Life Extension Magazine®
Every time you purchase a Life Extension product, you directly support scientific research aimed at slowing aging, finding cures for killer diseases, and conquering death itself. Life Extension research dollars support scientists who may be on the verge of making a discovery that could result in a major step forward in combating the physical limitations of the human life span. Over the past year, we have identified novel ways of treating cancer.1,2 Unlike today’s Byzantine bureaucracy that stifles innovation, we move quickly to support projects that could result in human lives quickly being saved. Human Breast Tumor Cell LineThe first step in identifying anticancer agents is to test them in vitro (Petri dish) on human cancer cells. This enables scientists to discover compounds that can be used in animal studies, and, if successful, then tested in human clinical trials. Life Extension has entered into an agreement to fund a human breast cancer cell research laboratory with a 32-year track record of successfully identifying compounds that later demonstrate efficacy in humans. This model will allow us to determine possible synergistic effects of various nutrients, hormones, drugs, and combinations of these agents with chemotherapeutic drugs. Scientists working at this laboratory in Oklahoma City are now testing a wide range of compounds. The most exciting development has been the discovery of an analog of an existing drug that has shown significant anticancer efficacy. As you will soon read, Life Extension is expediting research to ascertain if this new analog drug is effective in the in vivo (living organism) model. For many years, Life Extension has recommended that women with estrogen receptor-positive breast cancer do not use DHEA because of concerns that it might be converted to estrogen in the body and fuel tumor growth.3,4 Research remains conflicting in this area, and we still recommend that women with estrogen receptor-positive breast cancer avoid DHEA. Interestingly, a recent study showed that in an estrogen receptor-positive breast cancer cell line, supraphysiological (higher than normal) dosing of DHEA exerted anti-proliferative effects (anticancer), whereas moderate DHEA dosing caused proliferative effects. The scientists who conducted this study concluded: “These results suggest that DHEA could be used at supraphysiologic concentrations in the treatment of breast cancer.”5
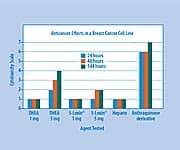
In the laboratory that Life Extension is now funding, a variety of compounds—including low-dose and high-dose DHEA— are being tested on an estrogen receptor-negative human breast cancer cell line. We have found that high-dose DHEA produces remarkable antitumor properties, which may help corroborate the recently published findings about DHEA’s anti-proliferative effects on estrogen receptor-positive breast cancer cells. While human clinical research is urgently needed, findings from our laboratory and others indicate that DHEA may hold potential as an anticancer hormone, rather than as a cancer-inducing one. For breast cancer prevention purposes, we continue to see positive findings in the published literature about the benefits of melatonin,6-11 progesterone,12-16 and DHEA,17-22 all of which point to the importance of achieving optimal hormone balance as we age. In our human breast cancer cell line, we found antitumor activity with higher-dose 5-LOXIN®, but not with lower-dose 5-LOXIN®. The drug heparin did not demonstrate efficacy in suppressing tumor growth in this breast tumor cell line. Chart 1 on this page shows the effects of compounds we have recently tested (note that the cytotoxicity scale goes from 0 to 8, with 8 being the most effective antitumor effect on this scale). Our New Analog Anticancer CompoundsAs can be seen from the chart on this page, the most effective agent tested was a primitive version of our new anthraquinone analog compound that has been discovered by our collaborators. Its anti-proliferative effects were three times more effective than high-dose DHEA at 24 hours and 43% more effective after 144 hours (six days).
We have refined the chemical characteristics of this new compound so that we can conduct the first small animal (mouse) study. These types of compounds, i.e. anthraquinone derivatives, have safer cytotoxicity performance in a human breast cancer cell line model (BOT-2) than the most successful chemotherapy compounds that are in the marketplace. The mechanism of action of these compounds will be evaluated in animal models that are being planned over the next few months. You may wonder how we can afford to develop a drug like this when pharmaceutical companies often spend over $100 million to bring out a new anticancer drug. Two advantages we have going for us are motivation and creativity. Life Extension is determined to find breakthrough therapies to help control and perhaps cure the cancer epidemic striking aging humans. Our motivation has enabled us to creatively design a protocol that will allow us to assess safety and efficacy of new compounds in small and large animal models. Life Extension is investing in the initial development phase that may eventually lead to the full commercial version of the final products. Life Extension has long criticized new drug development as taking too long and being way too costly. If the animal and human research yields the kind of results shown in our cancer cell line model, we plan to make this new analog drug available in a recordbreaking amount of time—at a fraction of the cost compared with what drug companies pay to develop new drugs. Research to Combat Advanced- Stage Breast CancerAs Life Extension long ago published, the timing of when chemotherapy drugs are administered is critically important to the long-term survival of the patient. For example, one chemotherapy drug may block certain cancer cell growth-survival mechanisms, while another drug may function via different anti-proliferative pathways. Based on favorable patient data23 and an understanding of how two FDA-approved anticancer drugs work, a Phase II clinical study is being funded by the Life Extension Foundation to ascertain the efficacy of administering Gemzar® (gemcitabine) and Taxotere® (docetaxel) on an alternatingweek dosing schedule.24
Conventional chemotherapy has a dismally high rate of failure in advanced-stage breast cancer. The objective of this $100,000 study is to show that by changing the timing of when these two existing anticancer drugs are administered, efficacy can be enhanced while minimizing the debilitating side effects of chemotherapy. You might wonder why the Life Extension Foundation is funding a study on drugs that are owned by multi-billion dollar pharmaceutical companies. The reason is simple. The pharmaceutical companies have no economic interest in trying to make their own drugs work better. These two drugs are selling briskly when used in the conventional way, so it takes a non-profit organization like the Life Extension Foundation to fund research that could enable the safety and efficacy profile of these two drugs to be greatly improved—and tens of thousands of lives potentially saved. This research project involving alternating weekly doses of Gemzar® and Taxotere® was initiated in Oklahoma City, but the inconvenience of travel has limited the number of advancedstage breast cancer patients who have enrolled in this study. Life Extension is negotiating with a major cancer center in Southern California to continue this study in an expeditious manner. According to the study’s coordinator, Orn Adalsteinsson, PhD: “We started the study in February 2007. Depending on how quickly we can sign up 25 people who meet the rigorous qualification criteria, we expect to be completed in a year to a year and a half. The researchers hope to reduce the side effects of the gemcitabine and docetaxel combination, while maintaining and hopefully maximizing the efficacy of the drugs. The findings of the Phase I study were very positive, and we expect that the Phase II study We are grateful for the assistance of the Life Extension Foundation, which is totally funding this study.” 24 Research to Combat Advanced-Stage MelanomaScientists continue to recruit patients for a clinical trial to investigate a promising new treatment for advanced melanoma called in situ photo-immunotherapy (ISPI), which has produced impressive results in preliminary findings.25 Immunotherapy—stimulating the body’s own immune system to recognize and destroy cancerous cells—is considered one of the most promising ways to treat advanced forms of the disease. ISPI may improve on this approach, as it enlists patients’ specialized defensive cells and sensitizes them to the patient’s specific tumor characteristics. ISPI makes use of an immunestimulating, topically applied skin cream used in conjunction with infrared lasers. The topical cream, imiquimod (Aldara®), binds with receptors on tumor cells and stimulates them to activate proteins that “broadcast” the presence of the tumor cells to the immune system. In essence, the patient’s own tumor cells become a unique antitumor vaccine.
Two patients with late-stage melanoma treated with ISPI are still alive—more than 38 months later in one case, and 30 months later in the second case. The median life expectancy for stage IV melanoma cases is typically six to eight months. In addition, researchers have observed shrinkage of untreated systemic metastases following therapy in at least one subject. These preliminary findings indicate that ISPI therapy may be a useful and relatively non-toxic way to treat patients with advanced melanoma. To inquire about participating in this study, contact: Lisa Perry, MA Research Coordinator Phone: 918-619-4466 Email: lisa-perry@ouhsc.edu University of Oklahoma College of Medicine, Tulsa, OK Life Extension has been aggressively seeking to enroll melanoma patients in this study as we believe it offers a realistic hope not only to control melanoma, but many other cancers as well. In anticipation of positive findings, Life Extension has already expended monies to get this treatment approved fast, so that no lives have to be lost needlessly. Life Extension does not have a financial interest in this melanoma therapy, only a humanitarian one. Your Membership Fees and Product Purchases Solely Support this Cancer ResearchBetween the federal government and various cancer societies, hundreds of billions of dollars have been spent on cancer research over the past 36 years. For most forms of cancer, improvements in survival have been mediocre, despite these vast sums of monies expended. The risk for contracting cancer increases exponentially as human beings age. Life Extension is expanding its support of innovative cancer research projects because we believe we have the expertise to make a difference. If you donate money to a cancer research organization, we ask that you reconsider and redirect your tax-deductible donations to the Life Extension Foundation and mark “Cancer Fund” on your check. We guarantee that 100% of your donation will be used to further the kind of cancer research that has a realistic potential of saving human lives very quickly. If you are unable to donate, please remember that every time you renew your membership or purchase a product from us, you help fund this critically important cancer research. In this issue, we introduce an ambitious new program to aggressively treat breast and prostate tumors, along with documented ways to reduce your risk of contracting these epidemic diseases. For longer life, | ||||||||
| References | ||||||||
| 1. Available at: www.lifeextension.com/magazine/mag2007/aug2007_itn_01.htm. Accessed Aug 20, 2007. 2. Available at: www.lifeextension.com/magazine/ mag2005/apr2005_report_female_02.htm. Accessed Aug 20, 2007. 3. Available at: http://www.lifeextension.com/dhea/ medical_information_on_dhea.html. Accessed Aug 20, 2007. 4. Available at: www.project-aware.org/ Resource/articlearchives/hrt-breastcancer.shtml. Accessed Aug 20, 2007. November 2007 LIFE EXTENSION 11 5. Gayosso V, Montano LF, Lopez-Marure R. DHEA-induced antiproliferative effect in MCF-7 cells is androgen- and estrogen receptor-independent. Cancer J. 6. Schernhammer ES, Rosner B, Willett WC, et al. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiol Biomarkers Prev. 2004 Jun;13(6):936-43. 7. Burch JB, Walling M, Rush A, et al. Melatonin and estrogen in breast cyst fluids. Breast Cancer Res Treat. 2007 Jul;103(3):331-41. 8. Schernhammer ES, Hankinson SE. Urinary melatonin levels and breast cancer risk. J Natl Cancer Inst. 2005 Jul 20;97(14):1084-7. 9. Lenoir V, de Jonage-Canonico MB, Perrin MH, et al. Preventive and curative effect of melatonin on mammary carcinogenesis induced by dimethylbenz[a]anthracene in the female Sprague-Dawley rat. Breast Cancer Res. 2005;7(4):R470-6. 10. Sanchez-Barcelo EJ, Cos S, Mediavilla D, et al. Melatonin-estrogen interactions in breast cancer. J Pineal Res. 2005 May;38(4):217-22. 11. Formby B, Wiley TS. Progesterone inhibits growth and induces apoptosis in breast cancer cells: inverse effects on Bcl-2 and p53. Ann Clin Lab Sci. 1998 Nov;28(6):360-9. 12. Mohr PE, Wang DY, Gregory WM, Richards MA, Fentiman IS. Serum progesterone and prognosis in operable breast cancer. Br J Cancer. 1996 Jun;73(12):1552-5. 13. Kaaks R, Berrino F, Key T, et al. Serum sex steroids in premenopausal women and breast cancer risk within the European Prospective Investigation into Cancer and Nutrition (EPIC). J Natl Cancer Inst. 2005 May 18;97(10):755-65. 14. Cowan LD, Gordis L, Tonascia JA, Jones GS. Breast cancer incidence in women with a history of progesterone deficiency. Am J Epidemiol. 1981 Aug;114(2):209-17. 15. Jerry DJ. Roles for estrogen and progesterone in breast cancer prevention. Breast Cancer Res. 2007;9(2):102. 16. Wiebe JP. Progesterone metabolites in breast cancer. Endocr Relat Cancer. 2006 Sep;13(3):717-38. 17. Adly L, Hill D, Sherman ME, et al. Serum concentrations of estrogens, sex hormonebinding globulin, and androgens and risk of breast cancer in postmenopausal women. Int J Cancer. 2006 Nov 15;119(10): 2402-7. 18. Tworoger SS, Missmer SA, Eliassen AH, et al. The association of plasma DHEA and DHEA sulfate with breast cancer risk in predominantly premenopausal women. Cancer Epidemiol Biomarkers Prev. 2006 May;15(5):967-71. 19. Hardin C, Pommier R, Calhoun K, et al. A new hormonal therapy for estrogen receptor- negative breast cancer. World J Surg. 2007 May;31(5):1041-6. 20. Labrie F. Drug insight: breast cancer prevention and tissue-targeted hormone replacement therapy. Nat Clin Pract Endocrinol Metab. 2007 Aug;3(8):584-93. 21. Toth-Fejel S, Cheek J, Calhoun K, Muller P, Pommier RF. Estrogen and androgen receptors as comediators of breast cancer cell proliferation: providing a new therapeutic tool. Arch Surg. 2004 Jan; 139(1):50-4. 22. Shilkaitis A, Green A, Punj V, et al. Dehydroepiandrosterone inhibits the progression phase of mammary carcinogenesis by inducing cellular senescence via a p16-dependent but p53-independent mechanism. Breast Cancer Res. 2005; 7(6):R1132-40. 23. Syrigos KN, Konstantinou M, Sepsas E et al. Biweekly administration of docetaxel and gemcitabine as adjuvant therapy for stage II and IIIA non-small cell lung cancer: a phase II study. Anticancer Res. 2007 Jul;27(4C):2887-92. 24. Available at: www.lifeextension.com/magazine/mag2007/may2007_report_lef_01.htm. Accessed Aug 30, 2007. 25. Naylor MF, Chen WR, Teague TK, Perry LA, Nordquist RE. In situ photoimmunotherapy: a tumour-directed treatment for melanoma. Br J Dermatol. 2006 Dec;155(6):1287-92. |