Life Extension Magazine®
People associate excess alcohol ingestion with liver cirrhosis and brain cell damage. Alcohol, however, inflicts a more insidious effect. Epidemiological studies clearly show that those who consume large amounts of alcohol have sharply increased risks of certain cancers. Especially troubling are esophageal and brain cancers, both of which are increasing in frequency at an alarming rate. In women, even moderate alcohol consumption is linked with higher breast cancer incidence. In this article, we reveal what most of the public does not know about the carcinogenic effects of excess alcohol ingestion. We then provide some guidance as to what one may do to reduce alcohol’s damaging effects. Despite its widespread use and social acceptance, alcohol is one of the 10 leading causes of death and injury in developed countries, according to the Institute for Alcohol Studies in Cambridgeshire, England.1 The World Health Organization (WHO) estimates that alcohol causes 1.8 million deaths worldwide each year, with the highest proportions occurring in the Americas and Europe.
“Alcohol was estimated to cause, worldwide, 20–30% of esophageal cancer, liver disease, epilepsy, motor vehicle accidents, and homicide and other intentional injuries,” the WHO noted in its 2002 World Health report.2 An estimated 63% of US adults drank alcohol in the past year. Alcohol abuse occurs in approximately 6% of Americans, and may affect 10-20% of the population at some point in their lives.3 Untreated alcoholism has been estimated to reduce life expectancy by as much as 15 years.4 In its 2000 Report on Carcinogens, the US Department of Health and Human Services listed alcohol as a known human carcinogen that can cause cancers of the mouth, pharynx, larynx, and esophagus. The risk is greatest among smokers and heavy drinkers. Cancers of the oral cavity and upper airway frequently go undiscovered until their latter stages, when the death rate is very high; surgical treatment of these malignancies can cause disfigurement and difficulties with speech, chewing, and swallowing. The Report on Carcinogens further noted that evidence suggests a link between alcohol consumption and cancers of the liver and breast.5 South American scientists reported in 2003 that Chileans who are heavy drinkers (defined as consuming more than 402 grams of alcohol per week) are significantly more likely to develop hemorrhagic stroke, “a major cause of disability and death worldwide.” The more than fourfold increase in risk was independent of other factors, such as high blood pressure, cigarette smoking, or liver disease.6 The use and misuse of alcohol may also wreck havoc with the brain and the nervous system. Peripheral neuropathy—marked by pain, tingling, and loss of sensation and muscle strength in the extremities—is often the first sign of alcohol dependence.7 Alcoholic neuropathy may result from alcohol’s toxic effects on nerve tissue or may be related to alcohol-induced nutritional deficiencies.8 Alcohol can also have extensive and far-reaching effects on the brain, including contributing to memory lapses and cognitive impairment.9 Clearly, alcohol is a major toxin that can contribute to cancer, stroke, and neurodegenerative decline. Guarding against the effects of this lethal chemical is crucial to promoting optimal well-being. While the history of alcohol use dates back thousands of years, the chemistry of alcohol metabolism—what actually takes place in the body when we imbibe—is only now becoming clear. Indeed, our understanding of alcohol’s toxic effects is still evolving. We know, for example, that the liver is uniquely susceptible to injury from alcohol, as it is the organ primarily responsible for metabolizing toxins entering the bloodstream. While evidence suggests that drinking in moderation may confer modest cardiovascular benefits,10,11 make no mistake—generally speaking, alcohol is toxic to living cells. Consumed in excessive quantities, alcohol can cause acute liver injury resembling that caused by viral hepatitis. Long-term abuse may result in chronic liver disease, cirrhosis, and increased risk of developing cancers of the liver, esophagus, mouth, larynx, breast, prostate, and colon.10-18 Other conditions, such as infection with the hepatitis B or C virus, obesity, type II diabetes, or exposure to toxins such as aflatoxin or vinyl chloride, may increase alcohol’s carcinogenic effects in a synergistic manner.16 One should avoid consuming alcohol in quantities sufficient to produce a morning-after hangover. Described as a “constellation of unpleasant physical and mental symptoms that occur between 8 and 16 hours after drinking alcohol,”19 a hangover may be nature’s way of telling us that we have overindulged. In fact, recent research associates morning-after hangovers with diminished memory, cognition, and visual functions, even with blood alcohol levels at or near zero.19-21 Other studies have associated alcohol dependence with significantly elevated levels of interleukin-6, an inflammatory cytokine.22 When abstinence is impractical or undesirable, it is possible to counteract some of the harmful effects of alcohol consumption. Scientists have identified several natural agents that counteract alcohol’s adverse effects on the liver.
How the Body Detoxifies AlcoholOnce ingested, alcohol must be eliminated by the body. Like other toxins, however, it must be transformed within the body before it can be safely removed. This transformation, or metabolism, of alcohol involves two major steps. First, it is oxidized to an intermediary compound, acetaldehyde, through the action of an enzyme called alcohol dehydrogenase, or a secondary enzyme, catalase. This initially takes place, to a small extent, in the stomach, and then, to a much greater extent, in the liver. After ethanol (alcohol) is converted to acetaldehyde—a compound even more toxic than alcohol—another enzyme, aldehyde dehydrogenase, converts acetaldehyde to acetate, which is eventually converted to harmless carbon dioxide and water.23,24 A secondary alcohol detoxification system involves a family of detoxifying proteins known as the cytochrome P450 enzymes, which also help metabolize alcohol. Known as the microsomal ethanol oxidizing system (MEOS), this second metabolic pathway also transforms alcohol to acetaldehyde. A highly reactive free radical known as 1-hydroxyethyl is created as a byproduct of this conversion.23,25-32 Another metabolic byproduct produced during the breakdown of acetaldehyde is a chemical called diacetyl. This previously overlooked metabolite may play an important role in generating oxidative stress that can eventually lead to the development of diseases such as Alzheimer’s and cancer, as well as genetic mutations.33 Women at Special RiskBecause men produce more alcohol dehydrogenase in their stomachs and livers than women, they metabolize more alcohol during first-pass metabolism than women. Women, on the other hand, rely more heavily on the detoxification capacity of their livers. Due to this gender-related difference, women are affected more profoundly than men by equivalent doses of alcohol,34-37 and are also more susceptible than men to the threat of developing fatty liver, cancer, cirrhosis of the liver, and brain damage when they drink.
Recent studies suggest that some Asians—who demonstrate genetic polymorphisms, or variability in the genes that code for the enzymes alcohol dehydrogenase and aldehyde dehydrogenase—are at elevated risk of developing alcohol- related liver disease, as are African-Americans of either sex.38,39 In fact, African-Americans have been dying of liver cirrhosis at a greater rate than whites of comparable age for the last 40 years.40 However, neither men nor women enjoy any relative advantages when it comes to protecting against the toxic effects of the powerful 1-hydroxy-ethyl radical. Because alcohol has substantial caloric value (7.1 calories per gram), it may displace ordinary nutrients in the diet, including antioxidants such as vitamin C, thereby causing primary malnutrition.23 Secondary malnutrition can occur later in the course of chronic alcohol use, when food is no longer properly digested and absorbed by the gastrointestinal tract.30,41-43 Long-term alcohol abuse often leads to a condition known as cirrhosis, which is responsible for the high rate of mortality among heavy drinkers. While liver disease was long thought to be caused by malnutrition, scientists eventually demonstrated that alcohol causes liver cirrhosis even in the absence of nutritional deficiencies. Liver cirrhosis was the twelfth leading cause of death in the US in 2000.35,44 The correlation between alcohol intake and cirrhosis is confirmed in epidemiological data gathered in the last century. For example, Canadian scientists recently analyzed alcohol consumption and cirrhosis incidence in the US before, during, and after Prohibition. The data provide striking evidence of the close correlation between drinking and incidence of the disease. As alcohol consumption plummeted during the Prohibition era, cirrhosis closely followed suit. With the repeal of Prohibition, drinking resumed with gusto, as did diagnoses of fatal liver cirrhosis. The nefarious cause-and-effect relationship between alcohol consumption and deadly cirrhosis continues to this day.35 | ||||||
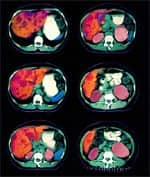
Alcohol and the LiverDuring first-pass metabolism of alcohol, the coenzyme nicotinamide adenine dinucleotide (NAD) is converted to its reduced form, NADH. NAD and NADH are compounds involved in the synthesis of the energy molecule adenosine triphosphate (ATP) within the mitochondria. Production of excess NADH upsets the delicate reduction/oxidation, or redox, balance in liver cells. Excess alcohol ingestion promotes fatty acid synthesis, causing a rise in liver fatty acid content. This saturates the liver with lipids, causing “fatty liver,” or steatosis, a first step on the path to more serious liver disease. Elevation of blood lipids, including high-density lipoprotein (HDL), may also occur.23 In recent years, the mild increase in HDL induced by alcohol has been touted as playing a beneficial role in the reduction of cardiovascular disease and incidence of stroke.23 But alcohol’s other effects are less benign. The acetaldehyde produced during alcohol metabolism is a mutagenic agent, capable of producing harmful genetic mutations that may trigger various cancers.45-47 Some of alcohol’s worst effects, however, are caused by the free radicals produced as a result of its metabolism. These rogue molecules steal hydrogen ions from fatty acids in the cell membranes, triggering a chain reaction that damages or destroys cell membranes, a process referred to as lipid peroxidation.48 Metabolism of alcohol provokes a striking increase in the activity of cytochrome P450 liver enzymes, especially a subset enzyme known as 2E1. Studies show that 2E1 liver enzymes are four to 10 times higher in people who have recently consumed alcohol than in non-drinking controls. This liver enzyme converts various compounds to highly toxic metabolites. One consequence of drinking, therefore, is the production of toxic metabolites that would otherwise not occur. For example, many pesticides are normally converted to non-carcinogenic compounds in the livers of non-drinkers. But among alcohol drinkers, they are converted to carcinogens—compounds known to have cancer-promoting properties.47
Glutathione and N-acetylcysteineGlutathione, one of the body’s most important natural antioxidants, plays a key role in alcohol detoxification. In the liver, glutathione binds to toxins and transforms them into compounds that can be excreted in the bile or urine. The liver’s supply of glutathione may be exhausted by binding to carcinogens produced during alcohol detoxification by the liver. The direct conjugation of acetaldehyde and glutathione has been observed in acute models of alcohol ingestion. When depleted by chronic alcohol ingestion, glutathione becomes unavailable for ordinary regulatory processes. N-acetylcysteine is an antioxidant supplement that has been shown to help restore depleted glutathione levels.49 Studies in rats suggest that oral glutathione supplementation may restore glutathione levels that have been depleted by toxins.50,51 Preventing glutathione depletion is important in preventing alcoholic hangover and averting the damaging effects of even moderate amounts of alcohol. Vitamin CVitamin C is one of the essential nutrients depleted by alcohol consumption.52 Because it is the body’s primary water-soluble dietary anti-oxidant, this depletion results in severe oxidative stress in daily drinkers.42 Vitamin C is also an essential co-factor for many enzymes, and its depletion lowers levels of internally produced antioxidant enzymes such as superoxide dismutase (SOD), catalase, and glutathione peroxidase.53 Low levels of these antioxidants may be associated with increased rates of cancers in humans, whether or not they consume alcohol.54 Vitamin C protects human brain cells against the damaging effects of alcohol exposure in several ways. Although alcohol increases brain cell levels of inflammatory mediators such as COX-2 and PGE-2, these remain at low levels when adequate vitamin C is present. Scientists have shown that brain cells enriched with vitamin C contain low levels of heat shock protein, even after exposure to alcohol. But cells not enriched with vitamin C produce high levels of heat shock protein upon exposure to alcohol.55 Heat shock protein activates glial cells, which damage other human brain cells when both are exposed to alcohol. Heat shock proteins are overexpressed in vascular disease and spinal disease, and appear to be involved in the death execution pathways of brain cells (apoptosis).56,57 Vitamin C supplementation is essential to protecting brain cells against oxidative damage caused by alcohol exposure. Vitamin EVitamin E is the most vital fat-soluble antioxidant and complements vitamin C and the important liver antioxidant glutathione. Vitamin E, which comprises eight structurally related tocopherols and tocotrienols, is capable of numerous actions within the body.58 As an antioxidant, it imbeds itself in the fat-soluble portions of cell membranes, where it counters free radical reactions in the fatty acid chains that are critical to the architecture and proper functioning of the membranes. Vitamin C regenerates vitamin E back to its reduced form, so that vitamin E, once spent, is able to rejoin the fray.59-61 Brain and liver cells contain the lion’s share of lipids among the body’s organs, and lipid peroxidation rates are highest in the brain and liver due to their fat content. Accordingly, vitamin E content is also highest in these organs. Alcohol contributes heavily to lipid peroxidation in both organs.58,62,63 Nature has tailored vitamin E to block the peroxidation process, thus explaining its concentration in these two organs and its depletion by alcoholism and cirrhosis.53,62,64 Vitamin E is an essential nutrient that may prevent damage caused by alcohol in the brain and liver.65,66 As such, it is a supplement that should always be taken by those who consume alcohol.
Thiamine and BenfotiamineThiamine (vitamin B1) is an essential water-soluble vitamin. Thiamine deficiency can cause lethargy, fatigue, apathy, impaired awareness, loss of equilibrium, disorientation, memory loss, anorexia, muscular weakness, and eventually death.67 Alcohol consumption depletes thiamine and produces the same symptoms as non-alcoholic thiamine deficiency.68 Thiamine deficiency damages brain cells and other nerve cells throughout the body. Thiamine deficiency—rather than the toxic effects of ethanol—has been proposed as the primary cause of cerebellar degeneration in alcoholics.69 Allithiamines are naturally occurring fat-soluble thiamines that have demonstrated a superior ability to penetrate cell membranes. The most common allithiamine, benfotiamine, has much greater bioavailability than thiamine. Benfotiamine prevents glucose from reacting with proteins in the body to form potentially harmful compounds called advanced glycation end products.70 Blocking this process helps preserve the structure and function of retinal, nerve, kidney, and other cells. Studies have shown that benfotiamine completely blocks advanced glycation end products from forming, while thiamine has no such effect. One study concluded that benfotiamine supplementation is absolutely essential for patients suffering from chronic alcohol abuse.71 Other studies have shown that benfotiamine increases thiamine status much more effectively than thiamine supplementation alone after chronic alcohol use.72 Supplementing with both fat-soluble benfotiamine and water-soluble thiamine therefore is essential to preventing some of chronic alcohol consumption’s most damaging effects. ChlorophyllinChlorophyllin, a water-soluble form of the green plant pigment chlorophyll, is among the most powerful gene protectors—or antimutagenic agents—ever discovered. Used extensively as a food colorant, it has numerous medicinal applications and has proven to be an effective anti-carcinogen in animal models of liver cancer.73 Chlorophyllin is an “interceptor molecule” that bonds to the carbon-chain backbone of hydrocarbon carcinogens and allows them to be excreted in the feces.74 It has been shown to be effective at the extremely low dose of 1 mg per kilogram of body weight in both animal and human studies. (It is rare to find a supplement for which the doses used in animal studies are virtually identical to the doses found to be effective in humans.) In numerous human and animal studies, chlorophyllin has been shown to protect the liver against environmental carcinogens and those produced by the liver itself.74 Chlorophyllin also acts as an antioxidant, protecting mitochondria against oxidative damage induced by various reactive oxygen species, and inhibiting lipid peroxidation.75 Middle-aged people at high risk of contracting liver cancer served as subjects in a landmark Chinese study that demonstrated chlorophyllin’s remarkable protective effects against liver-activated dietary carcinogens. This randomized, double-blind, placebo-controlled chemoprevention trial tested whether chlorophyllin could affect levels of the dietary toxin aflatoxin in the subjects’ livers. Nearly 200 adults were randomly assigned to ingest 100 mg of chlorophyllin or a placebo three times daily for four months. Subjects who took chlorophyllin lowered their load of the studied carcinogen by 55%. The investigators estimated that this could help protect these adults from developing cancer for 20 or more years beyond the age when liver cancer commonly occurs, thus extending life significantly in this Chinese population.76 In several studies, chlorophyllin has also been shown to protect against the harmful chromosome-breaking and mutating effects of commonly used pesticides and chemotherapy drugs. This is notable, as alcohol may induce the liver to metabolize pesticides into considerably more toxic compounds than it would otherwise normally do.77-80 | |||||
Grape Seed ExtractIts abundance of polyphenols and high bioavailability make grape seed extract one of nature’s most powerful antioxidants. Grape seed extract protects multiple organs against the toxic effects of diverse drugs and chemicals, while also enhancing the growth and viability of normal cells.81 Grape seed’s proanthocyanidins protect against chemotherapeutic drug-induced cytotoxicity in human liver cells, as well as against a variety of liver-toxic drugs such as acetaminophen.81 Grape seed proanthocyanidins prevent the oxidative stress that ordinarily occurs after a high-fat meal.82 They also prevent organ toxicity by minimizing lipid peroxidation and preventing glutathione depletion.83 Grape seed extract has been shown to be effective in preventing diseases associated with alcohol consumption, including gastric ulcers, large bowel cancer, cataracts, and diabetes.84 In human trials, grape seed was shown to prevent increased lipid peroxides in human plasma after exercise and to lessen muscle fatigue after weight training.84 Grape seed extract also causes a dose-dependent lowering of the liver’s cytochrome P450 2E1 drug-metabolizing enzyme, which is normally elevated in chronic drinkers. This enzyme is responsible for converting pesticides and other chemicals into highly toxic metabolites. In non-drinkers, who have lower levels of cytochrome P450 2E1 than drinkers, many pesticides are not converted into more toxic metabolites.81
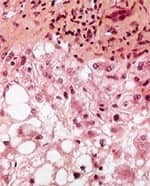
Milk Thistle ExtractIn folk medicine, milk thistle extract (Silybum marianum) traditionally has been used as a liver tonic. It has long been believed that this prickly weed, related to the artichoke, protects the liver against a variety of ailments. In the case of milk thistle, modern science has shown that ancient beliefs about a purported healing herb are based on verifiable fact. Numerous studies have shown that this archaic remedy fights inflammation and enhances the immune system. In fact, silibinin and silymarin—the two flavonoid compounds that serve as the active ingredients in milk thistle extract—are used clinically to treat liver toxicity in Europe and Asia. Studies suggest that in addition to protecting the liver, silymarin and silibinin may also help prevent cancers of the prostate, lungs, and skin, among other organs.85-93 In Vienna, scientists conducted a randomized, double-blind study of silymarin in 170 patients with liver cirrhosis. The patients, more than half of whom suffered from alcoholic cirrhosis, received 140 mg of silymarin three times daily for an average of three and a half years. Silymarin significantly improved the four-year survival rate among cirrhosis patients, including those with alcoholic cirrhosis, in contrast to control subjects who did not receive the herbal supplement. No side effects of silymarin treatment were observed, despite up to four years of continuous treatment.94 Scientists in India recently described the results of a clinical trial in which silymarin reversed markers of liver distress in patients receiving a powerful cocktail of drugs for the treatment of tuberculosis. The drugs are known to increase lipid peroxidation in the liver while depleting glutathione and raising levels of various enzymes associated with liver disease or injury. When elevated, these marker enzymes indicate pathological stress in the liver. When silymarin was administered with the antibiotic drugs, these indicators of liver health improved significantly.95 Charles S. Lieber, MD, a leading researcher in the field of alcoholic liver disease, examined silymarin’s effects on alcohol-induced liver fibrosis in baboons. “Silymarin opposed the alcohol-induced oxidative stress,” in the subjects’ livers, wrote Lieber’s research team. Noting that silymarin significantly slowed the development of alcohol-induced hepatic fibrosis, the researchers emphasized that their findings echo the results of previous studies.”96 Picrorhiza kurroaAnother exotic herb handed down by traditional medicine is Picrorhiza kurroa. A small, increasingly rare perennial herb that grows at high altitudes in the Himalayan region, Picrorhiza kurroa is prized for its liver-protecting properties.97 Picrorhiza has been shown to stimulate liver regeneration in rats, possibly by stimulating nucleic acid and protein synthesis.98 Scientists in India examined the effects of picroliv, the active constituent isolated from Picrorhiza kurroa, on alcohol-induced liver injury in living rats. Although alcohol induced various markers of liver distress, the herb improved all measured parameters of liver health.99 Its mechanism of action and efficacy appear to be similar to that of milk thistle extract, though picroliv may be even more effective than silymarin and silibinin in protecting the liver from toxic insult.97 Another study conducted in India examined picroliv’s effects on the livers of laboratory rats that were exposed to a known carcinogen. The toxin caused predictable effects, including increased lipid peroxidation and depletion of key antioxidants. Levels of antioxidants, including glutathione, were restored to normal in the livers of picroliv-treated rats. Microscopic examination of the animals’ liver tissue showed evidence of severe damage among the control animals, including cell death, inflammation, and growth of cancerous tissue. By contrast, the picroliv-fed rats had virtually normal liver tissue.100 Numerous other studies have investigated picroliv’s liver-protective effects against various toxic and biological insults, including alcohol, hepatitis virus, and various carcinogenic chemicals. All reported a significant protective effect.99-104 Although most studies have involved laboratory animals or cell cultures, human studies have also demonstrated efficacy. For example, in a randomized, double-blind, placebo-controlled trial of patients diagnosed with acute viral hepatitis, Picrorhiza kurroa extract was shown to significantly improve markers of liver health and function in supplemented patients as compared to control subjects.101
ResveratrolIronically, a constituent of wine may hold one of the keys to protecting the liver against alcohol-induced damage. Found in a variety of foods such as cranberries, peanuts, and grapes, resveratrol is a natural antioxidant. Abundant in red wine, it is believed to play an important role in the purported benefits of moderate wine consumption. Known as a phytoalexin—that is, a plant chemical responsible for preventing damage to plant tissue—and classified chemically as a polyphenolic stilbene, resveratrol has been shown to reduce both low-density lipoprotein (LDL) oxidation and the stickiness of platelets, two effects that may account for its cardioprotective benefits.105 As Spanish scientists recently noted, “Multiple lines of compelling evidence indicate [resvera-trol’s] beneficial effects on neurological, [liver], and cardiovascular systems.”106 This research team also concluded that resveratrol “blocks the multistep process of carcinogenesis at various stages: tumor initiation, promotion, and progression.”106 Other research suggests that resveratrol may help inhibit the growth of certain cancers.107 Resveratrol is thought to fight cancer by halting runaway inflammation through various discrete mechanisms, including inhibition of synthesis and release of pro-inflammatory mediators, inhibition of activated immune cells, and modification of eicosanoid synthesis.106
Barley GreenBarley green extract has been credited with reducing damage from alcohol’s oxidation to acetaldehyde in the body. Young green barley leaves contain flavonoid antioxidants, including the flavone-C-glycosides saponarin and lutonarin.108 Studies have shown that barley green extract inhibits the generation of superoxide and hydroxyl radicals in a dose-related manner.109 Moreover, tests using a rabbit model of human atherosclerosis have shown that barley leaf extract reduces atherosclerosis caused by excessively high blood lipids by 30% compared to control animals. “This 30% inhibition . . . was associated with a decrease in plasma lipids and an increase in antioxidative abilities,” noted a research team from Taiwan.110 The same team investigated the effects of young barley leaf extract on LDL oxidation and free radical scavenging activities in human patients with type II diabetes. Such individuals are at increased risk of cardiovascular disease. The study determined that barley leaf extract inhibited LDL oxidation and helped to scavenge oxygen free radicals.111 ConclusionWhile moderate alcohol consumption—particularly of resveratrol-rich red wine—may benefit the cardiovascular system,10,11 chronic alcohol abuse is anything but healthful. To guard against the toxic effects of acetaldehyde and increased free radical production generated by alcohol metabolism, it is advisable to use supplements that may prevent or ameliorate the potential damage. | ||||||
| References |
1. Available at: http://www.ias.org.uk/factsheets/health.pdf. Accessed August 29, 2005. 2. Available at: http://www.who.int/whr/ 2002/en/. Accessed August 29, 2005. 3. Available at: http://www.wrongdiagnosis.com/ a/alcohol_abuse/prevalence-types.htm. Accessed August 29, 2005. 4. Available at: http://www.intelihealth.com/ IH/ihtIH/WSIHW000/9339/9422.html.Accessed August 29, 2005. 5. Available at: http://www.niehs.nih.gov/oc/ news/9thROC.htm. Accessed August 29, 2005. 6. Diaz V, Cumsille MA, Bevilacqua JA. Alcohol and hemorrhagic stroke in Santiago, Chile. A case-control study. Neuroepidemiology. 2003 Nov-Dec;22(6):339-44. 7. Available at: http://www.emedicine.com/ NEURO/topic278.htm. Accessed August 29, 2005. 8. Available at: http://www.nlm.nih.gov/medlineplus/ency/article/000714.htm.Accessed August 29, 2005. 9. Available at: http://alcoholism.about.com/ gi/dynamic/offsite.htm?site=http://www.niaaa.nih.gov/. Accessed August 29, 2005. 10. Lieber CS. Alcohol and health: a drink a day won’t keep the doctor away. Cleve Clin J Med. 2003 Nov;70(11):945-3. 11. Rimm E. Alcohol and cardiovascular disease. Curr Atheroscler Rep. 2000 Nov;2(6):529-35. 12. Altieri A, Garavello W, Bosetti C, Gallus S, Vecchia CL. Alcohol consumption and risk of laryngeal cancer. Oral Oncol. 2005 May 28. 13. Randi G, Altieri A, Gallus S, et al. History of cirrhosis and risk of digestive tract neoplasms. Ann Oncol. 2005 May 26. 14. Morita M, Oyama T, Kagawa N, et al. Expression of aldehyde dehydrogenase 2 in the normal esophageal epithelium and alcohol consumption in patients with esophageal cancer. Front Biosci. 2005 Sep 1;10:2319-24. 15. Chang ET, Hedelin M, Adami HO, Gronberg H, Balter KA. Alcohol drinking and risk of localized versus advanced and sporadic versus familial prostate cancer in Sweden. Cancer Causes Control. 2005 Apr;16(3):275-84. 16. Voigt MD. Alcohol in hepatocellular cancer. Clin Liver Dis. 2005 Feb;9(1):151-69. 17. Dumitrescu RG, Shields PG. The etiology of alcohol-induced breast cancer. Alcohol. 2005 Apr;35(3):213-35. 18. Martinez ME. Primary prevention of colorectal cancer: lifestyle, nutrition, exercise. Recent Results Cancer Res. 2005;166:177-211. 19. Kim DJ, Yoon SJ, Lee HP, Choi BM, Go HJ. The effects of alcohol hangover on cognitive functions in healthy subjects. Int J Neurosci. 2003 Apr;113(4):581-94. 20. McKinney A, Coyle K. Next day effects of a normal night’s drinking on memory and psychomotor performance. Alcohol Alcohol. 2004 Nov;39(6):509-13. 21. Kim DJ, Kim W, Yoon SJ, et al. Effects of alcohol hangover on cytokine production in healthy subjects. Alcohol. 2003 Nov;31(3):167-70. 22. Nicolaou C, Chatzipanagiotou S, Tzivos D, et al. Serum cytokine concentrations in alcohol-dependent individuals without liver disease. Alcohol. 2004 Apr;32(3):243-7. 23. Lieber CS. Alcohol and the liver: metabolism of alcohol and its role in hepatic and extrahepatic diseases. Mt Sinai J Med. 2000 Jan;67(1):84-94. 24. Umulis DM, Gurmen NM, Singh P, Fogler HS. A physiologically based model for ethanol and acetaldehyde metabolism in human beings. Alcohol. 2005 Jan;35(1):3-12. 25. Lieber CS. ALCOHOL: its metabolism and interaction with nutrients. Annu Rev Nutr. 2000;20:395-430. 26. Quintans LN, Castro GD, Castro JA. Oxidation of ethanol to acetaldehyde and free radicals by rat testicular microsomes. Arch Toxicol. 2005 Jan;79(1):25-30. 27. Castro GD, Delgado de Layno AM, Costantini MH, Castro JA. Rat ventral prostate microsomal biotransformation of ethanol to acetaldehyde and 1-hydroxyethyl radicals: its potential contribution to prostate tumor promotion. Teratog Carcinog Mutagen. 2002;22(5):335-41. 28. Sakurai K, Stoyanovsky DA, Fujimoto Y, Cederbaum AI. Mitochondrial permeability transition induced by 1-hydroxyethyl radical. Free Radic Biol Med. 2000 Jan 15;28(2):273-80. 29. Worrall S, de Jersey J, Wilce PA. Comparison of the formation of proteins modified by direct and indirect ethanol metabolites in the liver and blood of rats fed the Lieber-DeCarli liquid diet. Alcohol Alcohol. 2000 Mar;35(2):164-70. 30. Lieber CS. Relationships between nutrition, alcohol use, and liver disease. Alcohol Res Health. 2003;27(3):220-31. 31. Lieber CS. The discovery of the microsomal ethanol oxidizing system and its physiologic and pathologic role. Drug Metab Rev. 2004 Oct;36(3-4):511-29. 32. Lieber CS. CYP2E1: from ASH to NASH. Hepatol Res. 2004 Jan;28(1):1-11. 33. Kovacic P, Cooksy AL. Role of diacetyl metabolite in alcohol toxicity and addiction via electron transfer and oxidative stress. Arch Toxicol. 2005 Mar;79(3):123-8. 34. Frezza M, di Padova C, Pozzato G, et al. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990 Jan 11;322(2):95-9. 35. Mann RE, Smart RG, Govoni R. The epidemiology of alcoholic liver disease. Alcohol Res Health. 2003;27(3):209-19. 36. Tuyns AJ, Pequignot G. Greater risk of ascitic cirrhosis in females in relation to alcohol consumption. Int J Epidemiol. 1984 Mar;13(1):53-7. 37. Becker PU, Deis A, Sorensen TI, et al. Alcohol intake and risk of liver disease—significance of gender. A population study. Ugeskr Laeger. 1997 Jun 9;159(24):3782-6. 38. Luo HR, Zhang YP. Aldehyde dehydrogenase (ALDH2) polymorphism and drinking behavior. Yi Chuan. 2004 Mar;26(2):263-6. 39. Yamauchi M, Maezawa Y, Mizuhara Y, et al. Polymorphisms in alcohol metabolizing enzyme genes and alcoholic cirrhosis in Japanese patients: a multivariate analysis. Hepatology. 1995 Oct;22(4 Pt 1):1136-42. 40. Stranges S, Freudenheim JL, Muti P, et al. Greater hepatic vulnerability after alcohol intake in African Americans compared with Caucasians: a population-based study. J Natl Med Assoc. 2004 Sep;96(9):1185-92. 41. Lieber CS. Biochemical factors in alcoholic liver disease. Semin Liver Dis. 1993 May;13(2):136-53. 42. Masalkar PD, Abhang SA. Oxidative stress and antioxidant status in patients with alcoholic liver disease. Clin Chim Acta. 2005 May;355(1-2):61-5. 43. Ryle PR, Thomson AD. Nutrition and vitamins in alcoholism. Contemp Issues Clin Biochem. 1984;1:188-224. 44. Minino AM, Arias E, Kochanek KD, Murphy SL, Smith BL. Deaths: final data for 2000. Natl Vital Stat Rep. 2002 Sep 16;50(15):1-119. 45. Theruvathu JA, Jaruga P, Nath RG, Dizdaroglu M, Brooks PJ. Polyamines stimulate the formation of mutagenic 1,N2-propanodeoxyguanosine adducts from acetaldehyde. Nucleic Acids Res. 2005;33(11):3513-20. 46. Lao Y, Hecht SS. Synthesis and properties of an acetaldehyde-derived oligonucleotide interstrand cross-link. Chem Res Toxicol. 2005 Apr;18(4):711-21. 47. Poschl G, Seitz HK. Alcohol and cancer. Alcohol Alcohol. 2004 May;39(3):155-65. 48. Lieber CS. Alcoholic fatty liver: its pathogenesis and mechanism of progression to inflammation and fibrosis. Alcohol. 2004 Aug;34(1):9-19. 49. Marzullo L. An update of N-acetylcysteine treatment for acute acetaminophen toxicity in children. Curr Opin Pediatr. 2005 Apr;17(2):239-45. 50. Vina J, Perez C, Furukawa T, Palacin M, Vina JR. Effect of oral glutathione on hepatic glutathione levels in rats and mice. Br J Nutr. 1989 Nov;62(3):683-91. 51. Aw TY, Wierzbicka G, Jones DP. Oral glutathione increases tissue glutathione in vivo. Chem Biol Interact. 1991;80(1):89-97. 52. Hancock RD, Viola R. Improving the nutritional value of crops through enhancement of L-ascorbic acid (vitamin C) content: rationale and biotechnological opportunities. J Agric Food Chem. 2005 Jun 29;53(13):5248-57. 53. Zhou JF, Chen P. Studies on the oxidative stress in alcohol abusers in China. Biomed Environ Sci. 2001 Sep;14(3):180-8. 54. Devasagayam TP, Tilak JC, Boloor KK, et al. Free radicals and antioxidants in human health: current status and future prospects. J Assoc Physicians India. 2004 Oct;52:794-804. 55. Sanchez-Moreno C, Paniagua M, Madrid A, Martin A. Protective effect of vitamin C against the ethanol mediated toxic effects on human brain glial cells. J Nutr Biochem. 2003 Oct;14(10):606-13. 56. Zhang F, Yin W, Chen J. Apoptosis in cerebral ischemia: executional and regulatory signaling mechanisms. Neurol Res. 2004 Dec;26(8):835-45. 57. Wang X, Qu WD, Ya S, et al. Effects of alcohol on the expression of heat shock protein 70 and super microstructure of astrocytes in rat embryonic brain. Wei Sheng Yan Jiu. 2005 Mar;34(2):158-60. 58. Schneider C. Chemistry and biology of vitamin E. Mol Nutr Food Res. 2005 Jan;49(1):7-30. 59. Huang J, May JM. Ascorbic acid spares alpha-tocopherol and prevents lipid peroxidation in cultured H4IIE liver cells. Mol Cell Biochem. 2003 May;247(1-2):171-6. 60. Halpner AD, Handelman GJ, Harris JM, Belmont CA, Blumberg JB. Protection by vitamin C of loss of vitamin E in cultured rat hepatocytes. Arch Biochem Biophys. 1998 Nov 15;359(2):305-9. 61. May JM, Qu ZC, Mendiratta S. Protection and recycling of alpha-tocopherol in human erythrocytes by intracellular ascorbic acid. Arch Biochem Biophys. 1998 Jan 15;349(2):281-9. 62. Prakash S, Joshi YK. Assessment of micronutrient antioxidants, total antioxidant capacity and lipid peroxidation levels in liver cirrhosis. Asia Pac J Clin Nutr. 2004;13(Suppl):S110. 63. McDonough KH. Antioxidant nutrients and alcohol. Toxicology. 2003 Jul 15;189(1-2):89-97. 64. Gutteridge JM. The membrane effects of vitamin E, cholesterol and their acetates on peroxidative susceptibility. Res Commun Chem Pathol Pharmacol. 1978 Dec;22(3):563-72. 65. Waluga M, Hartleb M. Alcoholic liver disease. Wiad Lek. 2003;56(1-2):61-70. 66. Mansouri A, Demeilliers C, Amsellen S, Pessayre D, Fromenty B. Acute ethanol administration oxidatively damages and depletes mitochondrial dna in mouse liver, brain, heart, and skeletal muscles: protective effects of antioxidants. J Pharmacol Exp Ther. 2001 Aug;298(2):737-43. 67. Martin PR, Singleton CK, Hiller-Sturmhofel S. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health. 2003;27(2):134-42. 68. Betrosian AP, Thireos E, Toutouzas K, et al. Occidental beriberi and sudden death. Am J Med Sci. 2004 May;327(5):250-2. 69. Maschke M, Weber J, Bonnet U, et al. Vermal atrophy of alcoholics correlate with serum thiamine levels but not with dentate iron concentrations as estimated by MRI. J Neurol. 2005 Jun;252(6):704-11. 70. Stracke H, Hammes HP, Werkmann D, et al. Efficacy of benfotiamine versus thiamine on function and glycation products of peripheral nerves in diabetic rats. Exp Clin Endocrinol Diabetes. 2001;109(6):330-6. 71. Netzel M, Ziems M, Jung KH, et al. Effect of high-dosed thiamine hydrochloride and S-benzoyl-thiamine-O-monophosphate on thiamine-status after chronic ethanol administration. Biofactors. 2000;11(1-2):111-3. 72. Ayazpoor U. Chronic alcohol abuse. Benfotiamine in alcohol damage is a must. MMW Fortschr Med. 2001 Apr 19;143(16):53. 73. Egner PA, Munoz A, Kensler TW. Chemoprevention with chlorophyllin in individuals exposed to dietary aflatoxin. Mutat Res. 2003 Feb;523-524:209-16. 74. Kensler TW, Egner PA, Wang JB, et al. Strategies for chemoprevention of liver cancer. Eur J Cancer Prev. 2002 Aug;11 Suppl 2S58-S64. 75. Kamat JP, Boloor KK, Devasagayam TP. Chlorophyllin as an effective antioxidant against membrane damage in vitro and ex vivo. Biochim Biophys Acta. 2000 Sep 27;1487(2-3):113-27. 76. Egner PA, Wang JB, Zhu YR, et al. Chlorophyllin intervention reduces aflatoxin-DNA adducts in individuals at high risk for liver cancer. Proc Natl Acad Sci USA. 2001 Dec 4;98(25):14601-6. 77. Della CC, Morichetti E, Intorre L, et al. Biochemical and genetic interactions of two commercial pesticides with the monooxygenase system and chlorophyllin. J Environ Pathol Toxicol Oncol. 1996;15(1):21-8. 78. Sarkar D, Sharma A, Talukder G. Differential protection of chlorophyllin against clastogenic effects of chromium and chlordane in mouse bone marrow in vivo. Mutat Res. 1993 Jan;301(1):33-8. 79. Gentile JM, Rahimi S, Zwiesler J, Gentile GJ, Ferguson LR. Effect of selected antimutagens on the genotoxicity of antitumor agents. Mutat Res. 1998 Jun 18;402(1-2):289-98. 80. Cho YS, Kim BY, Lee ST, Surh YJ, Chung AS. Chemopreventive effect of chlorophyllin on mutagenicity and cytotoxicity of 6-sulfooxymethylbenzo[a]pyrene. Cancer Lett. 1996 Oct 22;107(2):223-8. 81. Bagchi D, Bagchi M, Stohs S, et al. Cellular protection with proanthocyanidins derived from grape seeds. Ann NY Acad Sci. 2002 May;957:260-70. 82. Natella F, Belelli F, Gentili V, Ursini F, Scaccini C. Grape seed proanthocyanidins prevent plasma postprandial oxidative stress in humans. J Agric Food Chem. 2002 Dec 18;50(26):7720-5. 83. Ray SD, Lam TS, Rotollo JA, et al. Oxidative stress is the master operator of drug and chemically-induced programmed and unprogrammed cell death: Implications of natural antioxidants in vivo. Biofactors. 2004;21(1-4):223-32. 84. Ariga T. The antioxidative function, preventive action on disease and utilization of proanthocyanidins. Biofactors. 2004;21(1-4):197-201. 85. Katiyar SK. Silymarin and skin cancer prevention: anti-inflammatory, antioxidant and immunomodulatory effects (Review). Int J Oncol. 2005 Jan;26(1):169-76. 86. Lahiri-Chatterjee M, Katiyar SK, Mohan RR, Agarwal R. A flavonoid antioxidant, silymarin, affords exceptionally high protection against tumor promotion in the SENCAR mouse skin tumorigenesis model. Cancer Res. 1999 Feb 1;59(3):622-32. 87. Katiyar SK, Roy AM, Baliga MS. Silymarin induces apoptosis primarily through a p53-dependent pathway involving Bcl-2/Bax, cytochrome c release, and caspase activation. Mol Cancer Ther. 2005 Feb;4(2):207-16. 88. Singh RP, Dhanalakshmi S, Agarwal C, Agarwal R. Silibinin strongly inhibits growth and survival of human endothelial cells via cell cycle arrest and downregulation of survivin, Akt and NF-kappaB: implications for angioprevention and antiangiogenic therapy. Oncogene. 2005 Feb 10;24(7):1188-202. 89. Mallikarjuna G, Dhanalakshmi S, Singh RP, Agarwal C, Agarwal R. Silibinin protects against photocarcinogenesis via modulation of cell cycle regulators, mitogen-activated protein kinases, and Akt signaling. Cancer Res. 2004 Sep 1;64(17):6349-56. 90. Singh RP, Agarwal R. Flavonoid antioxidant silymarin and skin cancer. Antioxid Redox Signal. 2002 Aug;4(4):655-63. 91. Singh RP, Agarwal R. A cancer chemopreventive agent silibinin, targets mitogenic and survival signaling in prostate cancer. Mutat Res. 2004 Nov 2;555(1-2):21-32. 92. Chu SC, Chiou HL, Chen PN, Yang SF, Hsieh YS. Silibinin inhibits the invasion of human lung cancer cells via decreased productions of urokinase-plasminogen activator and matrix metalloproteinase-2. Mol Carcinog. 2004 Jul;40(3):143-9. 93. Tyagi A, Agarwal C, Harrison G, Glode LM, Agarwal R. Silibinin causes cell cycle arrest and apoptosis in human bladder transitional cell carcinoma cells by regulating CDKI-CDK-cyclin cascade, and caspase 3 and PARP cleavages. Carcinogenesis. 2004 Sep;25(9):1711-20. 94. Ferenci P, Dragosics B, Dittrich H, et al. Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J Hepatol. 1989 Jul;9(1):105-13. 95. Tasduq SA, Peerzada K, Koul S, Bhat R, Johri RK. Biochemical manifestations of anti-tuberculosis drugs induced hepatotoxicity and the effect of silymarin. Hepatol Res. 2005 Mar;31(3):132-5. 96. Lieber CS, Leo MA, Cao Q, Ren C, DeCarli LM. Silymarin retards the progression of alcohol-induced hepatic fibrosis in baboons. J Clin Gastroenterol. 2003 Oct;37(4):336-9. 97. Luper S. A review of plants used in the treatment of liver disease: part 1. Altern Med Rev. 1998 Dec;3(6):410-21. 98. Singh V, Kapoor NK, Dhawan BN. Effect of picroliv on protein and nucleic acid synthesis. Indian J Exp Biol. 1992 Jan;30(1):68-9. 99. Saraswat B, Visen PK, Patnaik GK, Dhawan BN. Ex vivo and in vivo investigations of picroliv from Picrorhiza kurroa in an alcohol intoxication model in rats. J Ethnopharmacol. 1999 Sep;66(3):263-9. 100. Rajeshkumar NV, Kuttan R. Modulation of carcinogenic response and antioxidant enzymes of rats administered with 1,2-dimethylhydrazine by Picroliv. Cancer Lett. 2003 Mar 10;191(2):137-43. 101. Vaidya AB, Antarkar DS, Doshi JC, et al. Picrorhiza kurroa (Kutaki) Royle ex Benth as a hepatoprotective agent—experimental & clinical studies. J Postgrad Med. 1996 Oct;42(4):105-8. 102. Rastogi R, Saksena S, Garg NK, et al. Picroliv protects against alcohol-induced chronic hepatotoxicity in rats. Planta Med. 1996 Jun;62(3):283-5. 103. Visen PK, Saraswat B, Dhawan BN. Curative effect of picroliv on primary cultured rat hepatocytes against different hepatotoxins: an in vitro study. J Pharmacol Toxicol Methods. 1998 Oct;40(3):173-9. 104. Seth P, Sundar SV, Seth RK, et al. Picroliv modulates antioxidant status and down-regulates AP1 transcription factor after hemorrhage and resuscitation. Shock. 2003 Feb;19(2):169-75. 105. Bradamante S, Barenghi L, Villa A. Cardiovascular protective effects of resveratrol. Cardiovasc Drug Rev. 2004;22(3):169-88. 106. de la Lastra CA, Villegas I. Resveratrol as an anti-inflammatory and anti-aging agent: mechanisms and clinical implications. Mol Nutr Food Res. 2005 May;49(5):405-30. 107. Jang M, Cai L, Udeani GO, et al. Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science. 1997 Jan 10;275(5297):218-20. 108. Markham KR, Mitchell KA. The mis-identification of the major antioxidant flavonoids in young barley (Hordeum vulgare) leaves. Z Naturforsch [C]. 2003 Jan;58(1-2):53-6. 109. Arimoto T, Ichinose T, Yoshikawa T, Shibamoto T. Effect of the natural antioxidant 2”-O-glycosylisovitexin on superoxide and hydroxyl radical generation. Food Chem Toxicol. 2000 Sep;38(9):849-52. 110. Yu YM, Wu CH, Tseng YH, Tsai CE, Chang WC. Antioxidative and hypolipidemic effects of barley leaf essence in a rabbit model of atherosclerosis. Jpn J Pharmacol. 2002 Jun;89(2):142-8. 111. Yu YM, Chang WC, Chang CT, Hsieh CL, Tsai CE. Effects of young barley leaf extract and antioxidative vitamins on LDL oxidation and free radical scavenging activities in type 2 diabetes. Diabetes Metab. 2002 Apr;28(2):107-14. |