Life Extension Magazine®

Why do elderly people contract so many diseases at the same time? One answer is that certain destructive cytokines (immune modulating agents) increase with aging. The good news is that there are drug and nutrient therapies available to suppress these dangerous cytokines and alleviate a host of degenerative diseases.
One nasty cytokine that increases as humans age is called tumor necrosis factor (TNF-a). Too much TNF-a results in a host of aging-related disorders including autoimmune disease, congestive heart failure, insulin resistance and catabolic wasting. When TNF-a attacks the linings of the joints, the result is inflammation, pain and eventual immobility. TNF-a and other cytokines have been implicated in both rheumatoid and osteoarthritis. Suppressing TNF-a, therefore, appears to be an effective method of treating a wide variety of aging-related diseases.
The most effective therapy to treat rheumatoid arthritis is a FDA-approved prescription drug called Enbrel. This drug (Enbrel) works by suppressing the destructive cytokine TNF-a.
By suppressing TNF-a, Enbrel often reverses the course of rheumatoid arthritis. The drug is relatively safe with the primary side effect being injection site reactions. Since TNF-a is needed to fight acute infectious disease, when one has a serious infection, Enbrel therapy is temporarily discontinued until the infection subsides.
So why don't you hear more about Enbrel? First of all, it costs about $12,000.00 a year and requires two visits every week to your doctor's office for the injections. Many HMOs insist that arthritis patients use less costly COX-2 inhibiting drugs like Celebrex or Vioxx in lieu of the more expensive Enbrel. The COX-2 inhibiting drugs, however, are not as effective as the Enbrel.
While Enbrel is only approved by the FDA for rheumatoid arthritis, it may also be effective in protecting against the cartilage destruction that occurs in osteoarthritis. Both TNF-a and another cytokine called interleuken one beta (IL-1b) have been shown to play a role in the cartilage destruction and inflammatory process1 characteristic of osteoarthritis. Even if one has insurance that would pay for Enbrel, it would still require a diagnosis of rheumatoid arthritis for the insurance company to pay for Enbrel. This means that those with osteoarthritis face the prospect of both having to pay the $12,000.00 yearly cost out-of-pocket, and locate a doctor willing to prescribe Enbrel for an unapproved use, i.e. treatment of osteoarthritis.
In rheumatoid arthritis, TNF-a is a proven key factor in promoting inflammation and damage to cartilage and bone.2,3 Drugs that suppress TNF-a are the new "Cadillac" therapies in the treatment of rheumatoid arthritis.
Using herbs to suppress pro-inflammatory agents

There are nutritional approaches to suppressing TNF-a and other inflammatory factors. While nutritional therapies work at a slower pace than drugs, they have the benefit of being less costly and virtually free of side effects. In fact, these nutritional approaches provide potential side benefits such as cartilage regeneration and reductions in cardiovascular disease risk.
Nettle leaf is an herb that has a long tradition of use as an adjuvant remedy in the treatment of arthritis in Germany. Nettle leaf extract contains active compounds that reduce TNF-a and other inflammatory cytokines.4,5
Not only does nettle leaf lower TNF-a levels, but it has been shown to do so by potently inhibiting the genetic transcription factor that activates TNF-a and IL-1b in the synovial tissue that lines the joint.6
A study on healthy volunteers demonstrated the anti-inflammatory potential of nettle.7 In this study, nettle extract significantly reduced TNF-a and IL-1b concentration in response to stimulation of these pro-inflammatory cytokines.
Another study conducted on 40 patients suffering from acute arthritis compared the effects of 200 mg of an anti-inflammatory drug (diclofenac) with only 50 mg of the same drug in combination with stewed nettle leaf.8 Total joint scores improved significantly in both groups by approximately 70%. The addition of nettle extract made possible a 75% dose reduction of the toxic drug, while still retaining the same anti-inflammatory benefits with reduced side effects.
Please note that while an extract from the nettle root (urtica dioica) is used to alleviate symptoms of benign prostate enlargement, it is nettle leaf extract that has shown efficacy in suppressing the pro-inflammatory cytokines TNF-a and IL-B1
Table 1
How inflammation-inducing prostaglandin E2 (PGE2) is formed:
Arachidonic acid + COX-2 = Increased Prostaglandin in E2 (PGE2) Increased Prostaglandin E2 = Inflammation
How COX-2 (cyclooxygenase-2) inhibitors work:
Arachidonic acid + COX-2 inhibitor = Reduced Prostaglandin E2 Less Prostaglandin E2 = Reduced inflammation
Other pro-inflammatory factors
Prostaglandins are hormone-like fatty acids that participate in many life functions. When present in excess levels, not all prostaglandins are beneficial. Excess levels of prostaglandin E2 (PGE2) can cause inflammation. Drugs (such as Celebrex and Vioxx) that suppress production of PGE2 are approved by the FDA as effective arthritis therapies.
Celebrex and Vioxx function by inhibiting an enzyme called cyclooxygenase-2 (COX-2) that is required to convert arachidonic acid into the destructive prostaglandin E2 (PGE2).
Another way of reducing the amount of pro-inflammatory PGE2 is to interfere with the production of arachidonic acid itself, which is how fish oil works. In one study, fish oil supplements given to rheumatoid arthritis patients reduced arachidonic acid levels by 33% compared to pre-supplement values.9 Another human study showed fish oil lowering arachidonic acid levels by 26%.10
Fish oil also suppresses the joint-tissue destructive TNF-a and IL-1B cytokines, which helps explain why so many published studies demonstrate that fish oil is an effective arthritis therapy.11-17 Studies on healthy volunteers and rheumatoid arthritis patients show that fish oil supplementation inhibits production of the proinflammatory cytokines, TNF-a and IL-1B by as much as 90%! 18
In addition to PGE2, another pro-inflammatory metabolite of arachidonic acid is leukotriene B(4). COX-2 inhibitors do not suppress leukotriene B4, which helps explain why COX-2 inhibitors usually provide only partial relief from arthritis symptoms. Fish oil, on the other hand, suppresses both leukotriene B(4) and PGE2.19-22
The effects of supplemental fish oil in suppressing leukotriene B(4) were shown in a study that compared the effect of aspirin alone or a combination of low-dose aspirin and fish oil. When aspirin was taken by itself, leukotriene B(4) levels increased 19%. When fish oil was added to the low dose aspirin regimen, leukotriene B(4) levels decreased by a striking 69%. This study showed that the combination of low-dose aspirin and moderate intake of fish oil is a potent weapon in the regulation of pro-inflammatory leukotrienes.23
Eating fish itself in lieu of meat is beneficial, in addition to taking fish oil capsules. The reason for this is that meat consumption increases arachidonic acid levels. By eating fish instead of meat, less arachidonic acid is available to convert to pro-inflammatory PGE2 and leukotriene B(4).
When rheumatoid arthritis patients are supplemented with omega-3 oils (fish, flax, Perilla), the most common effect is relief of tender joints and morning stiffness. In some cases, omega-3 oils enable the arthritis patient to reduce or eliminate the need for toxic drug therapy.24-26
Of 12 published double blind and placebo-controlled studies with a duration of 12-52 weeks, decreased joint tenderness was the most common favorable outcome reported with fish oil supplementation. Unlike toxic non-steroidal anti-inflammatory drugs, fish oil consumption is not associated with gastrointestinal toxicity, though some people experience gastric discomfort, which is why enteric-coated fish oil supplements are becoming more popular.27-36
- Fish oil provides the following benefits to those suffering from arthritis:
- Suppresses arachidonic acid, resulting in the inhibition of the pro-inflammatory prostaglandin E2 (PGE2).
- Reduces the toxic cytokines TNF-a and IL-1B, which attack the joint lining and other parts of the body.
- Interferes with the production of the inflammation-inducing fatty acid derivative leukotriene B(4).
While fish oil has three specifically identified mechanisms to inhibit inflammatory disease, arthritis patients may require additional help in suppressing excess levels of cyclooxygenase-2 (COX-2) and another enzyme called 5-lipooxygenase.
Remember, arachidonic acid is converted into the pro-inflammatory prostaglandin E2 (PGE2) by the COX-2 enzyme. The pro-inflammatory leukotriene B(4), on the other hand, requires the lipooxygenase enzyme to convert from arachidonic acid (Refer to Table 3).
The drugs Celebrex and Vioxx function as COX-2 inhibitors, but as you can see from the chart (Table 3), that still leaves the lipooxygenase pathway open to produce joint-destroying leukotriene B(4).
In experimental studies, the pharmacologically active components of the ginger root (gingerols) have been shown to inhibit both the cyclooxygenase and lipooxygenase pathways and the production of prostaglandin E2 and leukotrienes. No significant side effects have been reported using gingerols.37-39
Ginger oil is obtained by steam distillation of dried ginger root. In a study on rats,40 arthritis was induced in the knee and paw by injection of bacilli, leading to inflammation. One group of rats was also given ginger oil by mouth for 28 days starting the day before the injection. The rats given ginger oil had less than half the knee and paw inflammation compared to the controls.
Table 2
 |
How fish oil reduces inflammation:
- High prostaglandin E2 and leukotriene B(4) = Inflammation
- Fish oil supplements and fish = Reduced arachidonic acid levels
- Reduced arachidonic acid = Lower prostaglandin E2 and leukotriene B(4)
- Reduced prostaglandin E2 and leukotriene B (4) = Less inflammation
Rebuilding lost cartilage
Arthritis patients have a choice of using FDA-approved drugs and/or natural therapies to help protect the linings of the joints against autoimmune attack by dangerous cytokines and prostaglandins. But what about the cartilage destruction that already occurred?
According to the March 15, 2000 issue of the Journal of the American Medical Association (JAMA), a review of all known studies on glucosamine and chondroitin in the treatment of arthritis showed a mean improvement in quality scores of 35.5%. The conclusions of the authors were:
"Trials of glucosamine and chondroitin preparations for osteoarthritis symptoms demonstrate moderate to large effects, but quality issues and likely publication bias suggest that these effects are exaggerated. Nevertheless, some degree of efficacy appears probable for these preparations."
This rather pessimistic conclusion may be warranted based on the knowledge that to adequately treat arthritis, it is crucial to suppress cartilage-destroying cytokines like TNF-a and pro-inflammatory fatty acid-derivatives such as PGE2. This is where a holistic approach to treating arthritis starts to make sense even in the world of conventional medicine. Since glucosamine and chondroitin preparations obviously provide some benefit, it makes sense to combine them with nutritional and/or drug therapies that suppress inflammatory damage to the lining of the joint.
Among the natural therapies for osteoarthritis, glucosamine sulfate is probably the best known. It is extensively used as a drug for osteoarthritis in Europe, and it has been readily available in health food stores in the United States in recent years.
Glucosamine is a naturally occurring substance in the body, synthesized in the chondrocytes. The body uses supplemented glucosamine to synthesize the proteoglycans and the water-binding glycosaminoglycans (GAGs) in the cartilage matrix. In addition to providing raw material, the presence of glucosamine seems to stimulate the chondrocytes in their production of these substances. Glucosamine also inhibits certain enzymes, which destroy the cartilage, e.g. collagenase and phospholipase. By blocking pathogenic mechanisms that lead to articular degeneration, glucosamine delays the progression of the disease and relieves symptoms even for weeks after termination of the treatment.41
Chondroitin sulfate is a major component of cartilage. It is a very large molecule, composed of repeated units of glucosamine sulfate. Like glucosamine, chondroitin sulphate attracts water into the cartilage matrix and stimulates the production of cartilage. Likewise it has the ability to prevent enzymes from dissolving cartilage. Although the absorption of chondroitin sulfate is much lower than that of glucosamine (10-15% versus 90-98%), recent studies have shown good results from long-term treatment with chondroitin sulfate, reducing pain and increasing range of motion.42-44
Table 3
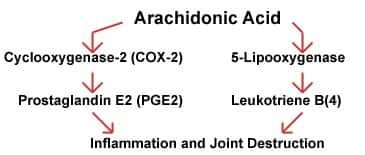 |
The toxic metabolic cascade of arachidonic acid.
Note that two specific pathways by which arachidonic acid can cause arthritic conditions.
Recommendations
For those with severe rheumatoid arthritis that does not respond to natural therapies, the drug Enbrel is the best therapy in the world. Enbrel may also be effective in treating osteoarthritis if combined with glucosamine and chondroitin. Enbrel costs about $12,000.00 a year and requires the patient to visit the doctor two times every week for injections. There are, however, natural solutions to the multi-faceted causes of arthritis that have been identified in this article.
By suppressing excess levels of tumor necrosis factor alpha (TNF-a) and other tissue destroying factors, many diseases associated with normal aging such as congestive heart failure, Type II diabetes and immune dysfunction may be avoided.49,50 TNF-a may be suppressed with drugs (Enbrel) or nutrients such as nettle leaf extract and EPA-DHA fish oil supplements.
The safe use of drugs and natural therapies
When choosing between drugs and natural therapies, some important considerations are in order. If natural therapies are going to be tried first, it should be noted that the published studies indicate it will take between three to six weeks for inflammation to cease and pain relief to occur. Some arthritis patients will use natural therapies along with lower doses of prescription anti-inflammatory drugs during the initiation phase.
A degree of caution is advised when combining prescription drugs with certain natural therapies. For example, if the drug Enbrel is being used to suppress TNF-a, it would be advisable to avoid nettle leaf extract supplements that also suppress TNF-a. There is a theoretical possibility that too much TNF-a could be suppressed if both Enbrel and nettle leaf extracts were taken at the same time. Nettle leaf extract can be found in the ArthroPro and ChronoForte supplements offered by Life Extension. Nettle leaf is present in these products to protect against the multiple deleterious effects of excess TNF-a production that occur with aging. For most people, the maximum safe dose for the potent nettle leaf extract is 2500 milligrams a day, which is the amount that would be consumed if a person takes the maximum dose of both ChronoForte and ArthroPro. Since Enbrel is contraindicated during the time when someone is suffering from acute infection, we recommend that ChronoForte and ArthroPro also be avoided during the time a person is battling an infection, and may need higher amounts of TNF-a to attack the infectious agent. Remember that the reason it is so important for aging humans to suppress chronically high levels of TNF-a is because this destructive cytokine is linked to a wide variety of age-associated degenerative diseases.
When it comes to inhibiting COX-2 with drugs such as Celebrex and Vioxx, it might be wise to avoid high potency gingerol, PABA and curcumin supplements when using these drugs because of a theoretical possibility of over-suppression of the COX-1 and COX-2 enzymes. Please know that while Celebrex and Vioxx are officially classified as COX-2 inhibitors, they also suppress COX-1. Over suppression of COX-1 is linked with the gastrointestinal side effects of NSAID arthritis drugs.45,46
The combination of fish oil with Celebrex or Vioxx could theoretically cause over suppression of prostaglandin E2 (PGE2). Remember, while high levels of PGE2 provokes an inflammatory response, the body does need some PGE2 to maintain mucosal integrity of the intestinal wall.47,48
In summary:
- If taking the drug Enbrel, avoid products that contain nettle leaf extract such asArthroPro and ChronoForte.
- If taking the drugs Celebrex, Vioxx, Lodine or other COX-2 inhibitors, you may want to avoid taking excessive amounts of gingerol, PABA, curcumin or fish oil. Moderate amounts of these nutrients should not cause a problem.
- Do not exceed 2500 mg per day of nettle leaf extract. During serious infections, do not exceed 1500 mg per day of nettle leaf extract.
References
- Feldman AM, et al. The role of tumor necrosis factor in the pathophysiology of heart failure. J Am Coll Cardiol 2000 Mar 1;35(3):537-44
- Bertolini DR, et al. Stimulation of bone resorption and inhibition of bone formation in vitro by human tumour necrosis factors. Nature 1986 Feb 6-12;319 (6053):516-8
- Saklatvala J. Tumour necrosis factor alpha stimulates resorption and inhibits synthesis of proteoglycan in cartilage. Nature 1986 Aug 7-13;322 (6079):547-9
- Teucher T, et al. [Cytokine secretion in whole blood of healthy subjects following oral administration of Urtica dioica L. plant extract]. Arzneimittelforschung 1996 Sep;46(9):906-10
- Klingelhoefer S, et al. Antirheumatic effect of IDS 23, a stinging nettle leaf extract, on in vitro expression of T helper cytokines. J Rheumatol 1999 Dec;26 (12):2517-22
- Riehemann K, et al. Plant extracts from stinging nettle (Urtica dioica), an antirheumatic remedy, inhibit the proinflammatory transcription factor NF-kappaB. FEBS Lett 1999 Jan 8;442(1):89-94
- Obertreis B, et al. Published erratum appears in Arzneimittelforschung 1996 Sep;46(9):936 Ex-vivo in-vitro inhibition of lipopolysaccharide stimulated tumor necrosis factor-alpha and interleukin-1 beta secretion in human whole blood by extractum urticae dioicae foliorum. Arzneimittelforschung 1996 Apr;46(4):389-94
- Chrubasik S, et al. Evidence for antirheumatic effectiveness of Herba Urticae in acute arthritis: a pilot study. Phytomedicine 1997 4:105-108
- Sperling RI, et al. Effects of dietary supplementation with marine fish oil on leukocyte lipid mediator generation and function in rheumatoid arthritis. Arthritis Rheum 1987 Sep;30(9):988-97
- Conquer JA, et al. Effect of supplementation with dietary seal oil on selected cardiovascular risk factors and hemostatic variables in healthy male subjects. Thromb Res 1999 Nov 1;96(3):239-50
- Venkatraman JT, et al. Effects of dietary omega-3 and omega-6 lipids and vitamin E on serum cytokines, lipid mediators and anti-DNA antibodies in a mouse model for rheumatoid arthritis. J Am Coll Nutr 1999 Dec;18(6):602-13
- Lo CJ, et al., Fish Oil Decreases Macrophage Tumor Necrosis Factor Gene Transcription by Altering the NFkappaB Activity. J Surg Res 1999 Apr;82(2):216-221
- Khalfoun B, et al., Docosahexaenoic and eicosapentaenoic acids inhibit in vitro human endothelial cell production of interleukin-6. Adv Exp Med Biol 1997;400B:589-97
- Caughey GE, et al. The effect on human tumor necrosis factor alpha and interleukin 1 beta production of diets enriched in n-3 fatty acids from vegetable oil or fish oil. Am J Clin Nutr 1996 Jan;63(1):116-22
- Khalfoun B, et al. Docosahexaenoic and eicosapentaenoic acids inhibit in vitro human lymphocyte-endothelial cell adhesion. Transplantation 1996 Dec 15;62(11):1649-57
- Espersen GT, et al. Decreased interleukin-1 beta levels in plasma from rheumatoid arthritis patients after dietary supplementation with n-3 polyunsaturated fatty acids. Clin Rheumatol 1992 Sep;11(3):393-5
- Curtis CL, et al. n-3 fatty acids specifically modulate catabolic factors involved in articular cartilage degradation. J Biol Chem 2000 Jan 14;275(2):721-4
- James MJ, et al. Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr 2000 Jan;71(1 Suppl):343S-8S
- Kremer JM. n-3 fatty acid supplements in rheumatoid arthritis. Am J Clin Nutr 2000 Jan;71(1 Suppl): 349S-51S
- Raederstorff D, et al. Anti-inflammatory properties of docosahexaenoic and eicosapentaenoic acids in phorbol-ester-induced mouse ear inflammation. Int Arch Allergy Immunol 1996 Nov;111(3):284-90
- Mayatepek E, et al. Influence of dietary (n-3)-polyunsaturated fatty acids on leukotriene B4 and prostaglandin E2 synthesis and course of experimental tuberculosis in guinea pigs. Infection 1994 Mar-Apr;22(2):106-12
- Terano T, et al. Eicosapentaenoic acid as a modulator of inflammation. Effect on prostaglandin and leukotriene synthesis. Biochem Pharmacol 1986 Mar 1;35(5):779-85
- Engstrom K et al. Effect of low-dose aspirin in combination with stable fish oil on eicasanopids. EPA and Eicosanoids. Prost Leukotr Ess Fat Acid 1997 57:229
- Kremer JM, et al. Effects of manipulation of dietary fatty acids on clinical manifestations of rheumatoid arthritis. Lancet 1985 Jan 26;1(8422):184-7
- Skoldstam L, et al. Effect of six months of fish oil supplementation in stable rheumatoid arthritis. A double-blind, controlled study. Scand J Rheumatol 1992;21(4):178-85
- Lau CS, et al. Effects of fish oil supplementation on non-steroidal anti-inflammatory drug requirement in patients with mild rheumatoid arthritis-a double-blind placebo controlled study. Br J Rheumatol 1993 Nov;32(11):982-9
- Faarvang KL, et al. [Fish oils and rheumatoid arthritis. A randomized and double-blind study]. Ugeskr Laeger 1994 Jun 6;156(23):3495-8
- Nielsen GL, et al. The effects of dietary supplementation with n-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: a randomized, double blind trial. Eur J Clin Invest 1992 Oct;22(10):687-91
- Cleland LG, et al.Clinical and biochemical effects of dietary fish oil supplements in rheumatoid arthritis. J Rheumatol 1988 Oct;15(10):1471-5
- Kremer JM, et al. Fish-oil fatty acid supplementation in active rheumatoid arthritis. A double-blinded, controlled, crossover study. Ann Intern Med 1987 Apr;106(4):497-503
- Kjeldsen-Kragh J, et al. Dietary omega-3 fatty acid supplementation and naproxen treatment in patients with rheumatoid arthritis. J Rheumatol 1992 Oct;19(10):1531-6
- van der Tempel H, et al. Effects of fish oil supplementation in rheumatoid arthritis. Ann Rheum Dis 1990 Feb;49(2):76-80
- Kremer JM, et al. Effects of high-dose fish oil on rheumatoid arthritis after stopping nonsteroidal antiinflammatory drugs. Clinical and immune correlates. Arthritis Rheum 1995 Aug;38(8):1107-14
- Fortin PR, et al. Validation of a meta-analysis: the effects of fish oil in rheumatoid arthritis. J Clin Epidemiol 1995 Nov;48(11):1379-90
- Kremer JM, et al. Dietary fish oil and olive oil supplementation in patients with rheumatoid arthritis. Clinical and immunologic effects. Arthritis Rheum 1990 Jun;33(6):810-20
- Lassus A, et al. Effects of dietary supplementation with polyunsaturated ethyl ester lipids (Angiosan) in patients with psoriasis and psoriatic arthritis. J Int Med Res 1990 Jan-Feb;18(1):68-73
- Kiuchi F, et al. Inhibition of prostaglandin and leukotriene biosynthesis by gingerols and diarylheptanoids. Chem Pharm Bull (Tokyo) 1992 Feb;40 (2):387-91
- Srivastava KC, et al. Ginger (Zingiber officinale) in rheumatism and musculoskeletal disorders. Med Hypotheses 1992 Dec;39(4):342-8
- Flynn DL, et al. Inhibition of human neutrophil 5-lipoxygenase activity by gingerdione, shogaol, capsaicin and related pungent compounds. Prostaglandins Leukot Med 1986 Oct;24(2-3):195-8
- Sharma JN, et al. Suppressive effects of eugenol and ginger oil on arthritic rats. Pharmacology 1994 Nov;49(5):314-8
- Qiu GX, et al. Efficacy and safety of glucosamine sulfate versus ibuprofen in patients with knee osteoarthritis. Arzneimittelforschung 1998 May;48 (5):469-74
- McAlindon TE, et al. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA 2000 Mar 15;283(11):1469-75
- Omata T, et al. Effects of chondroitin sulfate-C on articular cartilage destruction in murine collagen-induced arthritis. Arzneimittelforschung 2000 Feb;50(2):148-53
- Leeb BF, et al. A metaanalysis of chondroitin sulfate in the treatment of osteoarthritis. J Rheumatol 2000 Jan;27(1):205-11
- Schuna AA. New drugs for the treatment of rheumatoid arthritis. Am J Health Syst Pharm 2000 Feb 1;57(3):225-34
- Yamamoto S. [Essential unsaturated fatty acids]. Nippon Rinsho 1999 Oct;57(10):2242-6
- Brzozowski T, et al. Expression of cyclooxygenase (COX)-1 and COX-2 in adaptive cytoprotection induced by mild stress. J Physiol Paris 2000 Mar-Apr;94 (2):83-91
- Sakamoto C, et al. EGF stimulates both cyclooxygenase activity and cell proliferation of cultured guinea pig gastric mucous cells. J Gastroenterol 1994 Jul;29 Suppl 7:73-6
- Paolisso G, et al. Advancing age and insulin resistance: new facts about an ancient history. Eur J Clin Invest 1999 Sep;29(9):758-69
- Sliwa K, et al. Peripartum cardiomyopathy: analysis of clinical outcome, left ventricular function, plasma levels of cytokines and Fas/APO-1. J Am Coll Cardiol 2000 Mar 1;35(3):701-5
