Life Extension Magazine®
Reducing Risks of COX-2 InhibitorsDespite the FDA’s approval of COX-2 inhibitor drugs because of reduced incidences of gastric ulceration, a growing number of studies shows that COX-2 inhibitors still cause numerous upper gastrointestinal problems. Some studies suggest that COX-2 inhibitors are no better than the classic nonsteroidal anti-inflammatory drugs (NSAIDs) that they were supposed to replace.18 NSAIDs suppress both the COX-1 and COX-2 enzymes.
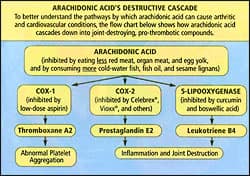
If you are taking a COX-2 inhibitor drug, the first step in reducing risk of heart attack and stroke caused by excess thromboxane A2 is to suppress the COX-1 enzyme.11 Ask your doctor if you can take just 81 mg of aspirin every other day to reduce your risk of developing a life-threatening arterial blood clot. Some studies show the COX-1-inhibiting effects of aspirin last for 48 hours or longer,19 so taking 81 mg of a coated aspirin tablet every other day may suppress enough thromboxane A2 to prevent a heart attack, while not damaging the stomach. The second step is to guard against the excess accumulation of artery-damaging leukotriene B4. One way to accomplish this is to reduce its mother substrate, arachidonic acid. This can be done by increasing your consumption of foods rich in omega-3 fatty acids, by taking fish oil supplements, and by decreasing your consumption of foods high in omega-6 fatty acids, especially red meat.17 Nutrients that suppress the 5-lipooxygenase enzyme (5-LOX) include a standardized boswellic acid extract20 (trademarked 5-Loxin™) and curcumin.21 Since blocking COX-2 deprives the arteries of beneficial prostacyclin (prostaglandin I2),11 have your blood evaluated at least once a year to identify all risk factors for heart attack and stroke, and take aggressive preventive actions if any parameters are not in the optimal ranges. If one is to take any drug that may inhibit too much COX-1 (and this includes the COX-2 inhibitors), consuming 1800 mg a day of polyenylphosphatidylcholine provides a considerable degree of protection to the stomach lining.
Is Celebrex® Safe?To date, the limited studies of the COX-2 inhibitor Celebrex® do not show an increased heart attack or stroke risk from using this drug. One study indicated that Celebrex® is sufficiently different from Vioxx® to not cause cardiovascular problems; however, this difference did not relate to the pathological mechanisms inherent to COX-2 inhibitor drugs, as discussed in the preceding paragraphs. Celebrex® is a potent COX-2 inhibitor, and those who find relief from arthritis pain by taking it should follow all the precautions outlined in these paragraphs. The question on the minds of many doctors and patients is, are other drugs in the “coxib” category safe? There are at least six such drugs: celecoxib (Celebrex®), valdecoxib (Bextra®), meloxicam (Mobic®), lumiracoxib (Prexige®), parecoxib (Dynastat®), and etoricoxib (Arcoxia®). Only three of these are available in the US. Recent research indicates that the sulfone component of the Vioxx® molecule, and perhaps that of the etoricoxib molecule, may be related to the occurrence of adverse side effects,22 so non-sulfone coxibs such as Celebrex® may be safer. A look at the underlying mechanisms by which COX-2 inhibitors cause adverse cardiovascular events reveals considerable reasons for concern with any drug in this class. Pfizer reports that its drug Celebrex® has not been associated with an increased risk of heart attack and stroke in large, long-term studies.23 Bextra®, also from Pfizer, does seem to increase cardiovascular events in people who have undergone a coronary bypass graft.10 Additional studies of both drugs are planned.24,25 With Vioxx® out of the picture, and the safety of other coxib drugs suspect, arthritis sufferers may increasingly rely on other, older drugs. However, many of these older drugs can cause significant gastrointestinal side effects, making them undesirable choices for the long-term management of arthritis. Fortunately, several effective natural remedies for arthritis pain and inflammation are readily available, including fish oil, boswellia, citrus flavonoids, glucosamine, and methylsulfonylmethane. These natural therapies promise to help reduce inflammation and manage arthritis symptoms without the risks associated with commonly used prescription and over-the-counter medications. Despite the negative publicity about Vioxx®, there is still good reason to inhibit excess cyclooxygenase-2, especially from a cancer-prevention standpoint. Taking the natural approaches suggested in this article to suppress all of the chronic inflammatory inducers would appear to be far safer than resorting to potent drugs that only function by one mechanism.
What Arthritis Is and Is NotArthritis is one of our most prevalent chronic health problems, and second only to heart disease as a cause of work disability. More women than men have arthritis. Although arthritis is often seen as an older person’s disease, more than half of those afflicted are under the age of 65.26
Many kinds of arthritis exist—it comprises perhaps 100 different diseases—but the most common forms are osteoarthritis, rheumatoid arthritis, gout, ankylosing spondylitis, juvenile arthritis, lupus, and scleroderma. The most common kind by far is osteoarthritis, which occurs with advancing age and is caused by degeneration of the cartilage “cushions” at the ends of bones, so that bones rub directly against each other. Rheumatoid arthritis afflicts 2.1 million Americans, mostly women, and like lupus and scleroderma, it is thought to be an autoimmune disease caused by the body reacting against its own connective tissue. Gout, which affects mostly men, is caused by the metabolic waste product uric acid crystallizing in one or another of the small joints, causing pain and inflammation. Arthritis is distinct from other causes of musculoskeletal pain, which can include stiff or spasmed muscles, sprained ligaments and tendons, or vague aches and pains. By definition, arthritis is inflammation affecting the joints, which can occur from any number of causes. The affected joints may be hot, swollen, and painful, but are not always symptomatic. For instance, osteoarthritis of the spine, often seen as changes on an X-ray, may be free of symptoms.
Anti-Inflammatory Drugs and NutrientsThe mechanisms involved in inflammation are complex. Perhaps the oldest class of arthritis drug is the NSAIDs, which began with the folk remedy, white willow bark. This bark’s active ingredient is salicylic acid. White willow bark’s efficacy inspired a chemist to synthesize acetyl-salicylic acid, which is today known as aspirin. Ibuprofen, indomethacin, naproxen, diclofenac, and others are also members of the NSAID family. The trouble with most NSAIDs is that they are not very specific, and inhibit both the COX-1 and COX-2 enzymes. Because COX-1 is involved in protecting the stomach lining, its inhibition can cause undesirable side effects, including stomach inflammation or ulcers. Pharmaceutical chemists thought they had something better and safer when the selective COX-2 inhibitors, like Vioxx®, became available.27 It now appears that their optimism was unwarranted. Several effective inhibitors of inflammation were invented by nature long before there were arthritic people who needed to use them. Today these are being combined into effective formulations that provide safe alternatives to the COX-2 inhibitor drugs. Omega-3s: Heart-Friendly FatsOne of the most powerful ways to reduce inflammation in the body is to optimize intake of fatty acids. While the intake of certain fats, such as hydrogenated oils from margarine and processed foods, can increase inflammation, other fats promote an anti-inflammatory biochemistry. The metabolism of fatty acids yields prostaglandins that may be either inflammatory or anti-inflammatory. Strictly speaking, only two fatty acids are nutritionally essential: linoleic acid and alpha-linolenic acid. Our bodies can make all the rest, but with varying degrees of efficiency. A key enzyme called delta-6 desaturase can be impaired because of age, alcohol abuse, B- vitamin deficiency, or diabetes and hyperinsulinism. In that case, relatively less gamma linolenic acid (GLA) and eicosapentaenoic acid (EPA) will be produced, causing a biochemical environment that is more susceptible to inflammation. The delta-6 desaturase enzyme also acts on EPA to transform it to docosahexaenoic acid (DHA), another anti-inflammatory fatty acid.28 GLA is the precursor of DGLA, which becomes the anti-inflammatory prostaglandin 1 (PGE-1).29 Supplemental GLA from sources such as evening primrose oil, black currant oil, and borage oil can be used to help control inflammation. EPA and DHA reduce levels of joint-destroying inflammatory cytokines, such as tumor necrosis factor-alpha and interleukin-6 (IL-6).30 These omega-3 fatty acids also suppress levels of the inflammatory mediators leukotriene B4 and prostaglandin E2.31 EPA also is metabolized to an anti-inflammatory prostaglandin, PGE-3.30 Excellent dietary sources of DHA and EPA are salmon, other oily cold-water fish, and fish oil. The body can also make EPA from alpha-linolenic acid, a fatty acid found in flaxseed oil. Modern eating habits promote an imbalance in dietary fatty acids, creating a biochemical environment that is conducive to inflammatory pathologies. The ancestral human diet contained about an equal balance of omega-6 fatty acids (such as arachidonic acid) and omega-3 fatty acids (such as EPA and DHA). A century ago, this dietary ratio of omega-6 fats to omega-3 fats was approximately 4:1, but today it equals or exceeds 20:1, mainly due to increased consumption of omega-6-rich vegetable oils, such as corn oil.32 Supplementing with omega-3 fatty acids is a beneficial strategy for reducing the inflammation inherent in many modern health disorders, including arthritis. An appropriate daily dose of fish oil is 2-3 grams of an EPA-DHA combination. This dosage has been found to relieve painful joints and reduce morning stiffness in patients with rheumatoid arthritis.33 | |||||||||||
Boswellia Inhibits 5-LOXNative to Asia, the Boswellia serrata tree produces a gummy sap that traditional medical practitioners have used for inflammation and arthritis. A key constituent of the sap is beta-boswellic acid, which scientists have found to be an effective inhibitor of the 5-LOX inflammatory enzyme.20 A standardized beta-boswellic acid preparation called 5-Loxin™, available in certain natural anti-inflammatory preparations, makes it possible to obtain the benefits of 5-LOX inhibition without consuming large quantities of ordinary boswellia extract.
Anti-Inflammatory Citrus FlavonoidsA specialized group of flavonoids from citrus offers numerous benefits in fighting inflammation. These compounds, called polymethoxylated flavonoids, have been found to benefit the cardiovascular system by lowering levels of cholesterol, LDL, and triglycerides. (See “Novel Dietary Supplement Shows Dramatic Effects in Lowering Cholesterol, LDL, and Triglycerides,” Life Extension, November 2004.) In light of recent findings regarding Vioxx®, which improves arthritis symptoms while placing the cardiovascular system at risk, this is a welcome side benefit to citrus flavonoids. Polymethoxylated flavonoids provide antioxidant protection and suppress inflammation. One of these flavonoids is very effective at inhibiting expression of the inflammatory cytokines tumor necrosis factor-alpha and IL-10.34 Several flavonoids, including tangeretin, sinensetin, and nobiletin, have been shown to suppress PGE-2 and matrix metalloproteinase production in joint cells, suggesting a chondroprotective effect of citrus bioflavonoids.35 In particular, the flavonoid nobiletin has been identified as a novel anti-inflammatory agent that has the potential to inhibit the degradation of articular cartilage in osteoarthritis and rheumatoid arthritis.35 Nobiletin has also been found to interfere with numerous inflammatory cytokines, including interleukin-1 beta and interleukin-6.36 These anti-inflammatory effects are comparable to those seen with powerful anti-inflammatory steroids such as dexamethasone. Tangeretin, another citrus flavonoid, has been found to offer complementary effects against inflammation.37
Glucosamine Promotes Healthy JointsThe cartilage between joints acts as a shock absorber, protecting the bones and tissues from the impact creating during walking and other bodily movements. Glycosaminoglycans are long, unbranched molecules of repeating pairs of sugars that help cushion the joints from wear and tear. These highly viscous molecules exist in the extracellular matrix, making them ideal as a lubricating fluid for the joints. Glucosamine is a natural remedy that has been found to be useful in promoting healthy joints. Glucosamine is an amino sugar that is crucial for the construction of glycosaminoglycans in articular cartilage. Reduced glycosaminoglycans content in osteoarthritic cartilage matrix has been found to correlate with the severity of osteoarthritis. Oral glucosamine appears to promote the secretion of more glycosaminoglycans by chondrocytes. Clinically, glucosamine has demonstrated benefits in patients with arthritis of the hip or knee.38 Clinical evidence suggests that glucosamine helps maintain the joint space and may help rebuild damaged cartilage. By contrast, NSAIDs have a propensity to make cartilage deteriorate.39 Glucosamine also inhibits certain enzymes that destroy cartilage, including collagenase and phospholipase. By blocking pathogenic mechanisms that lead to joint degeneration, glucosamine delays the progression of osteoarthritis and relieves symptoms even for weeks after termination of the treatment.40 Glucosamine is becoming recognized as a treatment of choice for osteoarthritis. Its ability to repair and improve joint function, in addition to providing pain relief, gives it a significant advantage over conventional treatments. Additionally, glucosamine may stimulate new tissue growth and suppress the enzymes that otherwise break down cartilage.
Multiple Benefits of MethylsulfonylmethaneMethylsulfonylmethane is another natural remedy that may benefit individuals with arthritis. A naturally occurring, organic sulfur compound found in human diets and those of virtually all other vertebrates, methylsulfonylmethane is produced by the body as a result of the foods we eat. In vertebrates, the body’s concentration of methylsulfonylmethane decreases with age. Some research suggests a minimum concentration of methylsulfonylmethane must be maintained in the body to preserve normal function and structure. In experiments using radiolabeled sulfur, it was shown that after ingestion, methylsulfonylmethane gives up its sulfur to the essential amino acids methionine, cysteine, and other serum proteins, eventually finding its way into the collagen of skin, joints, and blood vessels. It is also incorporated in the keratin of hair and nails. Animal studies have shown that joints affected by osteoarthritis have lower sulfur content,41 and that arthritic mice given methylsulfonylmethane experience less joint degeneration.42 In a double-blind trial in people with osteoarthritis, subjects who received methylsulfonylmethane experienced significant pain relief.43 Methylsulfonylmethane is known to be safe and nontoxic.
A small, uncontrolled study of arthritic women conducted by Stanley W. Jacob, MD, indicated that methylsulfonylmethane was as effective as ibuprofen, but without the latter’s side effects.44 Much of what we know about methylsulfonylmethane comes from Dr. Jacob’s 20 years of experience in the renowned DMSO Clinic at Oregon Health Sciences University. Methylsulfonylmethane is in fact a derivative of DMSO (dimethylsulfoxide), another powerful arthritis fighter. Methylsulfonylmethane is a small but highly effective molecule that inhibits pain impulses along nerve fibers, quells inflammation, increases blood supply, reduces muscle spasms, and softens scar tissue. Methylsulfonylmethane relieves pain and inflammation in osteoarthritis, rheumatoid arthritis, lupus, scleroderma, and fibromyalgia. It has also been reported to be helpful in allergies, back pain, headaches, temporomandibular joint dysfunction, tendonitis, and more. Most users take 1000-3000 mg daily, but some require more. Methylsulfonylmethane can be applied topically as well as taken orally.44
Synergistic Effects of Glucosamine, MethylsulfonylmethaneIn an exciting new study, the combination of glucosamine with methylsulfonylmethane was found to be more effective in improving the signs and symptoms of osteoarthritis than the use of either agent alone.45 Glucosamine is known as a chondroprotective agent since it helps to protect and restore joint cartilage. Methylsulfonylmethane is known to be an effective natural analgesic and anti-inflammatory. In this study, 118 patients with mild to moderate osteoarthritis were treated three times daily for 12 weeks with either 500 mg of glucosamine, 500 mg of methylsulfonylmethane, a combination of both, or an inactive placebo. The patients were evaluated for pain, inflammation, and swelling at 0, 2, 4, 8, and 12 weeks.45 Glucosamine, methylsulfonylmethane, and the combination of glucosamine and methylsulfonylmethane significantly relieved the pain and swelling of osteoarthritis compared with placebo. After 12 weeks of treatment, the average pain score in the glucosamine-only group dropped from 1.74 to 0.65. In the methylsulfonylmethane-only group, the score fell from 1.53 to 0.74. In the group taking both glucosamine and methylsulfonylmethane, however, the average pain score dropped from 1.70 to 0.36. The researchers also found that the combination therapy had a faster effect on pain and inflammation than either glucosamine or methylsulfonylmethane alone.45 The study authors concluded that the combination of glucosamine with methylsulfonylmethane provides better and more rapid improvement in patients with osteoarthritis than either agent alone. Practical Advice on Nutrients and DrugsThe nutritional management of arthritis goes far beyond the items discussed in this article. Additional nutrients important for those suffering with arthritis include vitamin C, antioxidants, B-complex vitamins, and trace minerals, especially selenium and copper. A healthy, natural diet is fundamental to managing inflammatory conditions such as arthritis (see the sidebar, “Nutrients for Healthy Joints”). Nutritional and herbal remedies may offer a safe, effective first line of therapy for many arthritis sufferers. Natural remedies—including fish oil, boswellia, citrus flavonoids, glucosamine, and methylsulfonylmethane—have been found to effectively reduce inflammation and protect joint health. For those experiencing more severe arthritis that requires powerful drugs such as COX-2 inhibitors, nutritional and herbal agents used concomitantly may allow lower drug doses. A physician should be consulted when combining prescription drugs with natural remedies. Prescription and over-the-counter medications are often the doctor’s first choice for treating pain and inflammation. Given the risks inherent in these drugs, as evidenced by the recent withdrawal of Vioxx® from the market, this may not be a safe or prudent choice. When nutritional substances like fish oil, boswellia, citrus flavonoids, glucosamine, and methylsulfonylmethane are used as a first line against arthritis pain, drugs can become a last resort. Some people will need drugs, but many others will find relief from pain and inflammation without the risk of toxic side effects. | |||||||
| References |
| 1. Available at: http://www.merck.com/newsroom/press_releases/product/2004_0930.html. Accessed November 22, 2004. 2. Available at: http://www.rheumatology.org/annual/press. Accessed October 24, 2004. 3. Marsa M. What now for pain? With Vioxx off the market, consumers face tough decisions. Los Angeles Times. October 11, 2004:F1-F8. 4. Topol EJ. Failing the public health—rofecoxib, Merck, and the FDA. N Engl J Med. 2004 Oct 21;351(17):1707-9. 5. Cheng Y, Austin SC, Rocca B, et al. Role of prostacyclin in the cardiovascular response to thromboxane A2. Science. 2002 Apr 19;296(5567):539-41. 6. de Leval X, Hanson J, David JL, Masereel B, Pirotte B, Dogne JM. New developments on thromboxane and prostacyclin modulators part II: prostacyclin modulators. Curr Chem Med. 2004 May;11(10):1243-52. 7. Penglis PS, Cleland LG, Demasi M, Caughey GE, James MJ. Differential regulation of prostaglandin E2 and thromboxane A2 production in human monocytes: implications for the use of cyclooxygenase inhibitors. J Immunol. 2002 Aug 1;165(3):1605-11. 8. Rubinsztajn R, Wronska J, Chazan R. Urinary leukotriene E4 concentration in patients with bronchial asthma and intolerance of non-steriods anti-inflammatory drugs before and after oral aspirin challenge. Pol Arch Med Wewn. 2003 Aug;110(2):849-54. 9. Subbarao K, Jala VR, Mathis S, et al. Role of leukotriene B4 receptors in the development of atherosclerosis: potential mechanisms. Arterioscler Thromb Vasc Biol. 2004 Feb;24(2):369-75. 10. Laufer S. Role of eicosanoids in structural degradation in osteoarthritis. Curr Opin Rheumatol. 2003 Sep;15(5):623-7. 11. Catella-Lawson F. Vascular biology of thrombosis: platelet-vessel wall interactions and aspirin effects. Neurology. 2001;57(5 Suppl 2):S5-7. 12. James MJ, Penglis PS, Caughey GE, Demasi M, Cleland LG. Eicosanoid production by human monocytes: does COX-2 contribute to a self-limiting inflammatory response? Inflamm Res. 2001 May;50(5):249-53. 13. Pommery N, Taverne T, Telliez A, et al. New COX-2/5-LOX inhibitors: apoptosis-inducing agents potentially useful in prostate cancer chemotherapy. J Med Chem. 2004 Dec 2;47(25):6195-206. 14. Koehne CH, Dubois RN. COX-2 inhibition and colorectal cancer. Semin Oncol. 2004 Apr;31(2 Suppl 7):12-21. 15. Abou-Issa H, Alshafie G. Celecoxib: a novel treatment for lung cancer. Expert Rev Anti-Cancer Ther. 2004 Oct;4(5):725-34. 16. Harris RE, Chlebowski RT, Jackson RD, et al. Breast cancer and nonsteroidal anti-inflammatory drugs: prospective results from the Women’s Health Institive. Cancer Res. 2003 Sep 15;63(18):6096-101. 17. Manav M, Su J, Hughes K, Lee HP, Ong CN. Omega-3 fatty acids and selenium as coronary heart disease risk modifying factors in Asian, Indian, and Chinese males. Nutrition. 2004 Nov:20(11-12):967-73. 18. Lugardon S, Lapeyre-Mestre M, Montastrue JL. Upper gastrointestinal adverse drug reactions and cyclo-oxygenase-2 inhibitors (celecoxib and rofecoxib): a case/non-case study from the French Phamacovigilance Database. Eur J Clin Pharmacol. 2004 Nov;60(9):673-77. 19. Feldman M, Cryer B, Rushin K, Betancourt J. A comparison of every-third-day versus daily low-dose aspirin therapy on serum thromboxane concentrations in healthy men and women. Clin Appl Thromb Hemost. 2001 Jan;7(1):53-7. 20. Kiefer D. Quenching the flames of inflammatory brain aging. Life Extension. September, 2003. 21. Chauhan DP. Chemotherapeutic potential of curcumin for colorectal cancer. Curr Pharm Des. 2002;8(19):1695-706. 22. Walter MF, Jacob RF, Day CA, et al. Sulfone COX-2 inhibitors increase susceptibility of human LDL and plasma to oxidative modification: comparison to sulfonamide COX-2 inhibitors and NSAIDs. Atherosclerosis. 2004 Dec;177(2):235-43. 23. Available at: http://www.pfizer.com/are/news_releases/2004pr/mn_2004_1001.html. Accessed November 7, 2004. 24. Available at: http://www.money.cnn.com/2004/10/15/news/fortune500/pfizer. Accessed November 22, 2004. 25. Available at: http://biz.yahoo.com/ap/041018/pfizer_celebrex_study_11.html. Accessed November 22, 2004. 26. Available at: http://www.arthritis.org/resource4s/gettingstarted/default/asp. Accessed October 24, 2004. 27. Chan CC, Boyce S, Brideau C, et al. Rofecoxib [Vioxx, MK-0966; 4-(4’-methylsul fonylphenyl)-3-phenyl-2-(5H)-furanone]: a potent and orally active cyclooxygenase-2 inhibitor. Pharmacological and biochemical profiles. J Pharmacol Exp Ther. 1999 Aug;290(2):551-60. 28. Anonymous. Functional Assessment Resource Manual. Great Smokies Diagnostic Laboratory, Asheville, NC. Winter 2002:N41-N56. 29. Horrobin DF. Prostaglandin E1: physiological significance and clinical use. Wien Klin Wochenschr. 1988 Jul 15;100(14):471-7. 30. Ferretti A, Flanagan VP, Reeves VB. Occurrence of prostaglandin E3 in human urine as a result of marine oil ingestion: gas chromatographic-mass spectrometric evidence. Biochim Biophys Acta. 1988 Apr 15;959(3):262-8. 31. Mayatepek E, Paul K, Leichsenring M, et al. Influence of dietary (n-3)-polyunsaturated fatty acids on leukotriene B4 and prostaglandin E2 synthesis and course of experimental tuberculosis in guinea pigs. Infection. 1994 Mar;22(2):106-12. 32. Simopoulos AP. Omega-3 fatty acids in health and disease and in growth and development. Am J Clin Nutr. 1991 Sep;54(3):438- 63. 33. Hendler SS, Rorvik D. PDR for Nutritional Supplements, 1st Ed. Montvale, NJ: Medical Economics Co; 2001:149. 34. Manthey JA, Grohmann K, Montanari A, Ash K, Manthey CL. Polymethoxylated flavones derived from citrus suppress tumor necrosis factor-alpha expression by human monocytes. J Nat Prod. 1999 Mar;62(3):441-4. 35. Ishiwa J, Sato T, Mimaki Y, et al. A citrus flavonoid, nobiletin, suppresses production and gene expression of matrix metalloproteinase 9/gelatinase B in rabbit synovial fibroblasts. J Rheumatol. 2000 Jan;27(1):20- 5. 36. Lin N, Sato T, Takayama Y, et al. Novel anti-inflammatory actions of nobiletin, a citrus polymethoxy flavonoid, on human synovial fibroblasts and mouse macrophages. Biochem Pharmacol. 2003 Jun 15;65(12):2065-71. 37. Datla KP, Christidou M, Widmer WW, Rooprai HK, Dexter DT. Tissue distribution and neuroprotective effects of citrus flavonoid tangeretin in a rat model of Parkin- son’s disease. Neuroreport. 2001 Dec 4;12(17):3871-5. 38. Hendler SS, Rorvik D. PDR for Nutritional Supplements, 1st Ed. Montvale, NJ: Medical Economics Co; 2001:149. 39. Brandt KD. Effects of nonsteroidal anti-inflammatory drugs on chondrocyte metabolism in vitro and in vivo. Am J Med. 1987 Nov 20;83(5A):29-34. 40. Qiu GX, Gao SN, Giacovelli G, Rovati L, Setnikar I. Efficacy and safety of glucosamine sulfate versus ibuprofen in patients with knee osteoarthritis. Arzneimittelforschung. 1998 May;48(5):469-74.41. Rizzo R, Grandolfo M, Godeas C, Jones KW, Vittur F. Calcium, sulfur, and zinc distribution in normal and arthritic articular equine cartilage: a synchrotron radiation-induced X-ray emission (SRIXE) study. J Exp Zool. 1995 Sep 1;273(1):82-6. 42. Murav'ev I, Venikova MS, Pleskovskaia GN, Riazantseva TA, Sigidin I. Effect of dimethyl sulfoxide and dimethyl sulfone on a destructive process in the joints of mice with spontaneous arthritis. Patol Fiziol Eksp Ter. 1991 Mar-Apr;(2):37-9. 43. Lawrence RM. Methysulfonylmethane (MSM): a double-blind study of its use in degenerative arthritis. Int J Anti-Aging Med. 1998;1:50. 44. Jacob SW, Lawrence RM, Zucker M. The Miracle of MSM. New York: Berkley Books, 1999. 45. Usha PR, Naidu MU. Randomised, double-blind, parallel, placebo-controlled study of oral glucosamine, methylsulfonylmthane and their combination in osteoarthritis. Clin Drug Invest. 2004 Jun;24(6):353-63. 46. Takase B, Maruyama T, Kurita A, et al. Arachidonic acid metabolites in acute myocardial infarction. Angiology. 1996 Jul;47(7):649-61. 47. Foral PA, Nystrom KK, Wilson AF, Christensen CM. Gastrointestinal-related adverse effects of COX-2 inhibitors. Drugs Today. 2003 Dec;39(12):939-48. 48. Biancone L, Tosti C, Geremia A, et al. Rofecoxib and early relapse of inflammatory bowel disease: an open-label trial. Aliment Pharmacol Ther. 2004 Apr 1;19(7):755-64. |