Life Extension Magazine®
A question we are asked nowadays is, “What causes people to die who take extraordinary steps to remain healthy?” Our response is that in many cases, there is one precipitating catastrophic event that ignites a cascade of degenerative changes that culminate in death. A classic example is an otherwise fit elderly individual who sustains a bone fracture. The combination of trauma, systemic inflammation, loss of mobility, hospital confinement, and psycho-logical stress can result in several diseases emerging that conspire to kill the victim in a relatively short time. Catastrophic events are by no means limited to accidents. Surgical trauma or the impact of temporary loss of blood flow can also initiate a downward spiral from which an aging person never recovers. Aortic stenosis is a catastrophic event that strikes aging individuals, but may be thwarted by a supplement that was introduced in 1999.1,2 It is too early to know for sure, but there is provocative evidence that what members already do to protect against atherosclerosis and bone loss also prevents calcification of the aortic valve.3,4 The Aortic ValveBlood exits the heart to nourish the body from the left ventricle. With each heartbeat, the aortic valve opens (to let blood out) and closes to enable the left ventricle to fill with fresh oxygenated blood from the lungs. In aortic stenosis, the aortic valve narrows and does not open fully. The result is the left heart ventricle enlarges as it desperately tries to force blood out through the constricted aortic valve. If not treated surgically, the aortic valve may either constrict so tightly that blood cannot exit the heart, or congestive heart failure may set in as the left ventricle deteriorates in response to having to squeeze harder to push blood through the narrowed aortic valve.
In the case of aortic stenosis, the catastrophic life-threatening event can emanate from surgical trauma (which can inflict short- and long-term side-effects) and anti-coagulant drugs like warfarin5-8 that will slowly poison a person to death if not used properly. Aortic valve replacement also increases stroke risk even with warfarin.9-11 There is no validated therapy other than surgery to reverse advanced aortic stenosis. Many doctors and their patients have valiantly tried but failed to remove the calcium deposits that constrict the aortic valve. Prevention of this potential catastrophic disease is thus crucial. Prevalence of Aortic StenosisWhile 2-9% of people over age 65 are diagnosed with aortic stenosis,12 48% of those over age 85 have aortic sclerosis, which is the calcification and thickening of the valve without left ventricular constriction.13 Aortic sclerosis is considered a precursor for eventual constriction (obstruction of blood flow out of the heart) that is ultimately diagnosed as aortic stenosis. Most of those with aortic sclerosis succumb to another disease before frank stenosis manifests. Historically, most cases of aortic stenosis were thought to result from the “wear and tear” of aging.14 This perception is changing. Taking steps to protect against calcification and thickening of the aortic valve would be expected to significantly reduce stenosis risk in one’s older years, when surgical procedures are of particular risk. What Causes Aortic Calcification?Calcium is always circulating in the blood. Our body goes to great lengths to maintain calcium blood levels in a very narrow range. Too much or too little blood calcium is invariably fatal.15,16 Lining our arteries and heart valves is a protein that regulates whether or not circulating blood calcium infiltrates (calcifies) our vasculature. The name of this calcium-regulating protein is matrix gamma-carboxyglutamic acid. To avoid having to repeat this tongue-twister again, we will refer to it from now on as MGP. MGP is synthesized in the vascular walls and plays a key role in regulating vascular calcification.7,17-19 Whether MGP allows vascular calcification or inhibits it depends on its state of carboxylation. When MGP is under-carboxylated, vascular calcification spontaneously occurs.18,20 When MGP is fully carboxylated, it functions as a potent inhibitor of vascular calcification.21-23
Carboxylation of MGP is dependent on vitamin K. In fact, MGP is classified as a vitamin K-dependent protein because it cannot shield against calcification without adequate vitamin K.1,24,25 Epidemic of Systemic CalcificationIn the aged population, vascular calcification is ubiquitous. Autopsy reports show that 75-95% of men and women suffer some degree of vascular calcification.26 Since calcification occurs in soft tissues throughout our body, including the kidneys, lungs, heart, and brain, this calcification epidemic is of great concern to those seeking to avoid a “catastrophic event” that precipitates a lethal downward spiral.27,28 It is fortunate that we are not dependent on a future breakthrough discovery to protect against vascular calcification as it may be prevented by correcting a vitamin K deficiency.29-32 |
Human Clinical DataAn interesting study published in 2008 measured the amount of under-carboxylated MGP in the blood of healthy individuals and compared it to those with severe vascular diseases including aortic stenosis. The findings showed that virtually all diseased subjects had under-carboxylated MGP levels below the normal adult range.20 If only these individuals with severe vascular disease had maintained adequate vitamin K status, they may not have been on death’s door. The most frequently cited data about vitamin K and vascular disease risk came from a study of more than 4,800 subjects who were followed for 7-10 years in the Netherlands. People in the highest one-third of vitamin K2 intake had a 57% reduction in risk of dying from cardiovascular disease, compared to those with the lowest intake. In the group with the highest vitamin K2 intake, risk of severe aortic calcification plummeted by 52%.2 It is doubtful that any of these European study subjects were taking vitamin K supplements. This means that just the tiny microgram amounts obtained in their diets is what may have produced this 52% reduction in risk of severe aortic calcification. Based on findings that maximal carboxylation of MGP requires significantly higher levels of vitamin K than obtained through diet, those taking vitamin K supplements might obtain greater benefit.33-36 The missing part of this puzzle is controlled clinical studies showing that vitamin K supplements themselves prevent aortic stenosis. Instead, we rely on intriguing clinical data that consistently show low vitamin K status in those who develop aortic valve calcification.1,35-37 We know that vitamin K is essential for MGP-carboxylation, which in turn shields heart valves and arteries from pathological calcification.37 We also know that vascular calcification is an active and therefore potentially preventable process if vitamin K intake is increased.38,39
Other Factors Involved in Aortic StenosisLike the modern day scourge of atherosclerosis, there are many risk factors for aortic stenosis.
While the majority of individuals who develop coronary atherosclerosis do not suffer aortic stenosis, the two diseases nonetheless share common risk factors.44 Those with elevated LDL,45-47 triglycerides,48,49 total cholesterol,50-53 and other atherogenic lipids have higher rates of aortic stenosis. Elevated C-reactive protein levels are also correlated with aortic valve disease.54,55 Underlying conditions that predispose people to coronary atherosclerosis such as hypertension,56-59 smoking,60,61 and diabetes62-64 have been consistently linked to the development of aortic stenosis. Other factors associated with aortic stenosis include osteoporosis, which is also strongly associated with vitamin K deficit.65-71 Those suffering from elevated blood calcium,72,73 obesity,60,61,74 and renal failure75-77 have higher incidences of aortic stenosis, which is why annual blood testing is so important to identify correctable problems before irreversible disease takes hold. Please remember that the use of calcium supplements is not the cause of increased blood calcium levels. Healthy persons have an intricate regulatory system that precisely controls how calcium is utilized in the body. When calcium is deficient in the blood, parathyroid hormone acts to remove it from the bone to ensure blood levels are maintained.78 Without adequate calcium intake, parathyroid hormone will continue to remove calcium from bone to the point that a person becomes osteoporotic. Since calcium is required for vital life functions beyond bone density, the body will continuously rob bones of calcium to ensure stable blood levels if there is not sufficient intake from diet or supplements. So the body makes sure there is always enough calcium in the blood to sustain vital life functions. The side effect of the body’s vigilant maintenance of blood calcium is that this calcium is freely available to calcify tissues (including our heart valves). In the presence of enough vitamin K, however, calcium binds to the skeletal matrix where it is needed to maintain bone density and is simultaneously inhibited from infiltrating the vasculature (including arteries and valves).79-81
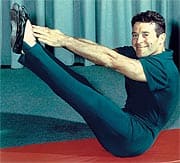
Risk Factors for Aortic Stenosis Overlooked by Most DoctorsIn order for calcium to infiltrate the aortic valve, there is first an initial injury to the endothelium (inner vascular lining).82,83 Homocysteine is a prime culprit that causes the initial endothelial injury that leads to atherosclerosis and possibly aortic stenosis later in life.83-85 What conventional doctors fail to acknowledge today is homocysteine’s role in initiating damage to the vascular system. A group of doctors at the Cleveland Clinic assessed the association between homocysteine levels and various degrees of aortic valve disease in 76 surgical patients. In patients with normal aortic valves, mean homocysteine level was 10.9 (µmol/L). Patients with aortic sclerosis had homocysteine mean levels of 11.4. Those with the more severe aortic stenosis had a significantly higher mean homocysteine level of 15.4! While the small size of this study limited its predictive value, the doctors stated, “It is conceivable that the elevated homocysteine levels seen in patients with renal impairment or older age could contribute to the more rapid progression of aortic stenosis observed in these patient populations.”83 The take-home lesson for anyone concerned about aortic stenosis is that virtually every risk factor for heart attack—be it excess body weight, hypertension, excess blood lipids, and even continued tobacco use—predicts the rate of aortic disease progression. Triumphs and Tragedy of Jack LaLanneIn December 2009, Jack LaLanne at age 95 underwent aortic valve replacement surgery. A little over 13 months later, he died at age 96 of respiratory failure due to pneumonia. Even in healthy elderly individuals, the traumatic impact of aortic valve surgery can be the “catastrophic event” that leads to a rapid downward spiral culminating in death.
There may never be a better example than Jack LaLanne of someone who did virtually everything right, but appears to have missed out on one key nutrient—vitamin K2—that may have prevented calcification of his aortic valve. Jack LaLanne was a pioneer hero who promoted and followed very healthy lifestyle practices—decades before others knew about them. When Jack LaLanne first proposed intensive exercise with weights in 1936, mainstream doctors warned that it would cause all kinds of terrible medical problems. This was the same medical establishment who said cigarette smoking was not dangerous. Jack LaLanne not only promoted lifelong physical activity, but also calorie moderation and avoiding all unhealthy foods. Jack LaLanne’s last book was published in 2003. The supplement regimen he recommended, however, appears to have been trapped in 1970s ideology. He mentioned the importance of vitamin K1 only in the context of normal blood clotting and recommended green leafy vegetables as the main source. We now know, of course, that almost everyone obtains enough vitamin K for their blood to clot, but not nearly enough vitamin K2 to protect against soft tissue calcification. As we often observe with elderly individuals, they tend to remember facts dating back decades but find new concepts difficult to grasp. Out of enormous respect for Jack LaLanne being scientifically ahead of his time regarding healthy eating and exercise, nowhere in his last book is there any mention about other critical steps that aging men should follow, such as maintaining youthful hormone balance. Low DHEA, for example, can compromise immune function,86-90 and the pneumonia Jack LaLanne acutely died of is common in elderly individuals with weakened immunity. We don’t know what supplements Jack LaLanne was using, but based on the recommendations made in his last book, there was no mention of omega-3s, CoQ10, amino acids like carnitine, dipeptides like carnosine, vitamin K2, higher-dose vitamin D, or many of the other nutrients that enlightened individuals take today. In reading Jack LaLanne’s last book (titled Revitalize Your Life), I can confidently state that if everyone in America followed his strict dietary and exercise programs, incidence of today’s major killers would plummet to extremely low levels. Jack LaLanne’s stern recommendations to avoid junk and other unhealthy foods alone could bail this country out of the health care cost crisis it now faces. At the same time we pay tribute to Jack LaLanne’s foresight, we must acknowledge the lethal consequence of omission. New information is published daily that provides clues as to what aging individuals can do to prevent the lethal “catastrophic event” that initiates a downward spiral of endless degenerative disease. When these clues become substantiated in well-controlled human studies, it is imperative for aging individuals to incorporate them into their own daily programs. We fear Jack LaLanne’s omissions may have created his personal catastrophic event. Life Extension Members Enjoy Significant ProtectionThe encouraging news for long-time Life Extension members is that they have been way ahead of the curve in protecting against aortic stenosis. Annual blood tests enable them to take affirmative steps to suppress excess C-reactive protein, LDL, homocysteine, triglycerides, glucose, and other vascular system-destroying factors.97 Members also ingest high-potency supplements that provide 24-hour blood levels of critically important vitamin K2. Long-acting vitamin K2 is emerging as an exciting player in the prevention and potential regression of coronary atherosclerotic plaque. According to some researchers, vitamin K2 has so many functions not associated with vitamin K1 that it should be viewed as a different vitamin entirely. In the largest human study to date, higher intakes of vitamin K2 reduced cardiovascular issues by 57%, whereas intake of vitamin K1 had no effect.2 Those following certain vegetarian diets may not be getting enough vitamin K2, thus exposing themselves to significant calcification disease risk even though they assume they are eating healthy. What is not yet known is whether higher intakes of vitamin K2 will reverse aortic calcification. Based on what has been published to date, there is a considerable basis to believe it will inhibit calcification in tissues throughout our aging bodies, thus reducing our odds of encountering the “catastrophic event” that could prematurely terminate our lives.
For longer life,
William Faloon
| ||||||||||||||||||||||
| References | ||||||||||||||||||||||
| 1. Rennenberg RJ, de Leeuw PW, Kessels AG, et al. Calcium scores and matrix Gla protein levels: association with vitamin K status. Eur J Clin Invest. 2010 Apr;40(4):344-9. 2. Geleijnse JM, Vermeer C, Grobbee DE, et al. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study. J Nutr. 2004 Nov;134(11):3100-5. 3. Schurgers LJ, Dissel PE, Spronk HM, et al. Role of vitamin K and vitamin K-dependent proteins in vascular calcification. Z Kardiol. 2001;90 Suppl 3:57-63. 4. Kidd PM. Vitamins D and K as pleiotropic nutrients: clinical importance to the skeletal and cardiovascular systems and preliminary evidence for synergy. Altern Med Rev. 2010 Sep;15(3):199-222. 5. Wallin R, Martin LF. Warfarin poisoning and vitamin K antagonism in rat and human liver. Design of a system in vitro that mimics the situation in vivo. Biochem J. 1987 Jan 15;241(2):389-96. 6. Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF. Risk of osteoporotic fracture in elderly patients taking warfarin. Arch Intern Med. 2006 Jan 23;166(2):241-6. 7. Koos R, Mahnken AH, Mühlenbruch G, et al. Relation of oral anticoagulation to cardiac valvular and coronary calcium assessed by multislice spiral computed tomography. Am J Cardiol. 2005 Sep 15;96(6):747-9. 8. Schurgers LJ, Aebert H, Vermeer C, Bültmann B, Janzen J. Oral anti-coagulant treatment: friend or foe in cardiovascular disease? Blood. 2004 Nov 15;104(10):3231-2. 9. Caswell J, O’Brien B, Schneck M. Risk of stroke following valve replacement surgery. Seminars in Cerebrovascular Diseases and Stroke. 2003 Dec;3(4):214-8. 10. Ruel M, Masters RG, Rubens FD, et al. Late incidence and determinants of stroke after aortic and mitral valve replacement. Ann Thorac Surg. 2004 Jul;78(1):77-83. 11. Available at: http://www.medscape.com/viewarticle/577915_5. Accessed June 13, 2011. 12. Available at: http://emedicine.medscape.com/article/150638-overview. Accessed June 13, 2011. 13. Pomerance A. Pathogenesis of aortic stenosis and its relation to age. Br Heart J. 1972; 34(6):569–74. 14. Lee JC, Zhao XQ, Otto CM. Aortic valve sclerosis. J Echocardiogr. 2005;3:51-9. 15. Skinner HG, Schwartz GG. Serum calcium and incident and fatal prostate cancer in the National Health and Nutrition Examination Survey. Cancer Epidemiol Biomarkers Prev. 2008 Sep;17(9):2302-5. 16. Canzoniero LM, Snider BJ. Calcium in Alzheimer’s disease pathogenesis: too much, too little or in the wrong place? J Alzheimers Dis. 2005 Nov;8(2):147-54. 17. Spronk HM, Soute BA, Schurgers LJ, et al. Matrix Gla protein accumulates at the border of regions of calcification and normal tissue in the media of the arterial vessel wall. Biochem Biophys Res Commun. 2001 Nov 30;289(2):485–90. 18. Luo G, Ducy P, McKee MD et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature. 1997 Mar 6; 386 (6620):78-81. 19. Zebboudj AF, Shin V, Bostrom K. Matrix GLA protein and BMP-2 regulate osteoinduction in calcifying vascular cells. J Cell Biochem 2003 90:756–65. 20. Cranenburg EC, Vermeer C, Koos R, et al. The circulating inactive form of matrix Gla Protein (ucMGP) as a biomarker for cardiovascular calcification. J Vasc Res. 2008 45(5):427-36. 21. Schurgers LJ, Spronk HM, Skepper JN, et al. Post-translational modifications regulate matrix Gla protein function: importance for inhibition of vascular smooth muscle cell calcification. J Thromb Haemost. 2007 Dec;5(12):2503-11. 22. Shanahan CM, Proudfoot D, Farzaneh-Far A, Weissberg PL. The role of Gla proteins in vascular calcification. Crit Rev Eukaryot Gene Expr. 1998; 8(3-4):357–75. 23. Schurgers LJ, Cranenburg EC, Vermeer C. Matrix Gla-protein: the calcification inhibitor in need of vitamin K. Thromb Haemost. 2008 Oct;100(4):593-603. 24. Vermeer C, Gijsbers BL, Craciun AM, et al. Effects of vitamin K on bone mass and bone metabolism. J Nutr. 1996;126(4 suppl):1187S-91S. 25. Binkley NC, Krueger DC, Engelke JA, et al. Vitamin K supplementation reduces serum concentrations of undergamma-carboxylated osteocalcin in healthy young and elderly adults. Am J Clin Nutr. 2000 Dec; 72(6):1523-8. 26. Available at: http://www.medscape.com/viewarticle/509074. Accessed June 15, 2011. 27. Fraser JD, Price PA. Lung, heart, and kidney express high levels of mRNA for the vitamin K-dependent matrix Gla protein. Implications for the possible functions of matrix Gla protein and for the tissue distribution of the gamma-carboxylase. J Biol Chem. 1988 Aug 15;263(23):11033-6. 28. Fujita D, Terada S, Ishizu H, et al. Immunohistochemical examination on intracranial calcification in neurodegenerative diseases. Acta Neuropathol. 2003 Mar;105(3):259-64. 29. Spronk HM, Soute BA, Schurgers LJ, Thijssen HH, De Mey JG, Vermeer C. Tissue-specific utilization of menaquinone-4 results in the prevention of arterial calcification in warfarin-treated rats. J Vasc Res. 2003 Nov-Dec;40:531–7. 30. Schurgers LJ, Dissel PE, Spronk HM, et al. Role of vitamin K and vitamin K-dependent proteins in vascular calcification. Z Kardiol. 2001;90 Suppl 3:57-63. 31. Shoji S. Vitamin K and vascular calcification. Clin Calcium. 2002 Aug;12(8):1123-8. 32. Cranenburg EC, Schurgers LJ, Vermeer C. Vitamin K: the coagulation vitamin that became omnipotent. Thromb Haemost. 2007 Jul;98(1):120-5. 33. Adams J, Pepping J. Vitamin K in the treatment and prevention of osteoporosis and arterial calcification. Am J Health Syst Pharm. 2005 Aug 1;62(15):1574-81. 34. Jie KS, Bots ML, Vermeer C, et al. Vitamin K intake and osteocalcin levels in women with and without aortic atherosclerosis: a population-based study. Atherosclerosis. 1995;116:117-23. 35. Booth SL, Martini L, Peterson JW, Saltzman E, Dallal GE, Wood RJ. Dietary phylloquinone depletion and repletion repletion in older women. J Nutr. 2003 Aug;133(8):2565-9. 36. Feskanish D, Weber P, Willett WC, et al. Vitamin K intake and hip fractures in women: a prospective study. Am J Clin Nutr. 1999;69:74-9. 37. Levy RJ, Zenker JA, Lian JB. Vitamin K-dependent calcium binding proteins in aortic valve calcification. J Clin Invest. 1980 Feb;65(2):563-6. 38. Beulens JW, Bots ML, Atsma F, et al. High dietary menaquinone intake is associated with reduced coronary calcification. Atherosclerosis. 2009 Apr;203(2):489-93. 39. Vermeer C, Braam L. Role of K vitamins in the regulation of tissue calcification. J Bone Miner Metab. 2001;19:201-6. 40. Available at: http://www.massdevice.com/news/medtronic%E2%80%99s-corevalve-demonstrates-quality-life-improvements. Accessed June 14, 2011. 41. Available at: http://www.edwards.com/fr/newsroom/Pages/ShowPR.aspx?PageGuid=%7Bb9b307be-967a-4cdc-a3f7432b46e938d2%7D. Accessed June 14, 2011. 42. Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF. Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2. Arch Intern Med. 2006 Jan 23;166(2):241-6. 43. Available at: http://www.internalmedicinenews.com/news/cardiovascular-disease/single-article/partner-puts-tavr-in-reach-of-older-high-risk-patients/05849896b6.html. Accessed April 14, 2011. 44. Rapp AH, Hillis LD, Lange RA, Cigarroa JE. Prevalence of coronary artery disease in patients with aortic stenosis with and without angina pectoris. Am J Cardiol. 2001;87:1216–7. 45. Mohty D, Pibarot P, Després JP, et al. Association between plasma LDL particle size, valvular accumulation of oxidized LDL, and inflammation in patients with aortic stenosis. Arterioscler Thromb Vasc Biol. 2008 Jan;28(1):187-93. 46. Pohle K, Maffert R, Ropers D, et al. Progression of aortic valve calcification: association with coronary atherosclerosis and cardiovascular risk factors. Circulation. 2001 Oct 16;104(16):1927–32. 47. Novaro GM, Pearce GL, Sprecher DL, Griffin BP. Comparison of cardiovascular risk and lipid profiles in patients undergoing aortic valve surgery versus those undergoing coronary artery bypass grafting. J Heart Valve Dis. 2001 Jan;10(1):19–24. 48. Mohler ER, Sheridan MJ, Nichols R, Harvey WP, Waller BF. Development and progression of aortic valve stenosis: atherosclerosis risk factors—a causal relationship? A clinical morphologic study. Clin Cardiol. 1991 Dec;14(12):995–9. 49. Swierszcz J, Dubiel JS, Milewicz T, Sztefko K, Krzysiek J. Smoking, increase in plasma lipoprotein (a) and triglycerides, as well as decrease in plasma HDL-cholesterol concentrations seem to be linked with aortic valve stenosis and its progression. Przegl Lek. 2009;66(4):159-65. 50. Chui MC, Newby DE, Panarelli M, Bloomfield P, Boon NA. Association between calcific aortic stenosis and hypercholesterolemia: is there a need for a randomized controlled trial of cholesterol-lowering therapy? Clin Cardiol. 2001 Jan;24(1):52-5. 51. Palta S, Pai AM, Gill KS, Pai RG. New insights into the progression of aortic stenosis: implications for secondary prevention. Circulation. 2000 May 30;101(21):2497-502. 52. Boon A, Cheriex E, Lodder J, Kessels F. Cardiac valve calcification: characteristics of patients with calcification of the mitral annulus or aortic valve. Heart. 1997 Nov;78(5):472–4. 53. Yilmaz MB, Guray U, Guray Y, et al. Lipid profile of patients with aortic stenosis might be predictive of rate of progression. Am Heart J. 2004 May;147(5):915-8. 54. Galante A, Pietroiusti A, Vellini M, et al. C-reactive protein is increased in patients with degenerative aortic valvular stenosis. J Am Coll Cardiol. 2001 Oct;38(4):1078–82. 55. Hsu SY, Hung KC, Chang SH, Wen MS, Hsieh IC. C-reactive protein in predicting coronary artery disease in subjects with aortic valve sclerosis before diagnostic coronary angiography. Am J Med Sci. 2006 May;331(5):264–9. 56. Pate GE. Association between aortic stenosis and hypertension. J Heart Valve Dis. 2002 Sep;11(5):612-4. 57. Garcia D, Pibarot P, Kadem L, Durand LG. Respective impacts of aortic stenosis and systemic hypertension on left ventricular hypertrophy. J Biomech. 2007;40(5):972-80. 58. Antonini-Canterin F, Huang G, Cervesato E, et al. Symptomatic aortic stenosis: does systemic hypertension play an additional role? Hypertension. 2003 Jun;41(6):1268-72. 59. Lindroos M, Kupari M, Valvanne J, Strandberg T, Heikkila J, Tilvis R. Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J. 1994 Jul;15(7):865–70. 60. Ngo MV, Gottdiener JS, Fletcher RD, Fernicola DJ, Gersh BJ. Smoking and obesity are associated with the progression of aortic stenosis. Am J Geriatr Cardiol. 2001 Mar-Apr;10(2):86-90. 61. Owens DS, Katz R, Takasu J, Kronmal R, Budoff MJ, O’Brien KD. Incidence and progression of aortic valve calcium in the Multi-ethnic Study of Atherosclerosis (MESA). Am J Cardiol. 2010 Mar 1;105(5):701-8. 62. Kamalesh M, Ng C, El Masry H, Eckert G, Sawada S. Does diabetes accelerate progression of calcific aortic stenosis? Eur J Echocardiogr. 2009 Aug;10(6):723-5. 63. Katz R, Wong ND, Kronmal R, et al. Features of the metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the Multi-Ethnic Study of Atherosclerosis. Circulation. 2006 May 2;113(17):2113-9. 64. Deutscher S, Rockette HE, Krishnaswami V. Diabetes and hypercholesterolemia among patients with calcific aortic stenosis. J Chronic Dis. 1984;37(5):407–15. 65. Iwamoto J, Takeda T, Sato Y. Role of vitamin K2 in the treatment of postmenopausal osteoporosis. Curr Drug Saf. 2006 Jan;1(1):87-97. 66. Hansen LB, Vondracek SF. Prevention and treatment of nonpostmenopausal osteoporosis. Am J Health Syst Pharm. 2004 Dec 15;61(24):2637-54. 67. Ikeda Y, Iki M, Morita A, et al. Intake of fermented soybeans, natto, is associated with reduced bone loss in postmenopausal women: Japanese Population-Based Osteoporosis (JPOS) Study. J Nutr. 2006 May;136(5):1323-8. 68. Kanai T, Takagi T, Masuhiro K, Nakamura M, Iwata M, Saji F. Serum vitamin K level and bone mineral density in post-menopausal women. Int J Gynaecol Obstet. 1997 Jan;56(1):25-30. 69. Miki T, Nakatsuka K, Naka H, et al. Vitamin K(2) (menaquinone 4) reduces serum undercarboxylated osteocalcin level as early as 2 weeks in elderly women with established osteoporosis. J Bone Miner Metab. 2003;21(3):161-5. 70. Skolnick AH, Osranek M, Formica P, Kronzon I. Osteoporosis treatment and progression of aortic stenosis. Am J Cardiol. 2009 Jul 1;104(1):122-4. 71. Sterbakova G, Vyskocil V, Linhartova K. Bisphosphonates in calcific aortic stenosis: association with slower progression in mild disease--a pilot retrospective study. Cardiology. 2010;117(3):184-9. 72. Roberts WC, Waller BF. Effect of chronic hypercalcemia on the heart. Am J Med. 1981;71:371–84. 73 Akat K, Kaden JJ, Schmitz F, et al. Calcium metabolism in adults with severe aortic valve stenosis and preserved renal function. Am J Cardiol. 2010 Mar 15;105(6):862-4. 74. Iribarren C, Sidney S, Sternfeld B, Browner WS. Calcification of the aortic arch: risk factors and association with coronary heart disease, stroke, and peripheral vascular disease. JAMA. 2000 Jun 7;283(21):2810-5. 75. Maher ER, Young G, Smyth-Walsh B, Pugh S, Curtis JR. Aortic and mitral valve calcification in patients with end-stage renal disease. Lancet. 1987 Oct 17;2(8564):875-7. 76. Urena P, Malergue MC, Goldfarb B, Prieur P, Guedon-Rapoud C, Petrover M. Evolutive aortic stenosis in hemodialysis patients: analysis of risk factors. Nephrologie.1999;20(4):217-25. 77. Perkovic V, Hunt D, Griffin SV, du Plessis M, Becker GJ. Accelerated progression of calcific aortic stenosis in dialysis patients. Nephron Clin Pract. 2003;94(2):c40-5. 78. Available at: http://www.parathyroid.com/parathyroid-function.htm. Accessed Apr 20, 2011. 79. Tsukamoto Y. Studies on action of menaquinone-7 in regulation of bone meta-bolism and its preventive role of osteoporosis. Biofactors. 2004;22(1-4):5-19. 80. Kobayashi M, Hara K, Akiyama Y. Effects of vitamin K2 (menatetrenone) on calcium balance in ovariectomized rats. Jpn J Pharmacol. 2002 Jan;88(1):55-61. 81. Yamaguchi M, Ma ZJ. Inhibitory effect of menaquinone-7 (vitamin K2) on osteoclast-like cell formation and osteoclastic bone resorption in rat one tissues in vitro. Mol Cell Biochem. 2001 Dec;228(1-2):39-47. 82. Mirzaie M, Meyer T, Schwarz P, Lotfi S, Rastan A, Schondube F. Ultrastructural alterations in acquired aortic and mitral valve disease as revealed by scanning and transmission electron microscopical investigations. Ann Thorac Cardiovasc Surg. 2002 Feb;8(1):24-30. 83. Novaro GM, Griffin BP. Calcific aortic stenosis: another face of atherosclerosis? Cleve Clin J Med. 2003 May;70(5):471-7. 84. Sainani GS, Sainani R. Homocysteine and its role in the pathogenesis of atherosclerotic vascular disease. J Assoc Physicians India. 2002 May;50 Suppl:16-23. 85. Gunduz H, Arinc H, Tamer A, Akdemir R, Ozhan H, Binak E, Uyan C.The relation between homocysteine and calcific aortic valve stenosis. Cardiology. 2005;103(4):207-11. 86. Khorram O, Vu L, Yen SS. Activation of immune function by dehydroepiandrosterone (DHEA) in age-advanced men. J Gerontol A Biol Sci Med Sci. 1997 Jan;52(1):M1-7. 87. Zenk JL, Kuskowski MA. The use of 3-acetyl-7-oxo-dehydroepiandrosterone for augmenting immune response in the elderly. Presented at meeting of FASEB, April 17, 2004. 88. Liu YY, Yang N, Kong LN, Zuo PP. Effects of 7-oxo-DHEA treatment on the immunoreactivity of BALB/c mice subjected to chronic mild stress. Yao Xue Xue Bao. 2003 Dec;38(12):881-4. 89. Bauer ME. Stress, glucocorticoids and ageing of the immune system. Stress. 2005 Mar;8(1):69-83. 90. Watson RR, Huls A, Araghinikuam M, Chung S. Dehydroepiandrosterone and diseases of aging. Drugs Aging. 1996 Oct;9(4):274-91. 91. Gijsbers BL, Jie KS, Vermeer C. Effect of food composition on vitamin K absorption in human volunteers. Br J Nutr. 1996 Aug;76(2):223-9. 92. Schurgers LJ, Teunissen KJ, Hamulyák K, Knapen MH, Vik H, Vermeer C. Vitamin K-containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7. Blood. 2007;109(8):3279-83. 93. Available at: http://www.ars.usda.gov/sp2userfiles/place/12354500/articles/jafc54_463-467.pdf. Accessed June 15, 2011. 94. Available at: http://www.westonaprice.org/abcs-of-nutrition/175#foods. Accessed June 15, 2011 95. Tsukamoto Y, Ichise H, Kakuda H, Yamaguchi M. Intake of fermented soybean (natto) increases circulating vitamin K2 (menaquinone-7) and gamma-carboxylated osteocalcin concentration in normal individuals. J Bone Miner Metab. 2000;18(4):216-22. 96. Rees K, Guraewal S, Wong YL, et al. Is vitamin K consumption associated with cardio-metabolic disorders? A systematic review. Maturitas. 2010 Oct;67(2):121-8. 97. Faloon W. How to circumvent 17 independent heart attack risk factors. Life Extension Magazine®. 2009 May;15(5):54-81. | ||||||||||||||||||||||