- Byrne A, Daly C, Rocke L, Gray J. Can risk stratification of transient ischaemic attacks improve patient care in the emergency department? EMJ. 2007;24(9):637-40.
- Sorensen AG, Ay H. Transient ischemic attack: definition, diagnosis, and risk stratification. Neuroimaging Clin N Am. 2011 May;21(2):303-13.
- McSharry J, Baxter A, Wallace LM, Kenton A, Turner A, French DP. Delay in seeking medical help following transient ischemic attack (TIA) or “mini-stroke”: A qualitative study. PLoS ONE. 2014;9(8):e104434.
- Croot EJ, Ryan TW, Read J, Campbell F, O’Cathain A, Venables G. Transient ischaemic attack: a qualitative study of the long term consequences for patients. BMC. 2014;15:174.

