Life Extension Magazine®
Most people think liver disease is caused by excess alcohol or hepatitis viruses.
The reality is that the leading cause of liver disease today is excess weight.1-4
This form of liver degeneration associated with obesity and high blood sugar is called nonalcoholic fatty liver disease (NAFLD).1,5
With epidemic levels of obese and diabetic Americans, doctors are encountering never before seen record numbers of liver disease.
One startling statistic is that 48% of obese teen boys are estimated to have NAFLD.6 Nonalcoholic fatty liver disease is now the most common cause of chronic liver disease in children and adolescents in the United States due to obesity, insulin resistance, and metabolic syndrome.7 That means that these young lives might be shortened and compromised due to liver disease that will haunt them for the rest of their lives.
With no approved pharmacological treatments, lifestyle and dietary therapies remain the only hope for stemming the tide of NAFLD in children, adolescents, and adults.7, 8
Fortunately, compounds like silymarin found in the milk thistle plant have undergone extensive research for their ability to support liver health. A growing list of studies shows the ability of silymarin to protect against damage inflicted by nonalcoholic fatty liver disease (NAFLD).
Silymarin has even been found to have the potential to reverse the dangerous progression of NAFLD that leads directly to liver fibrosis that destroys most of the liver’s natural functions.
Milk Thistle Extract Prevents And Reverses Liver Disease
Nonalcoholic fatty liver disease (NAFLD) is caused by the excess accumulation of fat in the liver.
It currently affects a staggering one in three Americans and can lead to liver fibrosis, cirrhosis, and liver failure, while sharply raising the risk of liver cancer.1,9-11
Due to the increasing prevalence and severity of fatty liver disease, its treatment should be an urgent priority in modern American healthcare. Yet surprisingly little attention is being given to the prevention of liver disease. Unfortunately, there are no good treatments for liver disease once it has become established. Physicians rarely focus on liver health except in advanced cases.
Liver disease is a major cause of disability and death worldwide, yet it often remains underdiagnosed and underinvestigated.12 Similar to other degenerative diseases, much of the damage and destruction that contributes to liver disease is related to inflammatory and oxidative changes in the liver.13-15
That is precisely what makes silymarin such a potent agent for liver protection. Silymarin has a broad spectrum of anti-inflammatory,16,17 anticancer, and specific liver-protective effects that have been shown to guard against the broad spectrum of threats to the liver and other tissues.18-22
Laboratory studies have uncovered numerous ways in which silymarin and its active constituent silibinin help protect the liver, including boosting the liver cells’ own natural protective processes, while simultaneously decreasing a number of inflammatory mediators (these include iNOS, tumor necrosis factor alpha,23,24 interleukins-6 25 and 1 beta,26,27 cycoloxygenase-2 [COX-2], and nuclear factor kappa-beta [NF-kappaB]).28,29
These beneficial properties are believed to be responsible for silymarin’s ability to prevent, and in some cases reverse, liver disease—all of which represent inflammation-induced accelerated aging.30,31
The Real Leading Cause Of Liver Damage

Liver disease was historically considered to be the result of excessive alcohol consumption. However, the single leading cause of liver disease is the direct result of excess weight.3,4,12,32 Nonalcoholic fatty liver disease (NAFLD) is closely associated with obesity and high blood sugar.1
NAFLD is defined by the presence of excessive fat stores in liver cells, which normally contain very little fat. Between 30 to 50% of adults in developed countries suffer from NAFLD—and most don’t know it.1,9-11
This is worrisome, since up to one-third of NAFLD patients will progress to a more severe condition known as nonalcoholic steatohepatitis, or NASH.1, 9,10 NASH is inflammation of the liver caused by excess fat. This type of liver injury leads directly to liver fibrosis, or scarring, which destroys most of the liver’s natural functions.1,33 We also know that inflammation in general promotes cancer, which helps explain why NASH is now considered a major risk factor for hepatocellular carcinoma, the most common form of primary liver cancer.1,15,34
Fortunately, silymarin’s anti-inflammatory action makes it especially powerful against NAFLD, as evidenced from a broad range of laboratory and clinical studies.
Animal Studies
In a study published in International Journal of Molecular Medicine, silymarin treatment of obese, diabetic rats was shown to help prevent liver fibrosis by decreasing activation of stellate cells. These cells produce fibrosis (scarring of the liver) thereby indicating the beginning of liver failure.35,36 These antifibrotic effects are attributed to the ability of silymarin to disrupt inflammatory cytokines—particularly TNF-alpha, which is known to drive the progression of NAFLD to the more deadly NASH.36-38
Another study found that when rats fed a high-fat diet to develop NAFLD were supplemented with silibinin, they experienced a significant reduction in the features associated with NAFLD, including microscopic changes to the liver, insulin resistance, and dysfunction of glucose metabolism.19
In the same study, researchers incubated liver cells with fat to encourage them to fill with lipids (simulating NAFLD). Researchers found that the addition of silibinin to the culture reduced lipid accumulation, restored cells’ viability, and lowered production of the protein resistin, a marker of insulin resistance, which is significantly associated with NAFLD and metabolic syndrome.
Other animal studies have shown a reduction in mean liver weight (a measure of fat accumulation) in mice whose NAFLD had progressed to dangerous NASH, demonstrating that milk thistle extracts can in fact reverse this deadly progression.39
What you need to know
 |
Milk Thistle Extract Provides Liver Protection
- Threats to liver function include weight gain, poor blood sugar control, metabolic syndrome, toxins in food and the environment, and several dangerous viruses.
- One of the leading causes of liver disease today is nonalcoholic fatty liver disease (NAFLD), which while producing no symptoms, can progress to liver fibrosis, cirrhosis, and premature death.
- No drug is available to cure or even adequately treat liver disease once it develops.
- Silymarin, a flavonoid-rich extract of milk thistle plant seeds, has specific liver-protective properties.
- Studies show that silymarin fights oxidative damage and inflammation, with real impact on prevention of NAFLD and other liver diseases.
- Silymarin also directly blocks hepatitis C virus infection and may prevent virus replication.
- Early results show potential cancer-chemopreventive effects of silymarin in lab studies.
- Daily supplementation with silymarin from milk thistle might be a great way to maintain liver health and resistance to accelerated aging from metabolic syndrome, diabetes, and obesity.
Human Studies
Human studies of silymarin in NAFLD are equally encouraging. The first such study, published just three years ago, examined vitamin E along with a complex called silybin phytosome complex, which consists of silybin plus phosphatidylcholine, a substance that enhances bioavailability. After just 12 months, the patients experienced significant improvements in markers of liver cell damage, glucose tolerance, and the microscopic structure of the liver; no such changes were seen in placebo recipients.8
Surprisingly, the body mass index (BMI) of the patients in the study, which had previously been elevated, normalized in 15% of treated subjects, but only in 2% of placebo patients. In addition, when patients with hepatitis C infection were treated with the supplement, they showed improvement in markers of fibrosis, while no such change was seen in hepatitis C patients who received the placebo, a demonstration of the multiple targets on which silymarin and silybin can act.
In a similar study, when 72 patients with NAFLD took a supplement containing silymarin, blood markers of liver damage fell significantly by about 45% in just three months.40 During that time period, researchers also noted significant improvement in the ultrasound appearance of the liver before and after treatment.
But one of the most exciting studies came in late 2014, when researchers published the first demonstration in humans of silymarin’s potential to reverse NASH, the dangerous progression of NAFLD.41
For the study, patients with existing NASH supplemented with 210 mg of silymarin daily and underwent blood tests before and after treatment. After eight weeks, supplemented patients had a 58% reduction in the liver enzyme ALT, while placebo recipients experienced a 38% reduction, a significant difference; similar decreases were found in other liver enzyme markers.
(Note: Placebo patients often exhibit some benefit when participating in clinical studies because they initiate changes on their own, such as losing weight, due to the education they receive from the paperwork they sign and the physician interactions that occur. In other words, patients are told their poor lifestyle choices have created a life-threatening condition and many instinctively take steps to correct their problem.)
Given the lack of drug options for NAFLD, scientists have also attempted to evaluate drugs used in diabetes as a means of controlling the progress of the disorder. In one such study, silymarin proved superior to two such drugs (metformin and pioglitazone) in reducing blood markers of liver damage.34
NAFLD Emerges As A Pediatric Health Threat
 |
A generation ago, most pediatricians were only vaguely familiar with the concepts of type II diabetes and nonalcoholic fatty liver disease (NAFLD). Children and adolescents were generally thought not to suffer from these “age-related” conditions.
Today, however, it is clear that all of these metabolic disruptions form part of the metabolic syndrome (obesity, lipid disturbances, elevated blood sugar, and hypertension), which leads directly to cardiovascular,69 neurodegenerative,70,71 and malignant diseases,72,73 regardless of age. In other words, these conditions are not so much “age-related” as they are “age-accelerating.”74,75
These changes are being brought to light by a host of alarming studies revealing a rapidly growing suspected prevalence of NAFLD in adolescents and even young children. In the period between 1988 and 1994, NAFLD prevalence was 3.9% in those aged 12-19 years; by 2007-2010, prevalence was 10.7% with that dramatic increase evenly distributed among all racial and ethnic groups and both sexes.6 Forty-eight percent of obese teen boys are estimated to have NAFLD,6 and NAFLD is now the most common cause of chronic liver disease in children and adolescents in the US, strongly associated with childhood obesity, insulin resistance, and metabolic syndrome.7
With no approved pharmacological treatments, lifestyle and dietary therapies remain the only hope for stemming the tide of NAFLD in children, adolescents, and adults.7,8
In addition, studies have shown that supplementation with the milk thistle extract silymarin can protect against liver damage from NAFLD. 39,76
Obesity And Diabetes
In addition to having a direct impact on liver disease, silymarin has also been found to help battle conditions that can contribute to liver disease, including obesity and diabetes.
Underlying the epidemic of NAFLD in America is the epidemic of obesity, which is so closely related to development of type II diabetes42 that the two are commonly referred to as a single problem: diabesity.43 Both diabetes and obesity contribute to metabolic syndrome, which accelerates aging by contributing to premature cardiovascular, neurodegenerative, and malignant diseases.44-47
Fortunately, silymarin is showing tremendous promise in protecting the liver against the age-accelerating impact of diabesity and metabolic syndrome. Studies of obese and/or diabetic animals show that silymarin and silibinin lower cellular and circulating levels of oxidative stress and inflammatory markers. These actions result in greater responsiveness to insulin, better glucose control, diminished fat production, better endothelial function (a risk factor for cardiovascular disease), and improved cognition,48,49 when compared with untreated animals.22,50-54
But in one of the most remarkable animal studies to date, researchers found that silymarin can induce a true reversal of diabetic neuropathy, which is painful nerve damage caused by chronic blood sugar elevations.55 This is an especially exciting development since diabetic neuropathy has so far proved resistant to conventional drug treatment.
Diabetes also damages kidney tissue and leads to impaired kidney function, a condition called diabetic nephropathy, which is a leading cause of kidney failure. In rat studies, silymarin treatment has been found to markedly restore kidney tissue damaged by diabetes and significantly improve impaired kidney function, largely by restoring diminished levels of natural enzyme systems.21,54
Studies In Human Diabetics Reinforce Lab Findings
Studies published between 1997 and 2007 found that diabetic subjects taking 600 mg a day of silymarin experienced numerous benefits, including significant decreases in fasting blood sugar, mean daily blood sugar, sugar in the urine, and long-term measures of glucose exposure (such as hemoglobin A1c), as well as in total insulin requirements in insulin-using patients.56-58 They also experienced improved liver function, as shown by decreases in triglycerides, total and LDL (“bad”) cholesterol, and enzyme markers of liver damage.57
Studies have also found that silymarin can help enhance the benefits of standard diabetic drugs. For example, in patients whose diabetes was poorly controlled on the prescription drug glibenclamide, the addition of 200 mg a day of silymarin for 120 days produced improvements over the drug alone, while also significantly reducing body mass index (BMI).58 And another study found that when silymarin was added to standard drugs for diabetic nephropathy (kidney disease), patients experienced improved urinary markers of kidney function, inflammation, and oxidative damage beyond that produced by the drug itself.59
Enhancing Silymarin With Phospholipids
 |
Silymarin holds tremendous potential for treating and preventing chronic liver diseases. Unfortunately, the extract alone is poorly soluble in fat, which slows its transport across lipid-rich cell membranes and may diminish its availability to the body (bioavailability) following oral dosing.77
This problem can be readily overcome by allowing the silybin components to form complexes with phospholipids, which are detergent-like molecules that facilitate the mixing of water- and fat-soluble compounds.8,77-79
Studies in both animals and humans show that a complex of silybin plus the phospholipid phosphatidylcholine produces greater oral bioavailability than pure silybin and silymarin.78,79 The impact of this phytosome complex was demonstrated quantitatively in dogs, which showed increases in the maximum concentration of silybin by 2.7-fold and in the total 24-hour accumulation of silybin by 3-fold, and shortened the time to achieve maximum concentration to 60% of that of silybin.80
Silymarin Shows Early Promise Against Many Cancer Types
Key events in the development of cancer very often include oxidative damage to cells with resultant inflammation, followed by an accelerated rate of cell replication and a resistance to normal cell death (apoptosis).
These features of cancer represent target areas that might be vulnerable to treatment with silymarin. There is growing interest among oncologists to capitalize on the supplement’s strong safety record and evidence of effectiveness in laboratory studies.
While no clinical data on silymarin as a cancer-preventive agent are yet available, the accumulation of basic laboratory findings is compelling and provides hope for the near future. For instance:
- Laboratory studies show that silymarin blocks proliferation in colon, lung, cervical, prostate, and ovarian cancer cell lines in culture.60-64
- Silymarin has been found to have a synergistic effect with known cancer chemotherapy drugs.60
- Silymarin blocks the master inflammation-generating complex NF-kappaB, decreasing further signaling that is regulated by this inflammatory molecule.61
- Silymarin restores cancer cells’ ability to die by apoptosis, which allows the body’s own scavenging and surveillance systems to clean up and prevent further tumor growth.61-63
- Silymarin can inhibit the invasiveness of certain types of cancer cells, a major step in limiting the severity of a malignancy.62,65
Excitingly, when silibinin was orally administered in mice bearing human lung cancer grafts, it sharply decreased the overall volumes of the resulting tumors, even in tumors known to be resistant to standard chemotherapy.66 Researchers found that silibinin prevented the transition from well-differentiated epithelial cells to more motile, and potentially invasive, mesenchymal cells.67,68 This epithelial-to-mesenchymal transition is a requirement for many tumor types to develop and grow, so blocking it is a major advance.66
Human studies of silymarin and cancer are in their infancy, but dose-finding studies have revealed safety and tolerability of the supplement while other studies show promise with encapsulating silymarin into tiny nanoparticles to markedly enhance its bioavailability to levels required for cancer treatment.61,64
Why The Liver Is So Important
 |
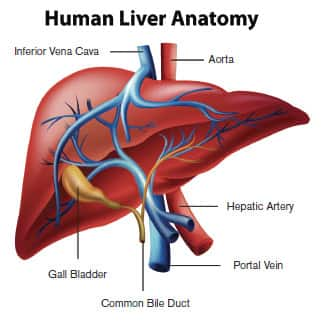
It is impossible to overstate the liver’s importance for health and longevity. Your liver processes the nutrients you need to survive and thrive from the food you eat. It manufactures scores of enzymes and other factors vital to blood clotting,81 to the immune system,82 and to metabolic control of blood sugar83 and lipid levels.84 It makes bile,85 which helps you digest and absorb fats. It stores sugar safely, releasing it as required to sustain energy requirements.85 It detoxifies the majority of chemical toxins we ingest, including alcohol 86 and most drugs.87 It stores minerals, such as iron and copper, as well as certain vitamins.88
Unfortunately, your liver is under constant attack, especially from natural and artificial toxins.89-91 Making matters worse, it is host to several potentially fatal viral infections, and also to hepatocellular carcinoma, a leading cause of cancer deaths.15,92-96
Because 100% of blood from the digestive tract goes straight to the liver for further processing, the liver is constantly exposed to high levels of fats, sugars, and potentially damaging chemicals from food.88,97,98 It is highly sensitive to fluctuations in blood sugar 99,100 and especially to the effects of obesity, which conspire to produce a chronic liver condition called nonalcoholic fatty liver disease, a condition suffered by nearly one-third of American adults.1,19
Currently, there are no drugs available that can prevent liver disease, or treat it once it has become established. But studies have shown that silymarin, an extract of the milk thistle, can do what no mainstream treatment can: It can provide potent protection against liver damage from NAFLD—and can even reverse NASH, the dangerous progression of NAFLD.41,101 Silymarin has also been found to reduce liver damage from diabetes and obesity.
By fighting oxidant damage and inflammation, silymarin can have a real impact on prevention of NAFLD and other dangerous liver diseases.
Summary
The epidemic of obesity and the metabolic syndrome are responsible for a growing threat to health and longevity: liver disease.
More than 30% of Americans have dangerous accumulations of fat in their liver, a condition called nonalcoholic fatty liver disease (NAFLD). This condition is especially dangerous because it is often without symptoms—meaning most people are unaware they have this condition. This “silent” disease leads to potentially fatal liver conditions, including nonalcoholic steatohepatitis (NASH) and ultimately fibrosis, cirrhosis, and liver failure.
No medications are approved for prevention, or even treatment, of most liver disorders. That means that lifestyle and dietary changes provide the best hope for avoiding these debilitating and deadly conditions. While weight loss and exercise are important, you can further tip the odds in your favor by supplementing with silymarin, the standardized extract of the milk thistle seed.
Studies show that silymarin and its active constituent silibinin provide potent protection against liver damage from NAFLD, in at least one case, genuinely reversing some of the more ominous findings. Silymarin has also been found to reduce liver damage from diabetes and obesity.
Finally, there is growing evidence that silymarin and its constituents have powerful anticancer capabilities that work on multiple cellular targets.
Silymarin is currently the best-studied and most effective means of protecting against chronic liver disease.
If you have any questions on the scientific content of this article, please call a Life Extension® Health Advisor at 1-866-864-3027.
Editor's Note
Science continues to evolve, and new research is published daily. As such, we have a more recent article on this topic: Milk Thistle Promotes Liver Detoxification
References
- Dietrich P, Hellerbrand C. Nonalcoholic fatty liver disease, obesity and the metabolic syndrome. Best Pract Res Clin Gastroenterol. 2014 Aug;28(4):637-53.
- Paschos P, Paletas K. Non-alcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009 Jan;13(1):9-19.
- Tolman KG, Dalpiaz AS. Treatment of nonalcoholic fatty liver disease. Ther Clin Risk Manag. 2007 Dec;3(6):1153-63.
- Loomba R, Sirlin CB, Schwimmer JB, Lavine JE. Advances in pediatric nonalcoholic fatty liver disease. Hepatology. 2009 Oct;50(4):1282-93.
- Xu YZ, Zhang X, Wang L, Zhang F, Qiu Q, Liu ML, Zhang GR, Wu XL. An increased circulating angiotensin II concentration is associated with hypoadiponectinemia and postprandial hyperglycemia in men with nonalcoholic fatty liver disease. Intern Med. 2013;52(8):855-61.
- Welsh JA, Karpen S, Vos MB. Increasing prevalence of nonalcoholic fatty liver disease among United States adolescents, 1988-1994 to 2007-2010. J Pediatr. 2013 Mar;162(3):496-500.e1.
- Aggarwal A, Puri K, Thangada S, Zein N, Alkhouri N. Nonalcoholic fatty liver disease in children: recent practice guidelines, where do they take us? Curr Pediatr Rev. 2014;10(2):151-61.
- Loguercio C, Andreone P, Brisc C, et al. Silybin combined with phosphatidylcholine and vitamin E in patients with nonalcoholic fatty liver disease: a randomized controlled trial. Free Radic Biol Med. 2012 May 1;52(9):1658-65.
- Pan JJ, Fallon MB. Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol. 2014 May 27;6(5):274-83.
- Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003 May;37(5):1202-19.
- Lazo M, Hernaez R, Eberhardt MS, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2013 Jul 1;178(1):38-45.
- Alazawi W, Mathur R, Abeysekera K, et al. Ethnicity and the diagnosis gap in liver disease: a population-based study. Br J Gen Pract. 2014 Nov;64(628):e694-702.
- Videla LA, Rodrigo R, Orellana M, et al. Oxidative stress-related parameters in the liver of nonalcoholic fatty liver disease patients. Clin Sci (Lond). 2004 Mar;106(3):261-8.
- Dowman JK, Tomlinson JW, Newsome PN. Pathogenesis of nonalcoholic fatty liver disease. QJM. 2010 Feb;103(2):71-83.
- Bishayee A. The role of inflammation and liver cancer. Adv Exp Med Biol. 2014;816:401-35.
- Sherif IO, Al-Gayyar MM. Antioxidant, anti-inflammatory and hepatoprotective effects of silymarin on hepatic dysfunction induced by sodium nitrite. Eur Cytokine Netw. 2013 Jul-Sep;24(3):114-21.
- Féher J, Lengyel G. Silymarin in the prevention and treatment of liver diseases and primary liver cancer. Curr Pharm Biotechnol. 2012 Jan;13(1):210-7.
- Vargas-Mendoza N, Madrigal-Santillan E, Morales-Gonzalez A, et al. Hepatoprotective effect of silymarin. World J Hepatol. 2014 Mar 27;6(3):144-9.
- Zhang Y, Hai J, Cao M, et al. Silibinin ameliorates steatosis and insulin resistance during nonalcoholic fatty liver disease development partly through targeting IRS-1/PI3K/Akt pathway. Int Immunopharmacol. 2013 Nov;17(3):714-20.
- Marrazzo G, Bosco P, La Delia F, et al. Neuroprotective effect of silibinin in diabetic mice. Neurosci Lett. 2011 Oct 31;504(3):252-6.
- Soto C, Perez J, Garcia V, Uria E, Vadillo M, Raya L. Effect of silymarin on kidneys of rats suffering from alloxan-induced diabetes mellitus. Phytomedicine. 2010 Dec 1;17(14):1090-4.
- Soto C, Recoba R, Barron H, Alvarez C, Favari L. Silymarin increases antioxidant enzymes in alloxan-induced diabetes in rat pancreas. Comp Biochem Physiol C Toxicol Pharmacol. 2003 Nov;136(3):205-12.
- Song Z, Deaciuc I, Song M, Lee DY, Liu Y, Ji X, McClain C. Silymarin protects against acute ethanol-induced hepatotoxicity in mice. Alcohol Clin Exp Res. 2006 Mar;30(3):407-13.
- Al-Anati L, Essid E, Reinehr R, Petzinger E. Silibinin protects OTA-mediated TNF-alpha release from perfused rat livers and isolated rat Kupffer cells. Mol Nutr Food Res. 2009 Apr;53(4):460-6.
- Zhang W, Hong R, Tian T. Silymarin’s protective effects and possible mechanisms on alcoholic fatty liver for rats. Biomol Ther (Seoul). 2013 Jul 30;21(4):264-9.
- Au AY, Hasenwinkel JM, Frondoza CG Silybin inhibits interleukin-1beta-induced production of pro-inflammatory mediators in canine hepatocyte cultures. J Vet Pharmacol Ther 2011(34):120-9.
- Bousserouel S, Bour G, Kauntz H, Gossé F, Marescaux J, Raul F. Silibinin inhibits tumor growth in a murine orthotopic hepatocarcinoma model and activates the TRAIL apoptotic signaling pathway. Anticancer Res. 2012 Jul;32(7):2455-62.
- Ahmad AHRi, Hossein R, Akram M. The inhibitory effect of Silymarin on Cell viability and cellular COX-2 and iNOS level in HepG2 cell line. HealthMed. 2013;7(7):2008.
- Saliou C1, Rihn B, Cillard J, Okamoto T, Packer L. Selective inhibition of NF-kappaB activation by the flavonoid hepatoprotector silymarin in HepG2. Evidence for different activating pathways FEBS Lett. 1998 Nov 27;440(1-2):8-12.
- Al-Anati L, Essid E, Reinehr R, Petzinger E. Silibinin protects OTA-mediated TNF-alpha release from perfused rat livers and isolated rat Kupffer cells. Mol Nutr Food Res. 2009 Apr;53(4):460-6.
- Jayaraj R, Deb U, Bhaskar AS, Prasad GB, Rao PV. Hepatoprotective efficacy of certain flavonoids against microcystin induced toxicity in mice. Environ Toxicol. 2007 Oct;22(5):472-9.
- Kneeman JM, Misdraji J, Corey KE. Secondary causes of nonalcoholic fatty liver disease. Therap Adv Gastroenterol. 2012 May;5(3):199-207.
- Firneisz G. Nonalcoholic fatty liver disease and type 2 diabetes mellitus: the liver disease of our age? World J Gastroenterol. 2014 Jul 21;20(27):9072-89.
- Hajiaghamohammadi AA, Ziaee A, Oveisi S, Masroor H. Effects of metformin, pioglitazone, and silymarin treatment on nonalcoholic Fatty liver disease: a randomized controlled pilot study. Hepat Mon. 2012 Aug;12(8):e6099.
- Moreira RK. Hepatic stellate cells and liver fibrosis. Arch Pathol Lab Med. 2007 Nov;131(11):1728-34.
- Kim M, Yang SG, Kim JM, Lee JW, Kim YS, Lee JI. Silymarin suppresses hepatic stellate cell activation in a dietary rat model of nonalcoholic steatohepatitis: analysis of isolated hepatic stellate cells. Int J Mol Med. 2012 Sep;30(3):473-9.
- Basaranoglu M, Basaranoglu G, Senturk H. From fatty liver to fibrosis: a tale of “second hit”. World J Gastroenterol. 2013 Feb 28;19(8):1158-65.
- Zahran WE, Salah El-Dien KA, Kamel PG, El-Sawaby AS. Efficacy of Tumor Necrosis Factor and Interleukin-10 Analysis in the Follow-up of Nonalcoholic Fatty Liver Disease Progression. Indian J Clin Biochem. 2013 Apr;28(2):141-6.
- Pais P, D’Amato M. In vivo efficacy study of milk thistle extract (ETHIS-094) in STAM model of nonalcoholics. Drugs R D. 2014 Dec;14(4):291-9.
- Cacciapuoti F, Scognamiglio A, Palumbo R, Forte R, Cacciapuoti F. Silymarin in non alcoholic fatty liver disease. World J Hepatol. 2013 Mar 27;5(3):109-13.
- Solhi H, Ghahremani R, Kazemifar AM, Hoseini Yazdi Z. Silymarin in treatment of nonalcoholic steatohepatitis: A randomized clinical trial. Caspian J Intern Med. 2014 Winter;5(1):9-12.
- Lam B, Younossi ZM. Treatment options for nonalcoholic fatty liver disease. Therap Adv Gastroenterol. 2010 Mar;3(2):121-37.
- Farag YM, Gaballa MR. Diabesity: an overview of a rising epidemic. Nephrol Dial Transplant. 2011 Jan;26(1):28-35.
- Barzilay JI, Stein PK. Association of the metabolic syndrome with age-related, nonatherosclerotic, chronic medical conditions. Metab Syndr Relat Disord. 2011 Oct;9(5):327-35.
- Businaro R, Ippoliti F, Ricci S, Canitano N, Fuso A. Alzheimer’s disease promotion by obesity: induced mechanisms-molecular links and perspectives. Curr Gerontol Geriatr Res. 2012;2012:986823.
- Morley JE. Diabetes and aging: epidemiologic overview. Clin Geriatr Med. 2008 Aug;24(3):395-405, v.
- Otabe S, Wada N, Hashinaga T, et al. Hyperadiponectinemia protects against premature death in metabolic syndrome model mice by inhibiting AKT signaling and chronic inflammation. J Endocrinol. 2012 Apr;213(1):67-76.
- Neha, Kumar A, Jaggi AS, Sodhi RK, Singh N. Silymarin ameliorates memory deficits and neuropathological changes in mouse model of high-fat-diet-induced experimental dementia. Naunyn Schmiedebergs Arch Pharmacol. 2014 Aug;387(8):777-87.
- Marrazzo G, Bosco P, La Delia F, Scapagnini G, Di Giacomo C, Malaguarnera M, Galvano F, Nicolosi A, Li Volti G. Neuroprotective effect of silibinin in diabetic mice. Neurosci Lett. 2011 Oct 31;504(3):252-6.
- Bouderba S, Sanchez-Martin C, Villanueva GR, Detaille D, Koceir EA. Beneficial effects of silibinin against the progression of metabolic syndrome, increased oxidative stress, and liver steatosis in Psammomys obesus, a relevant animal model of human obesity and diabetes. J Diabetes. 2014 Mar;6(2):184-92.
- Li Volti G, Salomone S, Sorrenti V, et al. Effect of silibinin on endothelial dysfunction and ADMA levels in obese diabetic mice. Cardiovasc Diabetol. 2011;10:62.
- Prakash P, Singh V, Jain M, et al. Silymarin ameliorates fructose induced insulin resistance syndrome by reducing de novo hepatic lipogenesis in the rat. Eur J Pharmacol. 2014 Mar 15;727:15-28.
- Srivastava RK, Sharma S, Verma S, Arora B, Lal H. Influence of diabetes on liver injury induced by antitubercular drugs and on silymarin hepatoprotection in rats. Methods Find Exp Clin Pharmacol. 2008 Dec;30(10):731-7.
- Sheela N, Jose MA, Sathyamurthy D, Kumar BN. Effect of silymarin on streptozotocin-nicotinamide-induced type 2 diabetic nephropathy in rats. Iran J Kidney Dis. 2013 Mar;7(2):117-23.
- Baluchnejadmojarad T, Roghani M, Khastehkhodaie Z. Chronic treatment of silymarin improves hyperalgesia and motor nerve conduction velocity in diabetic neuropathic rat. Phytother Res. 2010 Aug;24(8):1120-5.
- Velussi M, Cernigoi AM, De Monte A, Dapas F, Caffau C, Zilli M. Long-term (12 months) treatment with an anti-oxidant drug (silymarin) is effective on hyperinsulinemia, exogenous insulin need and malondialdehyde levels in cirrhotic diabetic patients. J Hepatol. 1997 Apr;26(4):871-9.
- Huseini HF, Larijani B, Heshmat R, et al. The efficacy of Silybum marianum (L.) Gaertn. (silymarin) in the treatment of type II diabetes: a randomized, double-blind, placebo-controlled, clinical trial. Phytother Res. 2006 Dec;20(12):1036-9.
- Hussain SA. Silymarin as an adjunct to glibenclamide therapy improves long-term and postprandial glycemic control and body mass index in type 2 diabetes. J Med Food. 2007 Sep;10(3):543-7.
- Fallahzadeh MK, Dormanesh B, Sagheb MM, et al. Effect of addition of silymarin to renin-angiotensin system inhibitors on proteinuria in type 2 diabetic patients with overt nephropathy: a randomized, double-blind, placebo-controlled trial. Am J Kidney Dis. 2012 Dec;60(6):896-903.
- Colombo V, Lupi M, Falcetta F, Forestieri D, D’Incalci M, Ubezio P. Chemotherapeutic activity of silymarin combined with doxorubicin or paclitaxel in sensitive and multidrug-resistant colon cancer cells. Cancer Chemother Pharmacol. 2011 Feb;67(2):369-79.
- Li W, Mu D, Song L, et al. Molecular mechanism of silymarin-induced apoptosis in a highly metastatic lung cancer cell line anip973. Cancer Biother Radiopharm. 2011 Jun;26(3):317-24.
- Yu HC, Chen LJ, Cheng KC, Li YX, Yeh CH, Cheng JT. Silymarin inhibits cervical cancer cell through an increase of phosphatase and tensin homolog. Phytother Res. 2012 May;26(5):709-15.
- Fan L, Ma Y, Liu Y, Zheng D, Huang G. Silymarin induces cell cycle arrest and apoptosis in ovarian cancer cells. Eur J Pharmacol. 2014 Nov 15; 743:79-88.
- Snima KS, Arunkumar P, Jayakumar R, Lakshmanan VK. Silymarin encapsulated poly(D,L-lactic-co-glycolic acid) nanoparticles: a prospective candidate for prostate cancer therapy. J Biomed Nanotechnol. 2014 Apr;10(4):559-70.
- Vaid M, Prasad R, Sun Q, Katiyar SK. Silymarin targets β-catenin signaling in blocking migration/invasion of human melanoma cells. PLoS One. 2011;6(7):e23000.
- Cufi S, Bonavia R, Vazquez-Martin A, et al. Silibinin meglumine, a water-soluble form of milk thistle silymarin, is an orally active anti-cancer agent that impedes the epithelial-to-mesenchymal transition (EMT) in EGFR-mutant non-small-cell lung carcinoma cells. Food Chem Toxicol. 2013 Oct;60:360-8.
- Battula VL, Evans KW, Hollier BG, Shi Y, Marini FC, Ayyanan A, Wang RY, Brisken C, Guerra R, Andreeff M, Mani SA. Epithelial-mesenchymal transition-derived cells exhibit multilineage differentiation potential similar to mesenchymal stem cells. Stem Cells. 2010 Aug;28(8):1435-45.
- Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003 Dec;112(12):1776-84.
- Galassi A, Reynolds K, He J.Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006 Oct;119(10):812-9.
- Ashrafian H, Harling L, Darzi A, Athanasiou T. Neurodegenerative disease and obesity: what is the role of weight loss and bariatric interventions? Metab Brain Dis. 2013 Sep;28(3):341-53.
- Cai D. Neuroinflammation and neurodegeneration in overnutrition-induced diseases. Trends Endocrinol Metab. 2013 Jan;24(1):40-7.
- Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D. Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care . 2012 Nov;35(11):2402-11.
- Pothiwala P, Jain SK, Yaturu S. Metabolic syndrome and cancer. Metab Syndr Relat Disord. 2009 Aug;7(4):279-88.
- Franke K, Ristow M, Gaser C. Gender-specific impact of personal health parameters on individual brain aging in cognitively unimpaired elderly subjects. Front Aging Neurosci. 2014;6:94.
- Takahashi K, Takatsu M, Hattori T, et al. Premature cardiac senescence in DahlS.Z-Lepr(fa)/Lepr(fa) rats as a new animal model of metabolic syndrome. Nagoya J Med Sci. 2014 Feb;76(1-2):35-49.
- Hikino H, Kiso Y, Wagner H, Fiebig M. Antihepatotoxic actions of flavonolignans from Silybum marianum fruits. Planta Med. 1984 Jun;50(3):248-50.
- Song Y, Zhuang J, Guo J, Xiao Y, Ping Q. Preparation and properties of a silybin-phospholipid complex. Pharmazie. 2008 Jan;63(1):35-42.
- Barzaghi N, Crema F, Gatti G, Pifferi G, Perucca E. Pharmacokinetic studies on IdB 1016, a silybin- phosphatidylcholine complex, in healthy human subjects. Eur J Drug Metab Pharmacokinet. 1990 Oct-Dec;15(4):333-8.
- Yanyu X, Yunmei S, Zhipeng C, Qineng P. The preparation of silybin-phospholipid complex and the study on its pharmacokinetics in rats. Int J Pharm. 2006 Jan 3;307(1):77-82.
- Filburn CR, Kettenacker R, Griffin DW. Bioavailability of a silybin-phosphatidylcholine complex in dogs. J Vet Pharmacol Ther. 2007 Apr;30(2):132-8.
- Mammen EF. Coagulation abnormalities in liver disease. Hematol Oncol Clin North Am. 1992 Dec;6(6):1247-57.
- Kmieć Z. Cooperation of liver cells in health and disease. Adv Anat Embryol Cell Biol. 2001;161:III-XIII, 1-151.
- Nordlie RC, Foster JD, Lange AJ. Regulation of glucose production by the liver. Annu Rev Nutr. 1999;19:379-406.
- Xu X, So JS, Park JG, Lee AH. Transcriptional control of hepatic lipid metabolism by SREBP and ChREBP. Semin Liver Dis. 2013 Nov;33(4):301-11.
- Berg JM, Tymoczko JL, Stryer L. Biochemistry. 5th edition. New York: W H Freeman; 2002.
- Cederbaum AI. Alcohol metabolism. Clin Liver Dis. 2012 Nov;16(4):667-85.
- Grant DM. Detoxification pathways in the liver. J Inherit Metab Dis. 1991;14(4):421-30.
- Available at: http://www.ncbi.nlm.nih.gov/pubmedhealth/pmh0015941. Accessed January 23, 2015.
- Malaguarnera G, Cataudella E, Giordano M, Nunnari G, Chisari G, Malaguarnera M. Toxic hepatitis in occupational exposure to solvents. World J Gastroenterol. 2012 Jun 14;18(22):2756-66.
- Meng Z, Wang Y, Wang L, Jin et al. FXR regulates liver repair after CCl4-induced toxic injury. Mol Endocrinol. 2010 May;24(5):886-97.
- Li Z, Diehl AM. Innate immunity in the liver. Curr Opin Gastroenterol. 2003 Nov;19(6):565-71.
- Reddy KR, Belle SH, Fried MW, et al. Rationale, challenges, and participants in a Phase II trial of a botanical product for chronic hepatitis C. Clin Trials. 2012 Feb;9(1):102-12.
- Ren S, Contreras D, Arumugaswami V. A protocol for analyzing hepatitis C virus replication. J Vis Exp. 2014 (88):e51362.
- Silberstein E, Taylor DR. Overcoming hurdles in hepatitis C virus research: efficient production of infectious virus in cell culture. Int J Biomed Sci. 2008 Jun;4(2):82-8.
- shfaq UA, Javed T, Rehman S, Nawaz Z, Riazuddin S. Inhibition of HCV 3a core gene through Silymarin and its fractions. Virol J. 2011;8:153.
- Kohli A, Murphy AA, Agarwal C, et al. HCC surveillance results in earlier HCC detection: results from an Indian cohort. Springerplus. 2014;3:610.
- Nagengast AK, Hurt RT, Downard CD, Smith JW, Garrison RN, Matheson PJ. Increased hepatic blood flow during enteral immune-enhancing diet gavage requires intact enterohepatic bile cycling. Nutrition. 2014 Mar;30(3):313-8.
- Takeuchi H, Sekine S, Kojima K, Aoyama T. The application of medium-chain fatty acids: edible oil with a suppressing effect on body fat accumulation. Asia Pac J Clin Nutr. 2008;17 Suppl 1:320-3.
- Han S, Ko JS, Jin SM, Park HW, Kim JM, Joh JW, Kim G, Choi SJ. Intraoperative hyperglycemia during liver resection: predictors and association with the extent of hepatocytes injury. PLoS One. 2014 Oct 8;9(10):e109120.
- Berg JM, Tymoczko JL, Stryer L. Biochemistry. 5th edition. New York: W H Freeman; 2002. Section 21.5.
- Haddad Y, Vallerand D, Brault A, Haddad PS. Antioxidant and hepatoprotective effects of silibinin in a rat model of nonalcoholic steatohepatitis. Evid Based Complement Alternat Med. 2011;2011:nep164.

