Life Extension Magazine®
Failure to understand the basic cause of a disease can negate the effects of well-meaning prevention strategies. At any given time, popular myths surround the real causes of human disorders. While you may have heard all kinds of reasons why increasing numbers of people are contracting cancer, the underlying cause (that few doctors address) is the aging process itself.1 One reason this fundamental cause has been neglected is that up until recently, there was little one could do to protect against this proven risk factor. In this article, we are going to explain how aging increases cancer risk and what you can do to protect against this pathological phenomenon. To enable you to fully understand the carcinogenic effects of aging, we have reprinted on this page a chart showing women’s breast cancer risk by age. A quick look at this chart clearly documents that aging is the underlying cause of breast cancer. Next we are going to tell you why and what you can do to protect yourself.
Why Aging Cells Are So VulnerableAn article published in the New England Journal of Medicine titled “Roads Leading to Breast Cancer” provides a great one sentence explanation of why aging cells are vulnerable to cancer. Here is that sentence: “Cancer results from the accumulation of mutations in genes that regulate cellular proliferation.”3 In this one sentence, you have just learned why people contract more cancer as they grow older. To clarify this further, please understand that every time a cell divides, slight mutations occur to the genes that regulate cellular proliferation. Furthermore, mutations to genes happen in response to direct insult from ionizing radiation. The longer you live, the more gene mutations you encounter. Once too many regulatory genes become mutated, cells lose normal regulatory control and can turn into cancer cells. So a basic prevention strategy is to do something about the gene mutations in your cells that make you more vulnerable to contracting cancer with each passing day. The encouraging news is that this is now possible with a very simple approach. Restoring Healthy Gene Function
In recent years, a multitude of studies have shown cancer risk reductions of 50% and greater based on higher vitamin D status.4-9 People with higher vitamin D levels have sharply lower risks of cancers of the breast, prostate, colon, esophagus, pancreas, ovary, rectum, bladder, kidney, lung and uterus, along with non-Hodgkin’s lymphoma and multiple myeloma.4,10-22 What has fascinated us most, however, is that vitamin D protects against cancer by enabling people to regain control over the genes that regulate cell proliferation. Vitamin D has an effect on at least 200 human genes.22 Many of these genes are responsible for regulating not only cell proliferation, but differentiation and apoptosis as well. Here are simple definitions of these cellular processes: Proliferation: Uncontrolled cell division (cancer cells are characterized by rapid and uncontrolled division). Differentiation: Process that cells undergo to mature into normal cells (uncontrolled reproduction of immature cells is a defining feature of cancer). Apoptosis: Natural termination of defective cells (cancer cells are resistant to natural destruction, making them difficult to eradicate). With less than optimal vitamin D status, the expression of the genes that regulate the three critical processes above becomes defective. This means these regulatory genes can no longer maintain healthy cellular function (including programmed termination). The result is sharply higher cancer risks, as the lack of vitamin D negatively impacts gene expression that controls proliferation, differentiation, and apoptosis of our cells. So for only pennies a day, we can all achieve optimal vitamin D status and help our cells regain control over genes that protect us against cancer. For the first time, humans can exert a significant degree of control over a lethal aging process, i.e. gene mutations that are the underlying cause of cancer itself! Breakthrough Study Documents Effectiveness of Vitamin DWhile numerous studies show people with higher blood levels of vitamin D have lowered cancer risk, what had been lacking was a doubleblind, placebo-controlled study that specifically measured the effects of higher-dose vitamin D supplementation (with calcium) on cancer incidence in humans. This is the kind of study that conventional medical doctors insist on seeing if they are to believe a nutrient (or drug) really provides a health benefit. In a breakthrough report, the effects of administering 1,000 IU a day of vitamin D (with calcium) was evaluated in 1,180 postmenopausal women living in the Midwest.10 After four years, the risk of contracting any cancer was 60% lower in the vitamin D (and calcium) group, compared with the placebo arm of the study. The scientists then performed an even more detailed analysis of the data. When excluding cancers diagnosed in the first year of the study, which would have included preexisting cancers present at the time participants began taking vitamin D, they found an astounding 77% reduction in cancer incidence in the group receiving vitamin D, compared with placebo. (Interestingly, in a third arm of this study in which the participants received calcium but no vitamin D, the cancer risk reductions were not as significant.) What this means is that if all Americans began taking just 1,000 IU of vitamin D each day (with calcium), as many as three-quarters of all cancers could be prevented in just four years. Not Good Enough!While a 60% to 77% reduction in cancer incidence in response to taking a moderate dose of vitamin D is impressive, it’s not good enough for us! It would be absurd to ignore the “other” documented factors that increase the incidence of cancer in aging people. We are going to talk a lot about specific breast cancer-prevention strategies in this article. Please keep in mind, however, that the same approaches that reduce breast cancer risk also lower rates of other common cancers, including cancer of the prostate gland.
Studies that look at human populations (epidemiological studies) have consistently shown that what we eat affects our cancer risk. Women who eat red meat suffer higher breast cancer rates, whereas men who eat red meat have greater prostate cancer rates.23,24 It’s not a coincidence. The same carcinogenic effects that red meat inflicts in breast cells occur in prostate and other cells in the body. In one of the better documented studies overseen by researchers at prestigious American universities, postmenopausal women in China who ate a Western-style diet (which included beef, pork, and desserts) were 60% more likely to develop breast cancer than those eating a diet based on vegetables and soy. Even more startling was the finding that in women who contracted estrogen receptor-positive breast tumors, those who ate the Western-style diet experienced a 90% increased risk!25 So what does this tell us when someone says that women should not take natural estrogen and progesterone because of fears of breast and other cancers? It tells us that we should not worry so much about natural hormone balancing, and should focus on the thousands of dangerous calories we are putting into our bodies each day.26 Don’t expect the government to warn you about the carcinogenic effects of common foods. Intense lobbying efforts by the food industry have resulted in the government perpetuating the myth that a “balanced diet” is healthy. The hard facts pulled from hundreds of published studies are that government-sanctioned Western diets are killing us in many ways, including sharply increasing incidences of breast, prostate, and other cancers. Consuming more plant-derived protein, phytonutrients, and omega-3 fatty acids in place of meat, high-fat dairy, and sugary foods is a good way to cut back on the foods that have been shown to increase breast cancer risk.25,27-29 (For specific information on why these bad foods are so dangerous, refer to the article titled “Eating Your Way to Prostate Cancer” in the February 2007 issue of Life Extension.)
How Cruciferous Vegetables Protect Against Breast CancerThere are certain fruits, vegetables and plant extracts that have been shown to protect against breast, prostate, and other cancers. Scientists have identified compounds in cruciferous vegetables (broccoli, cauliflower, Brussels sprouts, cabbage, kale) that specifically neutralize dangerous breakdown products of estrogen that promote cancer growth.30-35 Cruciferous vegetable compounds also help neutralize the many carcinogens we are inevitably exposed to each day.36,37 One of best studied cruciferous vegetable compounds is called indole-3-carbinol, or I3C for short. Women seeking to restore youthful hormone balance should make sure to obtain enough I3C from their diet or by taking standardized supplements. The reason for this is that I3C increases levels of a cancer- protective estrogen metabolite (2-hydroxyestrone, or 2-OHE1), while suppressing a dangerous estrogen metabolite (16 alpha-hydroxyestrone, or 16-OHE1) that promotes breast and other cancers.38,39 To emphasize the critical importance of I3C (and its related compounds), please understand that aging women still produce estrogen, and that the estrogen they supplement with can follow two primary metabolic pathways in the body. If we convert estrogen to 16 alphahydroxyestrone, then we increase the risk of breast and other cancers. If on the other hand, we convert estrogen to 2-hydroxyestrone, then we decrease our risk for breast and other cancers.40-42 I3C can readily be obtained by eating lots of cruciferous vegetables and/or taking the proper amount in supplement form. To confirm the theory that certain estrogen metabolites can contribute to cancer, researchers analyzed data gathered from over 10,000 Italian women over more than five years. The objective was to determine how dietary and hormonal factors influence breast cancer risk. They found that women were much less likely to develop breast cancer when they had higher levels of 2-hydroxyestrone.40 This same finding has been shown in additional studies of different populations.43,44 The toxic estrogen metabolite 16 alpha-hydroxyestrone acts as a breast tumor promoter.45 By contrast, estrogen metabolized via the 2-hydroxyestrone pathway does not exhibit estrogenic activity in breast tissue. 45 Additionally, a form of this less active estrogen metabolite is believed to prevent the formation of blood vessels necessary to feed growing cancers, thus helping to arrest tumor growth.46 This delicate balance of estrogens is crucially important for men’s health as well. In a study that examined the ratio of estrogen metabolites relative to prostate cancer risk, elevated levels of 16 alpha-hydroxyestrone were linked with an increased risk of prostate cancer.41 Fortunately, the cruciferous vegetable compounds (such as I3C) are effective in shifting estrogen metabolism to the more beneficial pathway, thus reducing levels of toxic 16 alphahydroxyestrone and increasing levels of protective 2-hydroxyestrone.42,45,47,48 This beneficial modulation of estrogen with reduced risk of breast and other cancers, including cervical, prostate, and even head and neck cancers.33,40-42 Cruciferous vegetable compounds thus play an important role in fighting cancer. | ||||||||
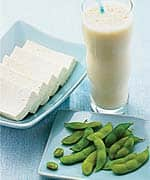
The Cancer Prevention Potential of SoyThe latest study showing a remarkable 90% reduction in estrogen receptor-positive breast cancers in women who consumed lots of vegetables and soy (in lieu of a Western-style diet) provides persuasive evidence that compounds found in soy indeed have a breast cancerpreventive effect.25 For the past decade, a controversy has raged over whether people can reduce their risk of cancer by increasing their consumption of soy foods or soy supplements. In response to the debate, a number of studies were initiated in the 1990s to ascertain soy’s effects on human health. Over the past few years, the results of these studies began to be released. While ignored by the mainstream media, the startling findings indicate that prostate and breast cancer risk could be cut in half if people only consumed more soy.25,49-51
Isoflavones derived from soy have shown great promise in providing natural protection against multipletypes of cancer.52-54 Isoflavones are phytochemical constituents of soy, with two of the best known being genistein and daidzein. The isoflavones are believed to exert a number of positive biological effects on the human body, and many practitioners of integrative medicine (and even a small but growing number in mainstream medicine) now believe that consumption of soy and isoflavones can reduce the risk of many chronic diseases, including cancer, heart disease, and osteoporosis.49-59 Studies conducted in Asia found that Asian women, who consume many more isoflavones than American women, have significantly lower risks of developing breast cancer.60 Because animal studieshave shown that a diet high in soyand genistein can protect againstmammary, colon, and skin tumors,61it seemed reasonable to think thatsoy could also help prevent humancancers and, in particular, breastcancer. Yet many mainstream medical practitioners remain skepticalthat something as “simple” as soycould have such a profound effect onhuman health.
Soy, Estrogen, and Breast CancerSome in the medical establishment believe that soy isoflavones have no role in preventing serious diseases such as cancer. Others believe that soy isoflavones should not be used as nutritional supplements because isoflavones act as natural estrogens and could cause many of the same problems—such as increased risk of stroke—that synthetic estrogens are now known to cause. In fact, soy isoflavones do not simply act as “natural” estrogens. Soy isoflavones are correctly classified as selective estrogen receptor modulators. Due to their unique molecular structure, soy isoflavones can act as either estrogen receptor agonists or receptor blockers. With this ability, soy isoflavones are thought by many to confer the beneficial effects of estrogen without its potentially dangerous side effects, especially in hormonally sensitive tissues found in both the breast and endometrium.62 Numerous studies show the potential benefits to women of incorporating soy in their diets to help prevent breast cancer. A landmark 1991 casecontrol study of women in Singapore, involving 200 case subjects and 420 control subjects, found that women with the highest consumption of soy-based products had a markedly decreased risk of developing breast cancer.63 An even larger Japanese case-control study in 1995, involving 1,186 subjects and 23,163 controls, also showed that women with increased tofu (soybean curd) intake had a significantly decreased risk of developing breast cancer compared with women who consumed small amounts of soy-based products such as tofu.51 Finally, a very large population-based, prospective study of 21,852 Japanese women aged 40-59 found that women with the highest intake of soy isoflavones reduced their risk of breast cancer by up to 54% compared with women with the lowest intake of soy isoflavones.60 Despite the evidence-based research showing soy isoflavones’ preventive effects on breast cancer, along with epidemiological studies highlighting the much lower rates of breast cancer among Asian women who consume significant amounts of soy-based products, some doctors still caution women against using soy-based foods and supplements.They contend that because soy isoflavones have been labeled as estrogen “mimics,” they could potentially worsen or even cause breast cancer. With the current knowledge that soy isoflavones act as selective estrogen receptor modulators and are not simply estrogen “mimics,” these arguments do not hold up. In addition to being a chemopreventive supplement for breast cancer, soy isoflavones are also thought to be effective in warding off other types of cancer that afflict women, including endometrial cancer. A recent casecontrol study reported the effects of soy isoflavones and other phytoestrogens on the risk of developing endometrial cancer.64 The study compared 500 women aged 35-79 who developed endometrial cancer between 1996 and 1999 with 470 age- and ethnicity-matched controls. As in studies examining the effects of isoflavones on breast cancer, this study showed that women with a higher intake of soy isoflavones had a significantly lower risk of developing endometrial cancer. Even more interesting was that the levels of isoflavones needed to provide protection against endometrial cancer were found to be much lower than the amount believed necessary to protect against breast cancer. Soy Counteracts Prostate Cancer in MenBoth animal and human studies have shown that soy isoflavones can help protect men from prostate cancer by slowing and even preventing the disease.65,66 Prostate cancer is the most common cancer in men and the second leading cause of death from cancer (after lung cancer) among men.67 As is the case concerning breast cancer in women, large epidemiological studies have shown that Asian men who consume large amounts of soy-based foods have a significantly lower incidence of prostate cancer, compared with their Western counterparts.68 Researchers found that soybean products, as well as other East Asian dietary staples such as fish and tofu, were associated with a decreased risk of prostate cancer in Japanese men.68 Specifically, men who consumed the greatest amounts of soybeans and tofu were 47% and 53% less likely, respectively, to develop prostate cancer than those who consumed the smallest amounts. Furthermore, in men who consumed the greatest product natto, the prostate cancer incidence was reduced by a remarkable 75%. Finally, in a case-control study published in January 2004, Japanese researchers sought to ascertain whether a high serum concentration of phytoestrogens reduces the risk of prostate cancer. The researchers collected lifestyle information and serum samples from more than 14,000 Japanese men in 1988-90, who were tracked until 1999. Phytoestrogens and sex hormones stored in serum were measured in 2002, and 52 case subjects and 151 controls were identified. This study clearly established that elevated serum levels of all three phytoestrogens assessed—genistein, daidzein, and equol—imparted a strong protective effect against prostate cancer.69 Men with the highest circulating levels of genistein, daidzein, and equol reduced their risk of prostate cancer by 62%, 59%, and 66%, respectively. Soy can be added to one’s diet in many ways, and it is increasingly being used in breast health dietary supplement formulas. Why Fruits are Important
The body is bombarded with carcinogens on a daily basis. These cancer-causing agents include pesticides, over-cooked food, alcohol, food additives, tobacco, fungal mutagens, and industrial pollutants. While avoiding carcinogens is difficult, it may be possible to mitigate their lethal effects by providing the body with a specific plant extract that facilitates the detoxification and removal of these dangerous substances from the body. A compound called D-glucarate is found in grapefruit, apples, oranges, broccoli, and Brussels sprouts.70,71 D-Glucarate has been shown to protect against cancer-causing agents by supporting detoxification and removal of dangerous chemicals, and also by protecting against the mutating effects that these carcinogens induce on cellular DNA.72 There are several mechanisms by which the body detoxifies itself. One way of guarding against toxic overload involves a pathway of detoxification in the body whereby carcinogens are combined with water-soluble substances, thus making them more easily removed from the body. This process is called glucuronidation, and D-glucarate has been shown to support this important detoxification mechanism.72 How Does D-Glucarate Work?D-Glucarate functions by inhibiting the dangerous beta-glucuronidase enzyme, thus protecting the critical “glucuronidation” detoxification mechanism. One example of the importance of glucuronidation can be seen in the risk factors for breast cancer. Excess levels of 16 alphahydroxyestrone and the beta-glucuronidase enzyme are associated with an increased incidence of breast cancer.73 D-Glucarate is thought to decrease estrogen levels by affecting estrogen’s elimination. Normally, estrogen is conjugated with glucurate in the liver (glucuronidation), and then excreted in the bile. A bacterial enzyme in the intestine called beta-glucuronidase can break the estrogen-glucuronide bond, allowing estrogen to be reabsorbed. D-Glucarate works at this step by inhibiting beta-glucuronidase.73 Blocking this enzyme is thought to decrease the amount of estrogen that is reabsorbed and thus to lower circulating estrogen levels.
Research studies have shown that D-glucarate inhibits mammary tumor incidence.74,75 One study in rats that already had breast cancer showed that oral D-glucarate administration resulted in a 50% inhibition of beta-glucuronidase, which led to a 30% reduction in mammary tumor growth during the promotion stage and a four-fold reduction in the absolute number of tumors.76 Another study showed a more than 70% decrease in mammary tumor development in rats exposed to carcinogens who were also administered D-glucarate.77 Still another study looked at the effects of D-glucarate on the initiation and promotional stages of mammary cancer. The results showed a reduction of 28% during the initiation stage, while cell replication was reduced by 42% during the promotion stage.78 Inhibition at the initiation stage is a very important part of D-glucarate’s actions, as it lessens the risk that cancer will even start. Eating lots of the right fruits and vegetables supplies the body with D-glucarate. It is also available in dietary supplements designed to support breast health. | |||||
How Lignans Protect the Breast and Prostate Glands
A number of published studies indicate that dietary lignans may protect against cancer by favorably altering estrogen metabolism, inhibiting angiogenesis, and inducing cancer cells to self destruct.79-81 The greatest support for a role of lignans in cancer prevention has been shown for premenopausal breast cancer. Researchers in New York assessed breast cancer risk and dietary lignan intake in more than 3,000 women, including about 1,100 patients with confirmed breast cancer and approximately 2,000 cancer-free women who served as controls. Using statistical analysis, the scientists determined that premenopausal women with the highest lignan intake had a 44% reduced risk of developing breast cancer.80 Scientists in Italy reported similar findings. Their research indicates that higher blood levels of enterolactone— the primary lignan derived by the body from flaxseed—are associated with a lower risk of breast cancer. Conversely, the researchers noted, “values of serum enterolactone were significantly lower in women who subsequently developed breast cancer,” leading them to conclude that the phytoestrogen enterolactone “had a strong protective effect on breast cancer risk.”81 Lignans may also protect against endometrial cancer, a condition associated with prolonged exposure to unopposed estrogens. Flax lignans may offer protection through an anti-estrogenic effect in the body. Researchers in California assessed lignan intake and cancer status among nearly 1,000 women in the San Francisco area and determined that women with the highest dietary lignan intake experienced the lowest risk of developing this carcinoma of the uterine lining. The relationship between lignans and endometrial cancer risk reduction was slightly stronger among postmenopausal women. Based on a lot of favorable publicity, health-conscious people are increasingly adding flax seed to their diet for the purpose of obtaining the beneficial lignans. Highly concentrated lignan extracts are also appearing in supplements to support breast and prostate health. Adding Up the NumbersAccording to the scientific data discussed in this article, significant reductions (up to 90%) in breast cancer risk have been found based on the types of foods and supplements one consumes.25 Even further risk reductions occur in conjunction with lowered overall calorie intake. In fact, for each excess calorie we ingest (and most of us ingest plenty of excess calories), our risk for many types of cancer increases.26,82,83 In adding up these numbers, it becomes clear that there are many steps one can take to sharply reduce the risk of breast, prostate, and other cancers. An evaluation of how certain plant extracts favorably affect estrogen metabolism indicates that aging humans may be able to safely benefit from natural hormone balancing. Is Fear of Cancer a Reason to Be Deprived of Hormones?As women enter the menopausal years, they face a difficult decision. The body’s natural production of estrogen, progesterone, DHEA, and other critical hormones needed to maintain health and vigor rapidly declines.84 While individual effects of menopause vary widely, most women suffer because their glands no longer produce the hormones needed to regulate critical physiological processes. Depression, irritability, and short-term memory lapses are common menopausal complaints, along with hot flashes, night sweats, and insomnia.85 Aging men suffer a host of disorders that range from unpleasant to lethal in response to testosterone deficiency and estrogen overload.86-92 Concern about cancer is the primary reason why men and women do not restore their hormones to more youthful levels. Like much of what we eat, estrogen and testosterone affect cell proliferation. Does that mean we should shrivel up, degenerate, and die from these sex hormone deficiencies we all face as a part of “normal” aging? Based on the enormity of the data showing how people can sharply reduce their rate of cancer and favorably affect estrogen metabolism in a way that points to cancer prevention, it is difficult to buy into the argument that natural sex hormones should only be enjoyed by the young. Large human population studies show huge reductions in cancer risk, along with specific protective mechanisms against estrogen’s negative pathways, when vitamin D, cruciferous vegetables (I3C), soy, D-glucarate, and lignans are consumed. Dramatic cancer rate reductions also occur when red meat, high-fat dairy, and other deleterious foods are reduced or eliminated from the diet. Misconceptions generated by conflicting studies and media hype have created an environment in which aging people suffer the agonies and shortened life spans caused by sex hormone imbalances, yet do nothing to correct this due to fear of cancer. When one looks at what the real risk factors are, it would appear that altering one’s lifestyle at any age would result in significant cancer reductions, even in those who properly restore their hormone balance to reflect a more youthful range. Remember the chart at the beginning of this article showing how breast cancer rates skyrocket as we age. During the younger years, when breast cancer is virtually non-existent, we enjoy high levels of youthful sex hormones (estrogen, progesterone, DHEA, and testosterone). As hormone levels decline with age, breast and prostate cancer risks increase. We now know this happens because of the “accumulation of mutations in our genes that regulate cellular proliferation.” 2 The incredible news is that there are low-cost nutrients that are proven to favorably restore healthy gene function and reduce our risk of cancer in the process. Just think, we have been told all our lives that there is nothing we can do about the genes we inherit from our parents that predispose us to certain diseases. Yet breakthrough research findings indicate that we can influence our genes to behave in a way that significantly reduces our risk of contracting common cancers. Additional scientific findings show how we can influence estrogen metabolism in our bodies so that it is protective against breast and other cancers. Based on the enormity of this data, it would appear that aging humans can restore many of the hormones they need to sustain life—without encountering adverse effects. If you have any questions on the scientific content of this article, please call a Life Extension Wellness Specialist at 1-800-226-2370. |
|
| References | |
|
1. Irminger-Finger I. Science of cancer and aging. J Clin Oncol. 2007 May 10;25(14):1844-51. 2. Simone CB. Cancer and Nutrition. Lawrenceville, NJ: Princeton Institute; 2005. 3. Haber D. Roads leading to breast cancer. N Engl J Med. 2000 Nov 23;343(21):1566-8. 4. Garland CF, Comstock GW, Garland FC, et al. Serum 25-hydroxyvitamin D and colon cancer: eight-year prospective study. Lancet. 1989 Nov 18;2(8673):1176-8. 5. Garland CF, Garland FC, Gorham ED. Can colon cancer incidence and death rates be reduced with calcium and vitamin D? Am J Clin Nutr. 1991 Jul;54(1 Suppl):193S-201S. 6. Garland CF, Gorham ED, Mohr SB, et al. Vitamin D and prevention of breast cancer: pooled analysis. J Steroid Biochem Mol Biol. 2007 Mar;103(3-5):708-11. 7. Gorham ED, Garland CF, Garland FC, et al. Vitamin D and prevention of colorectal cancer. J Steroid Biochem Mol Biol. 2005 Oct;97(1-2):179-94. 8. John EM, Schwartz GG, Koo J, Van Den BD, Ingles SA. Sun exposure, vitamin D receptor gene polymorphisms, and risk of advanced prostate cancer. Cancer Res. 2005 Jun 15;65(12):5470-9. 9. Garland CF, Garland FC, Gorham ED, et al. The role of vitamin D in cancer prevention. Am J Public Health. 2006 Feb;96(2):252-61. 10. Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007 Jun;85(6):1586-91. 11. Friedrich M, Rafi L, Mitschele T, et al. Analysis of the vitamin D system in cervical carcinomas, breast cancer and ovarian cancer. Recent Results Cancer Res. 2003;164:239-46. 12. de Lyra EC, da S, I, Katayama ML, et al. 25(OH)D3 and 1,25(OH)2D3 serum concentration and breast tissue expression of 1alpha-hydroxylase, 24-hydroxylase and Vitamin D receptor in women with and without breast cancer. J Steroid Biochem Mol Biol. 2006 Aug;100(4-5):184-92. 13. Holick MF. Vitamin D: its role in cancer prevention and treatment. Prog Biophys Mol Biol. 2006 Sep;92(1):49-59. 14. Skinner HG, Michaud DS, Giovannucci E, et al. Vitamin D intake and the risk for pancreatic cancer in two cohort studies. Cancer Epidemiol Biomarkers Prev. 2006 Sep;15(9):1688-95. 15. Zhang X, Nicosia SV, Bai W. Vitamin D receptor is a novel drug target for ovarian cancer treatment. Curr Cancer Drug Targets. 2006 May;6(3):229-44. 16. Konety BR, Lavelle JP, Pirtskalaishvili G, et al. Effects of vitamin D (calcitriol) on transitional cell carcinoma of the bladder in vitro and in vivo. J Urol. 2001 Jan;165(1):253-8. 17. Grant WB, Holick MF. Benefits and requirements of vitamin D for optimal health: a review. Altern Med Rev. 2005 Jun;10(2):94-111. 18. Mernitz H, Smith DE, Wood RJ, Russell RM, Wang XD. Inhibition of lung carcinogenesis by 1alpha,25-dihydroxyvitamin D3 and 9-cis retinoic acid in the A/J mouse model: evidence of retinoid mitigation of vitamin D toxicity. Int J Cancer. 2007 Apr 1;120(7):1402-9. 19. Becker S, Cordes T, Diesing D, Diedrich K, Friedrich M. Expression of 25 hydroxyvitamin D3-1alpha-hydroxylase in human endometrial tissue. J Steroid Biochem Mol Biol. 2007 Mar;103(3-5):771-5. 20. Polesel J, Talamini R, Montella M, et al. Linoleic acid, vitamin D and other nutrient intakes in the risk of non-Hodgkin lymphoma: an Italian case-control study. Ann Oncol. 2006 Apr;17(4):713-8. 21. Imseis RE, Palmieri GM, Holbert JM, Leventhal MR, Sebes JI. Effect of calcitriol and pamidronate in multiple myeloma. Am J Med Sci. 1999 Jul;318(1):61-6. 22. Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81. 23. Zhu G, Zhang YQ, Wan B. Role of dietary factors in prostate cancer development. Zhonghua Nan Ke Xue. 2005 May;11(5):375-8 24. Taylor EF, Burley VJ, Greenwood DC, Cade JE. Meat consumption and risk of breast cancer in the UK Women’s Cohort Study. Br J Cancer. 2007 Apr 10;96(7):1139-46. 25. Cui X, Dai Q, Tseng M et al. Dietary patterns and breast cancer risk in the shanghai breast cancer study. Cancer Epidemiol Biomarkers Prev. 2007 Jul;16(7):1443-8. 26. Silvera SA, Jain M, Howe GR, Miller AB, Rohan TE. Energy balance and breast cancer risk: a prospective cohort study. Breast Cancer Res Treat. 2006 May;97(1):97-106. 27. Tavani A, Giordano L, Gallus S, et al. Consumption of sweet foods and breast cancer risk in Italy. Ann Oncol. 2006 Feb;17(2):341-5. 28. Lajous M, Willett W, Lazcano-Ponce E, et al. Glycemic load, glycemic index, and the risk of breast cancer among Mexican women. Cancer Causes Control. 2005 Dec;16(10):1165-9. 29. Moorman PG, Terry PD. Consumption of dairy products and the risk of breast cancer: a review of the literature. Am J Clin Nutr. 2004 Jul;80(1):5-14. 30. Brennan P, Hsu CC, Moullan N, et al. Effect of cruciferous vegetables on lung cancer in patients stratified by genetic status: a mendelian randomisation approach. Lancet. 2005 Oct 29;366(9496):1558-60. 31. Ambrosone CB, McCann SE, Freudenheim JL, et al. Breast cancer risk in premenopausal women is inversely associated with consumption of broccoli, a source of isothiocyanates, but is not modified by GST genotype. J Nutr. 2004 May;134(5):1134-8. 32. Kristal AR, Lampe JW. Brassica vegetables and prostate cancer risk: a review of the epidemiological evidence. Nutr Cancer. 2002;42(1):1-9. 33. Jin L, Qi M, Chen DZ, et al. Indole-3-carbinol prevents cervical cancer in human papilloma virus type 16 (HPV16) transgenic mice. Cancer Res. 1999 Aug 15;59(16):3991-7. 34. Zhang SM, Hunter DJ, Rosner BA, et al. Intakes of fruits, vegetables, and related nutrients and the risk of non-Hodgkin’s lymphoma among women. Cancer Epidemiol Biomarkers Prev. 2000 May;9(5):477-85. 35. Dalessandri KM, Firestone GL, Fitch MD, Bradlow HL, Bjeldanes LF. Pilot study: effect of 3,3’-diindolylmethane supplements on urinary hormone metabolites in postmenopausal women with a history of early-stage breast cancer. Nutr Cancer. 2004;50(2):161-7. 36. Fimognari C, Hrelia P. Sulforaphane as a promising molecule for fighting cancer. Mutat Res. 2007 May;635(2-3):90-104. 37. Conaway CC, Wang CX, Pittman B, et al. Phenethyl isothiocyanate and sulforaphane and their N-acetylcysteine conjugates inhibit malignant progression of lung adenomas induced by tobacco carcinogens in A/J mice. Cancer Res. 2005 Sep 15;65(18):8548-57. 38. Kall MA, Vang O, Clausen J. Effects of dietary broccoli on human drug metabolising activity. Cancer Lett. 1997 Mar 19;114(1-2):169-70. 39. Bradlow HL, Telang NT, Sepkovic DW, Osborne MP. 2-hydroxyestrone: the ‘good’ estrogen. J Endocrinol. 1996 Sep;150 SupplS259-65. 40. Muti P, Bradlow HL, Micheli A, et al. Estrogen metabolism and risk of breast cancer: a prospective study of the 2:16alpha-hydroxyestrone ratio in premenopausal and postmenopausal women. Epidemiology. 2000 Nov;11(6):635-40. 41. Muti P, Westerlind K, Wu T, et al. Urinary estrogen metabolites and prostate cancer: a case-control study in the United States. Cancer Causes Control. 2002 Dec;13(10):947-55. 42. Yoo HJ, Sepkovic DW, Bradlow HL, Yu GP, Sirilian HV, Schantz SP. Estrogen metabolism as a risk factor for head and neck cancer. Otolaryngol Head Neck Surg. 2001 Mar;124(3):241-7. 43. Kabat GC, Chang CJ, Sparano JA, et al. Urinary estrogen metabolites and breast cancer: a case-control study. Cancer Epidemiol Biomarkers Prev. 1997 Jul;6(7):505-9. 44. Kabat GC, O’Leary ES, Gammon MD, et al. Estrogen metabolism and breast cancer. Epidemiology. 2006 Jan;17(1):80-8. 45. Fowke JH, Longcope C, Hebert JR. Brassica vegetable consumption shifts estrogen metabolism in healthy postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2000 Aug;9(8):773-9. 46. Fowke JH, Qi D, Bradlow HL, et al. Urinary estrogen metabolites and breast cancer: differential pattern of risk found with pre- versus post-treatment collection. Steroids. 2003 Jan;68(1):65-72. 47. Michnovicz JJ, Adlercreutz H, Bradlow HL. Changes in levels of urinary estrogen metabolites after oral indole-3-carbinol treatment in humans. J Natl Cancer Inst. 1997 May 21;89(10):718-23. 48. Wong GY, Bradlow L, Sepkovic D, et al. Dose-ranging study of indole-3-carbinol for breast cancer prevention. J Cell Biochem Suppl. 1997;28-29:111-6. 49. Hirose K, Tajima K, Hamajima N, et al. A large-scale, hospital-based case-control study of risk factors of breast cancer according to menopausal status. Jpn J Cancer Res. 1995 Feb;86(2):146-54. 50. Jacobsen BK, Knutsen SF, Fraser GE. Does high soy milk intake reduce prostate cancer incidence? The Adventist Health Study (United States). Cancer Causes Control. 1998 Dec;9(6):553-7. 51. Kurahashi N, Iwasaki M, Sasazuki S, et al. Soy product and isoflavone consumption in relation to prostate cancer in Japanese men. Cancer Epidemiol Biomarkers Prev. 2007 Mar;16(3):538-45. 52. Messina MJ. Legumes and soybeans: overview of their nutritional profiles and health effects. Am J Clin Nutr. 1999 Sep;70(3 Suppl):439S-50S. 53. Yamamoto S, Sobue T, Kobayashi M, Sasaki S, Tsugane S. Soy, isoflavones, and breast cancer risk in Japan. J Natl Cancer Inst. 2003 Jun 18;95(12):906-913. 54. Lee MM, Gomez SL, Chang JS, et al. Soy and isoflavone consumption in relation to prostate cancer risk in China. Cancer Epidemiol Biomarkers Prev. 2003 Jul;12(7):665-8. 55. Schabath MB, Hernandez LM, Wu X, Pillow PC, Spitz MR. Dietary phytoestrogens and lung cancer risk. JAMA. 2005 Sep 28;294(12):1493-504. 56. Nothlings U, Murphy SP, Wilkens LR, Henderson BE, Kolonel LN. Flavonols and Pancreatic Cancer Risk: The Multiethnic Cohort Study. Am J Epidemiol. 2007 Aug 9. 57. Xu HS, Dai SL, Sun RY. Cardiovascular effects of phytoestrogens. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2005 Apr;27(2):258-61. 58. de Kleijn MJ, van der Schouw YT, Wilson PW, Grobbee DE, Jacques PF. Dietary intake of phytoestrogens is associated with a favorable metabolic cardiovascular risk profile in postmenopausal U.S.women: the Framingham study. J Nutr. 2002 Feb;132(2):276-82. 59. Roudsari AH, Tahbaz F, Hossein-Nezhad A, et al. Assessment of soy phytoestrogens’ effects on bone turnover indicators in menopausal women with osteopenia in Iran: a before and after clinical trial. Nutr J. 2005;430. 60. Yamamoto S, Sobue T, Kobayashi M, Sasaki S, Tsugane S. Soy, isoflavones, and breast cancer risk in Japan. J Natl Cancer Inst. 2003 Jun 18;95(12):906-13. 61. Barnes S. Effect of genistein on in vitro and in vivo models of cancer. J Nutr. 1995 Mar;125(3 Suppl):777S-83S. 62. Setchell KD. Soy isoflavones—benefits and risks from nature’s selective estrogen receptor modulators (SERMs). J Am Coll Nutr. 2001 Oct;20(5 Suppl):354S-62S; discussion 381S-383S. 63. Lee HP, Gourley L, Duffy SW, et al. Dietary effects on breast-cancer risk in Singapore. Lancet. 1991 May 18;337(8751):1197-200. 64. Horn-Ross PL, John EM, Canchola AJ, Stewart SL, Lee MM. Phytoestrogen intake and endometrial cancer risk. J Natl Cancer Inst. 2003 Aug 6;95(15):1158-64. 65. Schroder FH, Roobol MJ, Boeve ER, et al. Randomized, double-blind, placebo-controlled crossover study in men with prostate cancer and rising PSA: effectiveness of a dietary supplement. Eur Urol. 2005 Dec;48(6):922-30. 66. Nagata Y, Sonoda T, Mori M, et al. Fujimoto Dietary isoflavones may protect against prostate cancer in Japanese men. J Nutr. 2007 Aug;137(8):1974-9. 67. Available at: http://www.cdc.gov/omhd/Highlights/2007/HJune07.htm#2. Accessed August 10. 2007. 68. Sonoda T, Nagata Y, Mori M, et al. A case-control study of diet and prostate cancer in Japan: possible protective effect of traditional Japanese diet. Cancer Sci. 2004 Mar;95(3):238-42. 69. Ozasa K, Nakao M, Watanabe Y, et al. Serum phytoestrogens and prostate cancer risk in a nested case-control study among Japanese men. Cancer Sci. 2004 Jan;95(1):65-71. 70. Available at: http://www.garfield.library.upenn.edu/histcomp/kritchevsky-d_auth-citing/node/7082.html. Accessed August 20, 2007. 71. Dwivedi C, Heck WJ, Downie AA, Larroya S, Webb TE. Effect of calcium glucarate on beta-glucuronidase activity and glucarate content of certain vegetables and fruits. Biochem Med Metab Biol. 1990 Apr;43(2):83-92. 72. Walaszek Z, Szemraj J, Narog M et al. Metabolism, uptake, and excretion of a D-glucaric acid salt and its potential use in cancer prevention. Cancer Detect Prev. 1997;21(2):178-90. 73. No authors listed. Calcium-D-glucarate. Altern Med Rev. 2002 Aug;7(4):336-9. 74. Walaszek Z, Hanausek M, Sherman U, Adams AK. Antiproliferative effect of dietary glucarate on the Sprague-Dawley rat mammary gland. Cancer Lett. 1990 Jan;49(1):51-7. 75. Heerdt AS, Young CW, Borgen PI. Calcium glucarate as a chemopreventive agent in breast cancer. Isr J Med Sci. 1995 Feb;31(2-3):101-5. 76. Slaga TJ, Quilici-Timmcke J. D-Glucarate: A Nutrient Against Cancer. Columbus, Ohio: McGraw-Hill; 1999. 77. Walaszek Z, Hanausek-Walaszek M, Minton JP, Webb TE. Dietary glucarate as anti-promoter of 7,12-dimethylbenz[a]anthracene-induced mammary tumorigenesis. Carcinogenesis. 1986 Sep;7(9):1463-6. 78. Abou-Issa H, Moeschberger M, el-Masry W, et al. Relative efficacy of glucarate on the initiation and promotion phases of rat mammary carcinogenesis. Anticancer Res. 1995 May;15(3):805-10. 79. Magnúsdóttir EV. Phytoestrogens and human health. Laeknabladid. 2002 Nov;88(11):821-5. 80. McCann SE, Muti P, Vito D, et al. Dietary lignan intakes and risk of pre- and postmenopausal breast cancer. Int J Cancer. 2004 Sep 1;111(3):440-3. 81. Boccardo F, Lunardi G, Guglielmini P, et al. Serum enterolactone levels and the risk of breast cancer in women with palpable cysts. Eur J Cancer. 2004 Jan;40(1):84-9. 82. Slattery ML, Potter J, Caan B, et al. Energy balance and colon cancer--beyond physical activity. Cancer Res. 1997 Jan 1;57(1):75-80. 83. Michels KB. The role of nutrition in cancer development and prevention. Int J Cancer. 2005 Mar 20;114(2):163-5. 84. Freeman EW, Sammel MD, Lin H, et al. Symptoms associated with menopausal transition and reproductive hormones in midlife women. Obstet Gynecol. 2007 Aug;110(2 Pt 1):230-40. 85. Von Bamberger CM. Prevention and anti-aging in endocrinology. MMW Fortschr Med. 2007 Mar 1;149(9):33-5. 86. Izumi S, Tsubahara A. Improvement of peripheral neuropathy by testosterone in a patient with 48,XXYY syndrome. Tokai J Exp Clin Med. 2000 Jun;25(2):39-44. 87. Phillips GB, Pinkernell BH, Jing TY. The association of hypotestosteronemia with coronary artery disease in men. Arterioscler Thromb. 1994 May;14(5):701-6. 88. Hak AE, Witteman JC, de Jong FH, et al. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab. 2002 Aug;87(8):3632-9. 89. Pope HG, Jr., Cohane GH, Kanayama G, Siegel AJ, Hudson JI. Testosterone gel supplementation for men with refractory depression: a randomized, placebo-controlled trial. Am J Psychiatry. 2003 Jan;160(1):105-11. 90. Zumoff B. Hormonal abnormalities in obesity. Acta Med Scand Suppl. 1988;723:153-60. 91. Vermeulen A, Kaufman JM, Goemaere S, van Pottelberg I. Estradiol in elderly men. Aging Male. 2002 Jun;5(2):98-102. 92. Novák A, Brod M, Elbers J. Andropause and quality of life: findings from patient focus groups and clinical experts. Maturitas. 2002 Dec 10;43(4):231-7. 93. Bradlow HL, Sepkovic DW, Telang NT, Osborne MP. Indole-3-carbinol. A novel approach to breast cancer prevention. Ann N Y Acad Sci. 1995 Sep 30;768:180-200. 94. Zumoff B. Hormonal profiles in women with breast cancer. Obstet Gynecol Clin North Am. 1994 Dec;21(4):751-72. 95. Napoli N, Armamento-Villareal R. Estrogen hydroxylation in osteoporosis. Adv Clin Chem. 2007;43:211-27. 96. Bradlow HL, Telang NT, Sepkovic DW, Osborne MP. 2-hydroxyestrone: the ‘good’ estrogen. J Endocrinol. 1996 Sep;150 Suppl:S259-65.
|