Life Extension Magazine®
| LE Magazine May 2004 | ||||||||||
| The Role of Nutrition in Macular Degeneration By Dennis L. Gierhard, PhD | ||||||||||
|
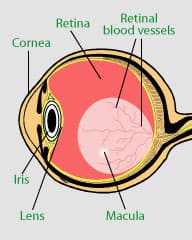
Macular degeneration is the leading cause of blindness in people over the age of 55, affecting more than 10 million Americans. The disease occurs when the central portion of the retina (the macula) deteriorates, resulting in impaired vision or blindness. The good news is that leading researchers have identified specific dietary factors that can prevent, and even partially reverse, this devastating ocular disorder. Zeaxanthin is one of 700 plant pigments called carotenoids that provide much of the color in nature and our diet. The carotenoids derive their name from the fact that the first pigment isolated, beta-carotene, was from carrots. Beta-carotene is an important source of vitamin A, which is critical to vision. Zeaxanthin and its closely related cousin, lutein, are called xanthophylls and are perhaps the third to seventh most prevalent carotenoids in the human diet (depending on fruit and vegetable selection).1,2 Humans cannot synthesize these carotenoids and thus must obtain them from their diet. Zeaxanthin and lutein have been recently called “conditionally essential nutrients” because of their critical protective functions in the eye.3 Guarding Against Light Damage While plants use zeaxanthin to safely harvest light, they more importantly use zeaxanthin to protect against harmful light levels. Dark green leafy vegetables contain large amounts of both pigments but have much more lutein compared to zeaxanthin. Zeaxanthin is more predominant in many of the yellow, orange, and red fruits and vegetables such as peppers, corn, and peaches.1-6 Both lutein and zeaxanthin absorb the very high-energy and most damaging portions of the light spectrum (ultraviolet blue). This absorption of the high-energy spectrum is critical to the protection of the lens, retina, and macular portions of the eye.1,5,7
Protecting Against Free Radicals Like other carotenoids, zeaxanthin is absorbed like a fat and its absorption is aided by the presence of fats in the accompanying meal. Because the bioavailability of carotenoids can be very poor, it is very important that the dietary supplements you consume have proven bioavailability (some sources may be as low as 5% bioavailable for these pigments).8 Zeaxanthin and lutein are transported from the intestine to the liver, where they are packaged for transport on the surface of blood lipoproteins to various body tissues such as the eye. There is good evidence that the xanthophylls protect lipoproteins—such as low-density lipoprotein (LDL)—and may reduce the earliest steps of atherosclerosis via their antioxidant and anti-inflammatory mechanisms.10-12 The xanthophylls are concentrated in the adrenal, prostate, and breast glands and in the kidneys. The largest total quantities are stored in the liver and adipose (or fat) tissues. The xanthophylls’ propensity to store in fat means that individuals who are obese or have a high body mass index (BMI) may have lower deposition of the xanthophylls in eye tissues and greater risk of degenerative eye disease. Both animal and human trial data suggest that lutein is affected more by this competition with fatty tissues, which may explain why in obese individuals zeaxanthin shows much greater ability to deposit in the eye than lutein.16 Other health benefits attributable to both zea-xanthin and lutein are supported by data from laboratory, animal, and epidemiological studies, as shown below. Discovering Lutein and Zeaxanthin in the Eye These two xanthophylls are found in almost all subsections of the eye,18,19 but occur in concentrations nearly 1,000 times greater in the macula section of the retina than in any other tissue in the body.4 This extremely high concentration creates a yellow spot that is visible to the trained professional and is called the “macula lutea.” The xanthophylls that give the macula its striking color also are often referred to as the “macular pigments.” The American biochemist Dr. George Wald was the first to connect the xanthophylls with eye health in 1945 when he tentatively identified the macular pigment as lutein. (Dr. Wald later won a Nobel Prize for his research on the role of vitamin A in vision.23,24) The modern era was initiated in 1985 when two Miami-based researchers, Bone and Landrum, determined that the macular pigment was actually two compounds, lutein and zeaxanthin.17 This group, along with others, demonstrated that zeaxanthin was concentrated in the center of the retina, while lutein was more prominent at the edges.18,19,20 In 1994, DSHEA legislation was passed and a group headed by Dr. Seddon at Harvard Medical School published epidemiological data that strongly suggested that people who consume fruits and vegetables containing zeaxanthin and lutein have reduced risks of advanced macular degeneration, the leading cause of acquired blindness in the elderly.22 In 1997, a group at Tufts identified the same two pigments in the lens of the human eye in nearly equal proportions; at about the same time, epidemiological studies linked the same two pigments with reduced risk of cataract incidence, progression, and severity.25-31,32
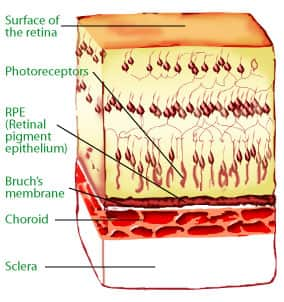
Macular Degeneration Macular degeneration is the leading cause of acquired blindness and vision impairment among elderly Americans. It is estimated that up to 17 million elderly Americans have at least early signs of the disease called age-related maculopathy. The National Eye Institute estimates that nearly 1.7 million elderly Americans have the more advanced stage of macular degeneration, and a new case is diagnosed every three minutes. The prevalence of the disease increases with age, affecting one in six Americans aged 55 to 64 and one in three Americans over 75. Of the 1.7 million currently afflicted, nearly 85% have the most prevalent form of the disease, known as dry macular degeneration.2,33,34 Patients who are affected suffer a gradual loss of central vision due to the death of photoreceptor cells (rods and cones) and their close associates, retinal pigmented epithelium cells. Photoreceptors are the cells in the retina that actually “see” light and are essential for vision. Retinal pigmented epithelium cells are like the “nursemaids” for photoreceptor cells and are necessary for photoreceptor survival. The death of either of these cell types leads to the death of the other. The macula contains the highest concentration of cone-type photoreceptors that are responsible for providing color and fine detail in the center of the visual field. Thus, patients with macular degeneration gradually lose their central vision and with it, the ability to drive, read, and see the faces of loved ones. As bad as this may be, those suffering the disease can function at a reasonable level for many years. However, another aspect of macular degeneration is even more devastating. As the photoreceptor and retinal pigmented epithelium cells slowly degenerate, blood vessels tend to grow from their normal location in the choroid into an abnormal location beneath the retina. This abnormal new blood vessel growth is called choroidal neovascularization, or wet macular degeneration. Abnormal blood vessels leak and bleed, resulting in sudden and severe loss of central vision. Depending on the location, laser treatment can sometimes be given to destroy the blood vessels. When retinal cells are lost, they are not replaced and central vision loss can be profound. New drugs are currently under development for wet macular degeneration, but their availability may be years away.
Protecting the Lens and Macula Within the retina, a significant portion of the xanthophylls reside in Henle’s fiber, a layer of axons in the inner retinal layer where xanthophylls can filter light prior to light striking photoreceptors (rods and cones) and the very important retinal pigmented epithelium cells. This location would suggest a very strong role for the xanthophylls in filtering damaging light, particularly the most damaging blue part of the spectrum. The exact center of the macula is where the highest concentrations of dietary zeaxanthin and a related isomer, meso-zeaxanthin, are found. In the peripheral retina, lutein dominates.18-21 Current theory suggests that high macular pigment, particularly dietary zea-xanthin, protects the portion of the macula most critical to vision and most exposed to photo-oxidative damage.35 Very high metabolic rates found in the fovea (the center of the macula) require extra antioxidant protection.7 Macular degeneration pathology often starts at the edges of the macula, where macular pigment concentrations start to decrease. Analyses of cadaver eyes have shown this direct link by contrasting macular pigment concentrations at distances from the macula’s center in eyes with macular degeneration with those in normal matched eyes.37 These experiments found a significant drop in pigment concentrations in eyes with macular degeneration compared to normal matched eyes, a difference corresponding to the relative concentrations of zeaxanthin in the eyes. To summarize, the eye concentrates just three xanthophylls—dietary zeaxanthin, non-dietary meso-zeaxanthin, and lutein—in the macula and other ocular tissues. Of the 16-20 carotenoids in the blood serum, only two are selected for deposition and hyper-concentration in the eye. This highly selective process is the most specific distribution in the entire field of carotenoid biochemistry.18-21,38 | ||||||||||
| LE Magazine May 2004 | |||||||
| The Role of Nutrition in Macular Degeneration By Dennis L. Gierhard, PhD | |||||||
How Many Xanthophylls Do We Need? Several major epidemiological studies have linked dietary carotenoid consumption with reduced risks of macular degeneration and cataract. The dietary gap between low-and high-risk individuals was equivalent to about 6 mg/day of lutein and zeaxanthin.22,25,29-32,39 The data suggest that a difference of 4-5 mg/day in consumption of xanthophylls could influence the risks of contracting eye disease and may be a basis for a maintenance or preventive dosage. For low-risk individuals, perhaps 3-6 mg/day of zeaxanthin may be extrapolated as a preventive dosage for degenerative eye diseases, though a dose as low as 0.5 mg/day over an entire lifetime may be sufficient. A number of other clinical trials are using 20-30 mg/day of zeaxanthin. Differences Between Zeaxanthin and Lutein A misconception among consumers is that they get enough dietary zeaxanthin from their lutein products. A second misconception, even among eye specialists, is that lutein is converted to zeaxanthin in the eye. In fact, lutein comes from marigold flowers and contains only a tiny amount of zeaxanthin compared to the 2:1 ratio seen in the section of the macula that seems to be protected. A second fact is that lutein is converted into a compromise structure, meso-zeaxanthin, in the eye. Zeaxanthin’s Protective Effects Against Eye Disease With trials in Japanese quail and primates, the evidence from animal trials has recently become much stronger. In the early 1980s, researchers depleted primate diets of carotenoids and demonstrated retinal pathologies consistent with symptoms of macular degeneration. The studies were extended in the mid-1990s when Dr. C.K. Dorey and colleagues at Harvard Medical School and the Schepens Eye Institute established the Japanese quail as a model for studying degenerative eye disease and xanthophylls.16,44-46 Using aging and light-insult models, Dr. Dorey was the first to show directly that the photo-protective effects of zeaxanthin were related to the retinal levels of zeaxanthin that she controlled by feeding. This retinal protection extended to both rods and cones, and prevented the massive losses seen in late-stage dry macular degeneration. The team also went on to show that zeaxanthin:
Further results with primates have shown that zeaxanthin is more photo-protective (blue laser light insult) than lutein or meso-zeaxanthin. Increasing the Macular Pigment’s Thickness Doctors can now measure “macular pigment optical density” indirectly and noninvasively by at least six different techniques, though some of these techniques have been subject to criticism. The human trials that measured macular pigment optical density in response to lutein and zeaxanthin intake are summarized in the next column:
The association between macular pigment optical density and risk factors for macular degeneration and cataracts is compelling. Reduced macular pigment optical density in the target population has been related to smoking, obesity/high BMI, age, lens density and opacity, gender, light iris, and poor zeaxanthin intake.1,2,4,7,9,47-51
Zeaxanthin and Other Eye Diseases The results to date are promising, but larger and longer clinical trials will be necessary to clarify the benefits for patients and eye-care professionals before zeaxanthin supplements will receive an unqualified recommendation. The FDA will need to see statistically relevant data, and the medical community will need to see these functional improvements along with reduced progression of symptoms like area of atrophy, drusen and lipofuscin progression, and reduced risk of neo-vascularization or its progression. Major trials on intervention in all stages of macular degeneration are in various stages of planning and execution. The largest of these may be the AREDSII trial, with more than 5,000 patients in late-stage macular degeneration. The National Eye Institute and National Institutes of Health are scheduled to begin this trial using lutein and zeaxanthin later this year. Zeaxanthin and lutein were not commercially available for the first trial. Finally, since zeaxanthin supplements were introduced, many patients who were hypersensitive to light (i.e., photophobic) are reporting dramatic decreases in this unpleasant phenomenon within months of initiating 20 mg/day doses of zeaxanthin. These observations are now being assessed objectively at two colleges of optometry. Dual Mechanisms of Action Both lutein and zeaxanthin are capable of quenching free-radical reactions that create reactive oxygen species. These reactive oxygen species then react with cell membranes and macromolecules to create pathogenesis leading to many human degenerative conditions. In the eye tissues, these oxidative processes can be further enhanced by the presence of light (which accelerates photo-oxidation), extremely high metabolic rates (in the retina), and the highly polyunsaturated lipids found in the retina and other neural tissues. Both singlet oxygen and peroxyl radicals are likely generated in eye tissues and quenched by the xanthophylls. Light-driven photo-oxidation likely generates excited triplet-state species that also cause severe oxidative damage. As noted earlier, zeaxanthin is a better antioxidant and is more directly embedded in a manner to protect biological cell membranes than is lutein. Xanthophylls are particularly effective at lower oxygen tensions (concentrations) like the interior of a cell membrane or the center of lens tissue. The tocopherols are more effective at higher oxygen tensions. Thus it is highly likely the two lipophilic antioxidants are synergistic and complement ascorbates and the metal-containing enzyme-based antioxidant enzymes that are active in ocular tissues for protection against oxidative damage. The very earliest steps in eye cells showing oxidative stress are the generation of lipoperoxides.56 In 2000, these very early oxidation markers were shown to directly induce the pathways of angiogenesis or neovasularization.57,58 This means that the earliest step of oxidation may be capable of increasing the risk of progressing to wet macular degeneration. The second biologically plausible mechanism is UV and blue-light filtering or absorption. The xanthophylls are excellent light filters and absorb that part of the UV and blue-light spectrum thought to be most damaging to the eye. In the lens, the xanthophylls absorb the UV light thought to be the principal initiator of oxidative stress that results in cross-linking of the component crystalline that in turn reduces the clearness of the lens. The xanthophylls would also reduce the amount of blue light reaching the retina. The absorption of blue light in the lens and from reflection in the retina would reduce light scatter and chromatic aberrations. This would suggest a more direct role in reducing visual effects like glare and starburst effects seen in early stages of these diseases.7 This blue-light filtering may directly reduce the photo-oxidation in the susceptible axons and likely reduces photo-oxidative damage directly in the photoreceptors and posterior retinal pigmented epithelium cells that support and maintain the photoreceptors. In the critically important retinal pigmented epithelium cells insulted with blue light, zeaxanthin has been shown to prevent oxidative damage, apoptosis, DNA damage, and cell death. In these cell culture experiments, zeaxanthin shows synergy with the other cellular protectants vitamins C and E, glutathione, and melanin.60 Theories of Aging Explain Degenerative Eye Disease These two disparate and opposing functions are within an inch of each other inside the eye. Readers should also know that caloric restriction, the almost universal environmental anti-aging influence, has also been shown to slow degeneration or aging of the eye. In addition to its role in the photo-oxidative mechanism of degenerative eye disease, it is likely that zeaxanthin also participates through other protective biological mechanisms. Because age-related eye degeneration is probably multi-etiological, it is likely zeaxanthin helps provide protection at multiple levels.1,4,7,35 | |||||||
| LE Magazine May 2004 |
| The Role of Nutrition in Macular Degeneration By Dennis L. Gierhard, PhD |
| Summary and Prediction A plausible theory is put forward to support others’ speculation that zeaxanthin may be a “critically essential nutrient” for proper eye function and protection.3 This theory suggests a need to change behaviors and increase dietary consumption of fruits and vegetables to decrease age-related degeneration of the eye. Some evidence suggests it may be more difficult to obtain higher levels of zeaxanthin from the diet than of lutein, indicating that supplementation may be desirable. There is good evidence that zeaxanthin is preferred by ocular tissues because it has unique properties and subtle structural differences compared to lutein that make it a better lipophilic antioxidant and photoprotectant. Dietary supplementation with 3-6 mg/day of zeaxanthin may reduce the risk of contracting degenerative eye diseases. Significantly higher dietary intake of zeaxanthin (not the isomer meso-zeaxanthin) may be important for individuals with high risks for or advanced symptoms of macular degeneration and cataracts. Other health benefits associated with zeaxanthin also have been noted. In the near future, we can expect more basic research, animal studies, and objective double-blind clinical trials attempting to clearly define zeaxanthin’s importance in degenerative eye diseases. It is likely that high intake of dietary antioxidants and zeaxanthin will be shown to be a factor in reducing the risk and slowing the progression of degenerative eye diseases. Other important phytonutrients are also likely to act synergistically with zeaxanthin in slowing the aging effects in the eye. As science elucidates the most important degenerative mechanisms and genetics shines its light on inheritance issues and mechanisms, supplements will be on the market to address these needs. Looking out a little further in the future, it is likely that cataract prevalence and progression will benefit from combined research on zeaxanthin and advances in the nutritional biochemistry of the eye.33 This advance could have a positive economic impact on growing Medicare expenditures tied to degenerative eye disease. Perhaps the same impact will be seen concerning diabetic complications of the eye and macular degeneration. With nearly 15 million dry macular degeneration sufferers in the US today and more on the way, a decreased incidence and progression rate would be welcome. Pharmaceutical and biotechnology companies are developing cold laser and angiogenesis inhibitors for treating the ravaging effects of wet macular degeneration.35 Almost all these treatments target single molecules or single pathways to prevent or destroy unwanted blood vessels. While zeaxanthin may be the single most critical nutrient for the eye, its value will most likely be in conjunction with high dietary intake of multiple nutrients. Eventually there will be a convergence of nutritional intervention (to prevent and modulate early insults and stresses of the eye) and sophisticated medical treatments (for very late and aggressive blood vessel growth of wet macular degeneration). Future generations will be able to see those important things in life. In the meantime, you can eat healthy (lots of fruits and vegetables, decreased fats, and increased fish oil), increase your dietary intake of zeaxanthin and other antioxidants, stop smoking, lose those extra pounds, watch your risk factors for cardiovascular disease, and protect your eyes when in the sun. About the Author |
| References |
| 1. Schalch W. Possible contribution of lutein and zeaxanthin, carotenoids of the macula lutea, to reducing the risk for age-related macular degeneration: a review. HKJ Ophthalmol. 4(1). 2. Seddon JM. Nutrition and age-related eye disease. VNIS Backgrounder. 3(1). 3. Semba RD, Dagnelie G. Are lutein and zeaxanthin conditionally essential nutrients for eye health? Med Hypotheses. 2003 Oct;61(4):165-72. 4. Krinsky NI, Landrum JT, Bone RA. Biologic mechanisms of the protective role of lutein and zeaxanthin in the eye. Annu Rev Nutr. 2003:23:171-201. 5. Krinsky NI. Possible biologic mechanisms for a protective role of xanthophylls. J Nutr. 2002 Mar;132(3):540S–542S. 6. Roche NDI. Available at: http://www.fda.gov/ ohrms/dockets/dockets/95s0316/rpt0096_01.pdf. Accessed February 27, 2004. 7. Snodderly DM. Evidence for protection against age-related macular degeneration by carotenoids and antioxidant vitamins. Am J Clin Nutr. 1995 Dec;62(6suppl): 1448S–1461S. 8. Zaripheh S, Erdman JW Jr. Factors that influence the bioavailability of xanthophylls. J Nutr 2002 Mar;132(2):531S-534S. 9. Mares-Perlman JA, Millen AE, Ficek TL, Hankinson SE. The body of evidence to sup- port a protective role for lutein and zeaxan- thin in delaying chronic disease. Overview. J Nutr. 2002 Mar;132(3):518-524S. 10. Ford ES, Liu S, Mannino DM, Giles WH, Smith SJ. C-reactive protein concentration and concentrations of blood vitamins, carotenoids, and selenium among United States adults. Eur J Clin Nutr. 2003 Sept;57(9)1157-63. 11. Suzuki K, Ito Y, Ochiai J, et al. Relationship between obesity and serum markers of oxidative stress and inflamma- tion in Japanese. Asian Pac J Cancer Prev. 2003 Jul-Sep;4(3):259-66. 12. Granado F, Olmedillo B, Blanco I. Nutritional and clinical relevance of lutein in human health. Br J Nutr. 2003 Sep; 90(3):487-502. 13. Nishino H. Murakosh M Li T, et al. Carotenoids in cancer chemoprevention. Cancer Metastasis Rev. 2002;21(3-4):257-64. 14. Chew BP, Park JS. Carotenoid action on the immune response. J Nutr. 2004 Jan;134(1):257S-261S. 15. Gonzalez S, Astner S, An W, Goukassian D, Pathak MA. Dietary lutein/zeaxanthin decreases ultraviolet B-induced epidermal hyperproliferation and acute inflammation in hairless mice. J Invest Dermatol. 2003 Aug;121(2)399-405. 16. Toyoda Y, Thomson L, Langner A, et al. Effect of dietary zeaxanthin on tissue distri- bution of zeaxanthin and lutein in quail. IOVS. 2002 Apr;43(4):1210-21. 17. Bone RA, Landrum JT, Tarsis SL. Preliminary identification of the human macular pigment. Vision Res. 1985;25(1):1531–5. 18. Bernstein PS, Khachik F, Carvalho LS, Muir GJ, Zhao DY, Katz NB. Identification and quantitation of carotenoids and their metabolites in the tissues of the human eye. Exp Eye Res. 2001 Mar;72(3):215–23. 19. Handelman GJ, Dratz EA, Reay CC, Van Kuijk JG. Carotenoids in the human macula and whole retina. Investig Ophthalmol Vis Sci. 1988 Jun;29:850–5. 20. Bone RA, Landrum JT, Fernandez L, Tarsis SL. Analysis of macular pigment by HPLC: retinal distribution and age study. Invest Ophthalmol Vis Sci. 1988;29(6):843–9. 21. Bone RA, Landrum J, Hime GW, Cains A, Zamor J. Stereochemistry of the human macular carotenoids. IOVS. 1993 May:34(6):2003-40. 22. Seddon JM, Ajani UA, Sperduto RD, et al. Dietary carotenoids, vitamins A, C and E and advanced age-related macular degenera- tion. JAMA. 1994 Nov 9;272(8):1413-20. 23. Wald G. Human vision and the spectrum. Science. 1945;101:653–658. 24. Nussbaum JJ, Pruett RC, Delori F. Historic perspectives: macular yellow pigment. The first 200 years. Retina. 1981 Oct- Dec;1(4):296-310. 25. Yeum KJ, Taylor A, Tang G, Russell RM. Measurement of carotenoids, retinoids, and tocopherols in human lenses. Investig Ophthalmol Vis Sci. 1995 Dec;36(13):2756–61. 26. Lyle BJ, Mares-Perlman JA, Klein BEK, Klein R, Greger JL. Antioxidant intake and risk of incident age-related nuclear cataracts in the Beaver Dam Eye Study. Am J Epidemiol. 1999 May 1;149(1):801–9. 27. Lyle BJ, Mares-Perlman JA, Klein BE, et al. Serum carotenoids and tocopherols and inci- dence of age-related nuclear cataract. Am J Clin Nutr. 1999 Feb;69(2):272–7. 28. Mares-Perlman JA, Lyle BJ, Klein R, et al.Vitamin supplement use and incident cataracts in a population-based study. Arch Ophthalmol. 2000 Nov;118(11):1556-63. 29. Chasan-Taber L, Willett WC, Seddon JM, et al. A prospective study of carotenoid and vitamin A intakes and risk of cataract extrac- tion in US women. Am. J. Clin. Nutr. 1999 Oct;70(4):509–16. 30. Brown L, Rimm EB, Seddon JM, et al. A prospective study of carotenoid intake and risk of cataract extraction in U.S. Men. Am. J. Clin. Nutr. 1999 Oct;70(4):517–24. 31. Jacques PF, Chylack LT Jr, Hankinson SE, et al. Long-term nutrient intake and early age-related nuclear lens opacities. Arch Ophthalmol. 2001 Jul;119(7):1009-19. 32. Berendschot TT, Broekmans WM, Klopping-Ketelaars IA, Kardinaal AF, Van Poppel G, Van Norren D. Lens aging in relation to nutritional determinants and possible risk factors for age-related cataract. Arch Ophthalmol. 2002 Dec;120(12):1732-7. 33. Taylor A. Nutritional and Environmental Influences on the Eye. Boca Raton, FL: CRC Press; 1999:215-50. 34. National Eye Institute. Available at: http://www.nei.nih.gov/. Accessed February 27, 2004. 35. Sun H, Nathans J. The challenge of macular degeneration. Sci Am. 2001Oct;285(4):68-75. 36. Weiter JJ, Delori F, Dorey CK. Central spar- ing in annular macular degeneration. Am J Ophthalmol. 1988 Sep 15;106(3):286–92. 37. Bone RA, Landrum JT, Mayne ST, Gomez CM, Tibor SE, Twaroska EE. Macular pig- ment in donor eyes with and without AMD: a case-control study. Invest Ophthalmol Vis Sci. 2001 Jan;42(1):235–40. 38. Schalch W, Dayhaw-Barker P, Barker FM II. The carotenoids of the human retina. In: Nutritional and Environmental Influences on the Eye. Boca Raton, FL: CRC Press; 1999. 39. Mares-Perlman JA, Fisher AI, Klein R, et al. Lutein and zeaxanthin in the diet and serum and their relation to age-related mac- ulopathy in the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2001;153:424–432 40. AREDS Research Group. The Age-related Eye Disease Study (AREDS): A Randomized placebo-controlled clinical trial of high-dose supplementation with vitamins C and E, beta carotene and zinc for age-related macular degeneration and vision loss. AREDS Report #8. Arch Ophthalmol. 2001 Oct;119(10):1417-36. 41. Gale CR, Hall NF, Phillips DI, Martyn CN. Lutein and zeaxanthin status and risk of age-related macular degeneration. Invest Opthalmol Vis Sci. 2003 Jun;44(6):2461-5. 42. Sujak A, Gabrielska J, Grudzinski W, Borc R, Mazurek P, Gruszecki WI. Lutein and zeaxanthin as protectors of lipid mem- branes against oxidative damage: the struc- tural aspects. Arch Biochem Biophys. 1999 Nov 15;371(2):301–7. 43. Craft N, Haitema T, Garnett K, Fitch K, Dorey K. Carotenoid, tocopherol, and retinol concentrations in elderly human brain. J Nutr Health and Aging. 2004 (in press). 44. Thomson L, Toyoda Y, Langner A, et al. Elevated retinal zeaxanthin and prevention of light-induced photoreceptor cell death in quail. IOVS. 2002 Nov;43(11):3535-49. 45. Thomson L, Toyoda Y, Delori F, et al. Long term dietary supplementation with zeaxan thin reduces photoreceptor death in light-damaged Japanese quail. Exp Eye Res. 2002 Nov;75(5):529-42. 46. Dorey CK, Cheng KM, Gierhart DL, Craft NE. Dietary manipulation of lens zeaxan- thin in quail. ARVO. 2003;abstract #207/B182. 47. Hammond BR Jr, Johnson EJ, Russell RM, et al. Dietary modification of human macu- lar pigment density. Investig Ophthalmol Vis Sci. 1997 Aug;38(9):1795–801. 48. Garnett KM, Guerra LH, Lamb JD, et al. Serum and macular pigment responses to supplementation with lutein or zeaxanthin. Assoc Res Vis Ophthalmol. 2002;43:2820(abs). 49. Bone RA, Landrum JT, Guerra LH, Ruiz CA. Lutein and zeaxanthin dietary supple- ments raise macular pigment density and serum concentrations of these carotenoids in humans. J Nutr. 2003 Apr;133(4):992-8. 50. Johnson EJ, Hammond BR, Yeum KJ, et al. Relation among serum and tissue concentra- tions of lutein and zeaxanthin and macular pigment density. Am J Clin Nutr. 2000 Jun;71(6):1555–62. 51. Rock CL, Thornquist MD, Neuhouser ML, et al. Diet and lifestyle correlates of lutein in the blood and diet. J Nutr. 2002 Mar;132(3):525S–530S. 52. Olmedilla B, Granado F, Blanco I, Vaquero M, Cajigal C. Lutein in patients with cataracts and age-related macular degenera- tion: a long-term supplementation study. J Sci Food Agric. 2001;81:904–9. 53. Massacesi AL, et al. The effect of oral sup- plementation of macular carotenoids on the prevention of AMD. ARVO 2001;abstract #1261. 54. Olmedilla B, Granado F, Blanco I, Vaquero M. Lutein but not alpha tocopherol supple- mentation improves visual function in patients with age-related cataracts. Nutrition. 2003 Jan;19(1):21-24. 55. Richer SP et al. The lutein antioxidant sup- plementation trial. ARVO 2002;mtg abst #2542. 56. Beatty S, Koh H, Phil M, Henson D, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Opthalmol. 2000 Sep- Oct;45(2):115-34. 57. Ueda T, Ueda T, Fukuda S, et al. Lipid hydroperoxide-induced tumor necrosis fac- tor (tnf) – alpha vascular endothelial growth factor and neovacularization in the rabbit cornea: effect of TNF inhibition. Angiogenesis. 1988;1(2):174-184. 58. Armstrong D, Ueda T, Ueda T, et al. Lipid hydroperoxide stimulates retinal neovascu- larization in rabbit retina through expression of tumor necrosis factor – alpha vascular endothelial growth factor and platelet-derived growth factor. Angiogensesis. 1988;2(1):93-104. 59. Davies NP, Morland AB. Color matching in diabetes: optical density of the crystalline lens and macular pigments. Investig Ophthamol Vis Sci. 2002 Jan; 43(1) 281-9. 60. Nilsson SE, Sundelin SP, Wihlmark U, Brunk UT. Aging of cultured retinal pig- ment epithelial cells: oxidative reactions, lipofuscin formation and blue light damage. Doc Opthalmol. 2003 Jan;106(1):13-6. 61. Khachik F, Bernstein PS, Garland DL. Identification of lutein and zeaxanthin oxidation products in human and monkey retinas. Investing Ophthalmol Vis Sci. 1997 Aug;38(9):1802–11. |