Life Extension Magazine®
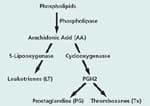
Pharmaceutical companies proclaimed a new era in arthritis management with the advent of the COX-2 inhibitors such as Celebrex® and Vioxx®. Unfortunately, these drugs work against themselves by upsetting the system of checks and balances through which the body regulates inflammation. A brief review of arthritis and the biochemical pathways leading to inflammation will help us understand the fly in this ointment—and what we can do about it. Aging and arthritis seem to go hand in hand. Arthritis is not a single disease, but rather a host of conditions that adversely affect the joints. Osteoarthritis is the most common form, affecting approximately 70% to 80% of the population over age 50. The onset is marked by morning stiffness, crackling joints and perhaps some pain. As it gets worse, it causes discomfort, pain and disability in varying degrees for millions of people. New research is beginning to shed light on how osteoarthritis develops at the cellular and molecular levels. Evidence is accumulating that the culprits are proinflammatory cytokines, together with the enzymes that generate inflammatory mediators and break down the collagen matrix. Cytokines are proteins that carry messages between cells and regulate immunity and inflammation. Two cytokines, tumor necrosis factor alpha (TNF-alpha) and interleukin one beta (IL-1 beta), play an essential role in the cartilage destruction and inflammation process.[1] They have been found in elevated levels in the synovial membrane, the synovial fluid and the cartilage of osteoarthritis patients. In animal models, it was shown that inhibition of TNF-alpha results in decreased inflammation, while inhibition of IL-1 beta effectively prevents cartilage destruction.[2] TNF-alpha has proven to be even more important in rheumatoid arthritis, where it is a key factor in promoting inflammation and damage to cartilage and bone.[3,4] Arthritis is almost certainly more common today than it was among our prehistoric ancestors. Its prevalence is most likely due to two facts of modern life: we live longer today and more of us are obese than ever before. However, effective treatments are now available that combine up-to-the-minute pharmacological advances with ancient herbal remedies. These remedies not only provide symptomatic pain relief, but also reverse the degenerative process itself. Inflammatory Pathways The rub is that inhibition of COX-2 is thought to lead to an imbalance between two key inflammatory mediators, raising levels of thromboxane A2 relative to prostaglandin E2. This in turn increases production of the above mentioned proinflammatory signaling molecules, the cytokines TNF- alpha (tumor necrosis factor alpha) and IL-1b (interleukin-1 beta).[5] In addition, there is evidence that elevated thromboxane A2 raises levels of an important inflammatory mediator in the LOX (lipoxygenase) pathway, leukotriene B4.[6] Thus COX-2 inhibition may help perpetuate the underlying degenerative process while relieving its superficial symptoms. As the scientists who made this discovery put it, “the short-term effects of (COX-2 inhibitors) on the pain and swelling of inflammation and arthritis may be achieved at the cost of an increased propensity to long-term tissue damage with which these cytokines have been associated.”[5] Another prominent researcher writes, “Tumor necrosis factor (TNF) and interleukin-1 (IL-1) are considered to be master cytokines in chronic, destructive arthritis.”[7] Their destructive roles overlap, however. In rheumatoid arthritis, TNF-alpha figures more prominently in triggering inflammation both locally and systemically, while IL-1 beta is more involved in destruction of cartilage and bone, and in impeding the repair of cartilage.[8] This research points up the importance of inhibiting TNF-alpha, IL-1 beta, and the LOX pathway when using a COX-2 inhibitor. Nettle Leaf Extract Nettle “may inhibit the inflammatory cascade in autoimmune diseases and rheumatoid arthritis,” concluded a team of researchers.[10] It is interesting to note that the prescription drug Enbrel®, approved for the treatment of rheumatoid arthritis, acts by suppressing TNF-alpha. One of the ways nettle leaf extract blocks proinflammatory signaling is by inhibiting the genetic transcription factor that activates TNF-alpha and IL-1 beta in synovial tissue.[11] This proinflammatory transcription factor, known as nuclear factor kappa beta (NF-kb), is elevated in chronic inflammatory diseases and is essential to activation of TNF-alpha. Nettle is thought to work by preventing degradation of the natural inhibitor of NF-kb in the body. TNF-alpha also activates NF-kb in synovial cells, leading to the suggestion that a cycle of cross-activation between TNF-alpha and NF-kb may sustain and amplify the disease process in rheumatoid arthritis.[12] A recent laboratory experiment revealed one of the mechanisms by which nettle leaf extract protects joints. Inflammatory joint diseases are characterized by breakdown of the extracellular matrix (ECM), which surrounds and supports cells. In arthritis, TNF-alpha and especially IL-1 beta stimulate enzymes known as matrix metalloproteinases (MMP’s) that break down the extracellular matrix. The experiment measured MMP levels of chondrocytes (joint cells) exposed to IL-1 beta. Nettle leaf extract was found to significantly inhibit all the matrix metalloproteinases tested (MMP-1, -3 and -9).[13] Another study conducted on 40 patients suffering from acute arthritis compared the effects of 200 mg of the nonsteroidal anti-inflammatory drug (NSAID) diclofenac with 50 mg of the NSAID in combination with 50 g of stewed nettle leaf per day.[14] Total joint scores improved significantly in both groups by approximately 70%. The nettle leaf extract clearly enhanced the anti-inflammatory effect of the NSAID. The addition of nettle extract made possible a 75% dose reduction of the NSAID, while still retaining the same anti-inflammatory effect with reduced side effects. Nettle leaf extract thus makes the ideal complement to COX-2 inhibitors, by virtue of its ability to counteract their negative effects. The herbal COX-2 inhibitor Nexrutine® is derived from the bark of the phellodendron tree, which folk healers use to treat arthritis and other ailments. Prescription COX-2 inhibitors intervene in the inflammation cascade by blocking the action of the COX-2 enzyme. But Nexrutine® inhibits the gene expression of COX-2, preventing its manufacture in the first place. This difference in mechanism of action may account for the rapidity of Nexrutine®’s inflammation-quenching action. According to reports from subjects who used Nexrutine® for two weeks, 79% agreed that Nexrutine® helped relieve or avoid the general aches and pains associated with overexertion and physical activity. No side effects were reported at recommended dosages.[15] |