Life Extension Magazine®
In a shocking exposé of the cancer establishment, Dr. Ralph Moss in his frequently updated book The Cancer Industry revealed the sordid history of radiation therapy. The first victims were researchers and physicians who succumbed to radiation's lethal effects without even suspecting it posed a danger to them. The next set of medical victims was patients who received severe burns from radiation overdoses that left them painfully mutilated or dead from acute radiation poisoning. As radiation doses were refined, the cancer establishment proclaimed a major treatment breakthrough. Yet the statistics were manipulated to cover up what was really happening to irradiated patients. For instance, patients with progression-free survival of 5 years (or less) are often listed as successes even if the same cancer later returns.1,2 Most disturbing are statistical methods that ignore lethal side effects such as radiation necrosis in the brain that kills the majority of its victims, but are not always officially tabulated as cancer deaths.3,4 This enables statisticians to say the radiation "cured" the patient of cancer, while omitting the fact that the therapy itself killed the patient. Radiation therapy is an important part of treating certain head and neck tumors and is often used after surgery.5 But lethal radiation necrosis to the brain is one potential side effect.6 Radiation therapy is routinely used to treat primary brain tumors. The cure rate for the most common brain tumors is disturbingly low,7 but even in those fortunate enough to have their brain tumors destroyed by the radiation, a large percentage succumb shortly thereafter to radiation necrosis of the brain.8 The more prevalent and omitted cover-up relates to the long-term impact of radiation therapy. For example, another danger of radiation therapy to the head is increased risk of stroke.9 A study of head and neck cancer patients who received radiation therapy found that stroke rates were five times greater than expected.10 This elevated stroke risk was found many years after administration of radiation. The average time between radiation treatment and stroke was 10.9 years, but the increased risk of stroke persisted for 15 years after radiation therapy. For cancer patients treated with radiation therapy that later die from a stroke, the official cause of death is stroke, even though the radiation therapy often caused the stroke. This is an example of how cancer cure statistics are misleading. The government contends that radiation therapy is curing cancer patients, yet long-term radiation side effects cause many deaths that are not attributed to cancer.
The government claims that more cancer victims are living beyond five years, but ignores the fact that the toxic therapies used to eradicate cancer can themselves cause premature death.11 High-dose radiation to the chest cavity increases heart disease risk… and this side effect may not occur for 20 years or later.12 Some of the side effects from radiation therapy to the breast include a breakdown of the skin or such severe pain in the breast that surgery is needed for treatment.13 Radiation therapy given to the axillary lymph nodes can increase the risk of patients developing arm swelling ("lymphedema") following axillary (armpit) dissection.14-17 Radiation to this area can cause numbness, tingling, or even pain and loss of strength in the hand and arm years after treatment.14,16 Some patients develop "radiation pneumonitis," a lung reaction that causes a cough, shortness of breath, and fevers three to nine months after completing treatment.16 These side effects may go away within a relatively short time or persist over an extended period. The primary concern with radiation therapy is that it may initiate secondary cancers years or decades after the primary cancer was "cured." This does not means that all cancer patients should refuse radiation therapy, as it often adds years or decades to their lives, and is in many cases curative. But as Ralph Moss, PhD, graphically described in his Cancer Industry books, oncology researchers are motivated to achieve complete responses that they can later claim to be cancer "cures." Overlooked from the statistics are horrific long-term side effects that leave patients permanently mutilated, in constant pain with loss of bodily functions, and under chronic medical care to deal with the damage inflicted by the "cancer cure." Patients suffering side effects from conventional treatments are often never the same again, yet the cancer establishment uses these cases to create statistical models to pretend their toxic therapies are a panacea. In Suzanne Somers' case, she has long regretted her submission to radiation therapy after her lumpectomy. While she made the right choice in saying "no" to chemotherapy, she has suffered for ten years from the destructive effects caused by the intense amount of radiation delivered to her breast and surrounding tissues. How Radiation Causes Long-term Damage to Breast TissuesRadiation therapy has long been used to treat breast cancer. For patients who choose breast-conserving surgery, have multiple positive lymph nodes, or have a local recurrence, radiation therapy will likely be part of the treatment plan.
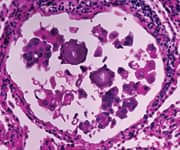
Radiation acts directly on the cell nucleus. Cancer cells grow rapidly compared to normal cells, so by radiating the cancerous area, cancer cells are damaged and many of them destroyed. Unfortunately, radiation also has a negative effect on normal cells. By mutating genes in the nucleus of healthy cells, these normal cells are more likely to later develop into cancer. This damage to genes in the cells' nucleus also causes the expression of pro-inflammatory factors that result in a constant bombardment (inflammatory fires) by one's immune cytokines against the irradiated cells. As the cells initially damaged by radiation are destroyed, the "inflammatory fires" spread to nearby healthy cells and create a chain reaction whereby more healthy cells come under chronic cytokine-inflammatory attack. Radiation damages the blood supply to normal skin at a microscopic level. This results in a significantly greater risk of complications following surgery. These risks include infection, delayed healing, wound breakdown, and fat necrosis, as well as implant-related problems.18 Radiation therapy can be the source of serious problems when it comes to breast reconstruction. This Explains Why Suzanne Somers Stated:
Important SummaryThis article is not meant to dissuade cancer patients from utilizing radiation therapy, as when properly used against specific tumors it can produce significantly higher cure rates that offset the risk of side effects. For instance, if you are diagnosed with Hodgkin lymphoma in the chest cavity, radiation has a high probability of curing you. Even though your risk of heart disease increases because of the radiation, it can buy you decades of additional life and you can take assertive steps to reduce your odds of suffering a heart attack knowing that you are at increased risk.12,19-21 Same for stroke risk in those who receive radiation to the head. Aggressive stroke prevention may enable you to avoid the five-fold increase in stroke risk caused by the radiation.10,22,23
For women with breast cancer, there are established criteria for determining if radiation therapy is likely to provide a benefit that offsets the side effect risks. A careful analysis of one's individual breast cancer that include primary tumor molecular profiling, tumor size, lymph node involvement, presence of circulating tumor cells, whole-body PET scans and CT scans, and many other diagnostics are critical to determining if radiation therapy is an appropriate choice. Life Extension® published an extensive Cancer Radiation Protocol long ago that provides validated methods of improving the ability of radiation to eradicate cancer cells, while sparing healthy cells from radiation's many potential side effects. Access the most recent version of the Cancer Radiation Protocol. If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027. | |||||
| Reference | |||||
|