Life Extension Magazine®
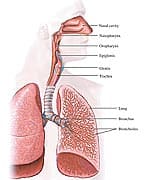
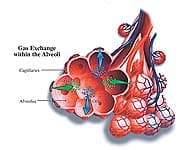
Potential Health Risks of Inhaled Insulin TherapyOther questions still remain unresolved about the potential health risks of inhaled insulin. Among the documented and possible health risks of insulin inhalation therapy are: 1. Increased risk of respiratory tract irritation, causing cough, shortness of breath, sore throat, and dry mouth.12 2. Development of hypoglycemia, with adverse outcomes in those who exercise immediately after inhalation and those who smoke. These effects may occur due to the rapid absorption of inhaled insulin from the alveoli.13-15 3. Exacerbation of existing conditions in asthmatics who require more inhaled insulin to control their blood sugar.16 Furthermore, inhaled insulin could lead to airway smooth muscle contraction, which could precipitate or exacerbate chronic obstructive pulmonary disease or episodes of asthma.17 4. Alveolar thickening, poor gas exchange, pulmonary hypertension, or pulmonary fibrosis. Additionally, inhaled insulin could cause adverse effects in people with pre-existing respiratory diseases such as chronic bronchitis, tuberculosis, tumors, and other chronic lung afflictions.18 5. Increase in insulin anti-bodies. In one study, inhaled insulin increased the level of insulin anti-bodies in the body from baseline levels of 6% to 35%.19 This could have the adverse effect of retarding the action of soluble insulin in the blood, since the removal of an insulin immune complex could make less insulin available to lower blood sugar. 6. Unknown long-term effects of supraphysiologic doses of insulin in the human lung or on neoplastic lung tissue. It is possible that insulin could stimulate unwanted tissue growth in normal and precancerous cells, which could lead to genetic defects and ultimately to cancer. 7. Potentially increased tumor incidence in the tissues of the respiratory tract, although no evidence of this has been presented to date. The true health risks could take a long time to come to light, as occurred with other drugs such as Vioxx® (an anti-inflammatory) and Avandia® (an oral anti-diabetic drug). In addition to the eye-opening health risks of inhaled insulin, it is more expensive than other insulin preparations. Should You Use Inhaled Insulin?I recommend that inhaled insulin should not be used in smokers or in patients with underlying lung diseases such as asthma or chronic obstructive pulmonary disease. Until the drug’s full health risks are known, I further discourage its use in those with precancerous lesions (such as polyps, dysplasia, or the leukoplakia that can accompany tobacco use). Inhaled insulin is not approved for use in pregnant women, children, or adolescents. I hope that the FDA and drug companies involved in licensing and developing an inhaled method of insulin delivery will fully investigate these health risks and concerns on a post-approval surveillance basis. The future of insulin delivery with the fewest side effects may come from development of slow-release injectable insulin lasting days to weeks with a single shot, or from implantation of insulin-producing stem cells. |
| References |
| 1. Heinemann L, Traut T, Heise T. Time-action profile of inhaled insulin. Diabet Med. 1997 Jan;14(1):63-72. 2. Agu RU, Ugwoke MI, Armand M, Kinget R, Verbeke N. The lung as a route for systemic delivery of therapeutic proteins and peptides. Respir Res. 2001;2(4):198-209. 3. Available at: http://formularyjournal.mediwire.com/main/Default.aspx?P=Content&ArticleID=282691Accessed July 7, 2007. 4. Stattin P, Bjor O, Ferrari P, et al. Prospective study of hyperglycemia and cancer risk. Diabetes Care. 2007 Mar;30(3):561-7. 5. Li Y, Chang Q, Rubin BP, et al. Insulin receptor activation in solitary fibrous tumours. J Pathol. 2007 Apr;211(5):550-4. 6. Ryan CJ, Haqq CM, Simko J, et al. Expression of insulin-like growth factor-1 receptor in local and metastatic prostate cancer. Urol Oncol. 2007 Mar;25(2):134-40. 7. Mallikarjuna K, Pushparaj V, Biswas J, Krishnakumar S. Expression of insulin-like growth factor receptor (IGF-1R), c-Fos, and c-Jun in uveal melanoma: an immunohistochemical study. Curr Eye Res. 2006 Oct;31(10):875-83. 8. Dearth RK, Cui X, Kim HJ, et al. Mammary tumorigenesis and metastasis caused by overexpression of insulin receptor substrate 1 (IRS-1) or IRS-2. Mol Cell Biol. 2006 Dec;26(24):9302-14. 9. Shen MR, Hsu YM, Hsu KF, et al. Insulin-like growth factor 1 is a potent stimulator of cervical cancer cell invasiveness and proliferation that is modulated by alphavbeta3 integrin signaling. Carcinogenesis. 2006 May;27(5):962-71. 10. Belfiore A. The role of insulin receptor isoforms and hybrid insulin/IGF-I receptors in human cancer. Curr Pharm Des. 2007;13(7):671-86. 11. Zhao YL, Piao CQ, Wu LJ, Suzuki M, Hei TK. Differentially expressed genes in asbestos-induced tumorigenic human bronchial epithelial cells: implication for mechanism. Carcinogenesis. 2000 Nov;21(11):2005-10. 12. Available at: http://www.pdrhealth.com/drug_info/rxdrugprofiles/drugs/exu1734.shtml. Accessed July 7, 2007. 13. Kohler D. Aerosols for systemic treatment. Lung. 1990;168 Suppl:677-84. 14. Himmelmann A, Jendle J, Mellen A, et al. The impact of smoking on inhaled insulin. Diabetes Care. 2003 Mar;26(3):677-82. 15. Rave K, Bott S, Heinemann L, et al. Time-action profile of inhaled insulin in comparison with subcutaneously injected insulin lispro and regular human insulin. Diabetes Care. 2005 May;28(5):1077-82. 16. Henry RR, Mudaliar SR, Howland WC, III, et al. Inhaled insulin using the AERx Insulin Diabetes Management System in healthy and asthmatic subjects. Diabetes Care. 2003 Mar;26(3):764-9. 17. Schaafsma D, Gosens R, Ris JM, et al. Insulin induces airway smooth muscle contraction. Br J Pharmacol. 2007 Jan;150(2):136-42. 18. Aye M, Sheedy W, Harrison R, et al. Pulmonary vasodilation in the rat by insulin in vitro could indicate potential hazard for inhaled insulin. Diabetologia. 2003 Sep;46(9):1199-202. 19. Hermansen K, Ronnemaa T, Petersen AH, Bellaire S, Adamson U. Intensive therapy with inhaled insulin via the AERx insulin diabetes management system: a 12-week proof-of-concept trial in patients with type 2 diabetes. Diabetes Care. 2004 Jan;27(1):162-7. |