Life Extension Magazine®
The Deprenyl Controversy |
| Recent papers in the British Medical Journal (BMJ) and Annals of Neurology (AN) have called into question the value of deprenyl as a treatment for Parkinson's disease. After a series of positive studies on deprenyl, starting in the mid 1980s, these papers have doctors around the world debating whether they should continue to prescribe deprenyl for Parkinson's disease. As one of the earliest advocates of deprenyl for Parkinson's disease, Alzheimer's disease and as a general anti-aging therapy, the Life Extension has analyzed the findings of these papers in the context of past findings on deprenyl, and has re-evaluated our recommendations of deprenyl. The British Deprenyl StudyIn the December 1995 BMJ, a paper by A.J. Lees (on behalf of the Parkinson's Disease Research Group of the United Kingdom) reported the findings of a multi-center (93 hospitals) open clinical trial.1 This trial compared standard L-Dopa treatment (including a dopa decarboxylase inhibitor) to the combination of L-Dopa and deprenyl in 520 early-stage Parkinson's patients after an average of 5-6 years of follow-up. The Rationale Behind L-Dopa TreatmentThe rationale behind the standard L-Dopa treatment, which has been in routine use for the past 25 years, is that L-Dopa, the precursor of the neurotransmitter dopamine, serves as a substitute source of dopamine, replacing dopamine lost after the death of dopamine-secreting neurons in the substantia nigra region of the brain. The accelerated depletion of dopamine in the brain resulting from the destruction of these neurons is the primary cause of Parkinson's disease. Since dopamine plays an important role in movement, coordination, strength, sex drive, and cognitive function, Parkinson's patients suffer from progressive movement and cognitive disorders that greatly reduces the quality of their lives and shortens their lifespan. A Short-Lived "Miracle"When L-Dopa was first given to Parkinson's patients in the 1960s, it was widely hailed as a "miracle" drug because of the dramatic improvements in function it produced. But when longer-term studies were conducted, it was found that the benefits were short-lived, that the drug does not slow the progression of Parkinson's Disease, and that it produces serious adverse side effects, including involuntary movements, fluctuations in motor performance and mood, and psychiatric abnormalities.2 As a result, doctors began reserving L-Dopa for moderately or severely impaired patients, where its functional benefits outweigh its side effects. The Dilemma For Parkinson's DoctorsFor decades, doctors searched for a therapy that could help early-stage Parkinson's patients without adverse side effects. Their dilemma was that at diagnosis most Parkinson's patients have lost up to 80% of their dopaminergic neurons.3 By the time the symptoms of the disease begin to seriously interfere with the quality of their lives, they've already lost almost all of their dopamine-producing neurons. L-Dopa is merely a source of dopamine. It cannot prevent the ongoing loss of neurons, but only provides temporary symptomatic relief. The Promise Of DeprenylThat's why doctors were so excited when deprenyl (also known as selegiline), a drug developed by Joseph Knoll of the University Of Semmelweis in Hungary, came on the scene in the 1980s. A series of positive studies suggested that deprenyl might not only improve the quality of life for Parkinson's patients, but might also slow the progression of the disease. These studies showed that deprenyl could extend lifespan in laboratory animals,4 restore lost sex drive in animals,5 and neutralize the deleterious effects of powerful neurotoxins such as MPTP (l-methyl-4-phenyl-1,2,3,6-tetrihydropyridine)6 and 6-hydroxydopamine.7 Doctors were especially intrigued by deprenyl's ability to counteract the effects of MPTP, which produced severe Parkinsonian symptoms in young people who took it as a "street drug", and which induces a Parkinson-like syndrome in laboratory animals. |
 |
Clinical Trials |
Hopes for deprenyl were raised in 1985 when Austrian researcher, W. Birkmayer, found (in a retrospective study) that Parkinson's patients receiving both L-Dopa and deprenyl lived 30% longer than patients receiving L-Dopa alone.8 In the next couple of years, multi-center trials with deprenyl were started in the U.S., England and Italy. The largest of these trials was the double-blind, placebo-controlled DATATOP study in the U.S (and Canada), which tested deprenyl and vitamin E in 800 early-stage Parkinson's patients. Its main objective was to see how long it would take before the patients became impaired enough to require L-Dopa. The medical community was electrified in 1989 when the DATATOP trial was cut short because of dramatic benefits in the patients receiving deprenyl. A few months later, a paper in the New England Journal of Medicine reported a 9-month delay before L-Dopa was necessary in the deprenyl patients. DATATOP scientists hypothesized that deprenyl might slow the progression of Parkinson's disease by slowing down the loss of dopaminergic neurons. FDA approval of deprenyl as a treatment for Parkinson's disease soon followed, and deprenyl soon became the drug of choice for early-stage Parkinson's disease patients. Proposed Mechanisms Of ActionDeprenyl is a selective, irreversible inhibitor of monoamine oxidase B (MAO-B), the enzyme that degrades dopamine. Since the depletion of dopamine is the primary factor in the genesis of Parkinson's disease, and levels of MAO-B increase with advancing age in humans,11 it is assumed that the effect of deprenyl therapy is to conserve dopamine in the brain. Scientists speculated that deprenyl may protect brain cells from damage in Parkinson's patients through its action as an MAO-B inhibitor, or by countering the deleterious effects of free radical damage caused by dopamine metabolism and other factors.12 In the early 1990s, scientists at the University of Toronto found that deprenyl could "rescue" dopaminergic (and other) neurons from functional damage in tissue culture.13-15 Since this effect occurred at doses of deprenyl lower than those needed to inhibit MAO-B, it was suggested that there may be another mechanism of action that enables deprenyl to protect neurons in the brain.15 When the results of other clinical trials with deprenyl showed significant benefits for Parkinson's patients16 and Alzheimer's patients, it was assumed that deprenyl is an effective treatment for Parkinson's disease, that the drug might be effective for other neurodegenerative diseases, and that it might retard aging by slowing the loss of essential neurons in the brain. The Findings Of The British StudyThese assumptions must now be re-evaluated in light of the recent BMJ and AN papers. The BMJ study investigated the effect of three treatment regimens: L-Dopa alone, L-Dopa and deprenyl, and bromocriptine (a dopamine agonist). The BMJ paper deals primarily with the first two regimens. The treatment groups were similar with respect to age, sex, duration of Parkinson's disease, and baseline disability scores. The study was conducted by 58 physicians at 93 hospital throughout the United Kingdom. Patients were recruited between September 1985 and September 1990 at University College Hospitals and randomly assigned to the three groups. The doctors treating the patients in both L-Dopa groups determined what they considered the optimal dose of L-Dopa for each patient, which was given daily in three divided doses after meals. Deprenyl was given twice daily in 5-mg doses. Mortality and disability scores were assessed at the beginning of the trial and every 3 to 4 months thereafter, preferably in the presence of one of the patients' close relatives. The severity of adverse side effects were rated on a scale of 0-3 at each visit. Results Of StudyAnalysis was performed in 520 patients in both groups, regardless of whether they were subsequently withdrawn from treatment. The dose of L-Dopa was increased gradually in both groups as the patients' condition worsened. After a year, the median dose of L-Dopa in the first group (L-Dopa alone) was 375 mg per day, while the median dose in the second group (L-Dopa plus deprenyl) was 375 mg After four years, the median dose of L-Dopa in group one rose to 625 mg per day, but remained at 375 mg per day in the second group. The primary finding in The British Study, after an average of 5-6 years of follow-up, was that mortality was about 60% higher in patients given both L-Dopa and deprenyl than in those given L-Dopa alone, and that this effect was independent of sex and age. This finding was essentially the same, regardless of whether the analysis was done for patients while they were being treated, or included the period after they (252 out of 520) withdrew from the study. The other findings were that disability scores were slightly worse in patients receiving L-Dopa than in patients receiving both L-Dopa and deprenyl, and that severe motor complications were more frequent in patients given the combined treatment. The British Scientists' ConclusionsThe British scientists' concluded that "combined treatment with levodopa and selegiline (deprenyl) in patients with mild, previously untreated, Parkinson's disease seems to confer no detectable clinical benefit over treatment with levodopa alone. Furthermore, mortality was significantly increased in the patients given levodopa and selegiline. This is the first study to report such a finding. Analysis of mortality in other ongoing studies will be needed to see if this finding can be corroborated." "The critical question is whether the relation between levodopa and selegiline and increased mortality is genuinely causal....The precise cause of the increased mortality... remains to be determined. "In the meantime, the patients in arm two of our trial (levodopa and selegiline) will be advised of our results and advised to withdraw selegiline from their treatment regimens." The Results Of The Study Are ControversialThe fact that the British study is the first to report increased mortality in Parkinson's patients receiving deprenyl, coupled with the recommendation that patients stop taking it, has led to debate among doctors, many of whom aren't yet ready to accept this recommendation for their own patients. The March 16, 1996 issue of the British Medical Journal published eight letters in response to the Parkinson's study, some of which contested the contention that deprenyl was the cause of the excess mortality in the L-Dopa/deprenyl group.18 Some doctors pointed out flaws in the British study, others presented evidence to contradict the findings of the study, and some gave their own interpretation of the findings. Clinical Trials Contradicting The British StudyThe manufacturer of deprenyl cited a collection of findings from clinical trials with deprenyl, all of which, it was stated, contradict the extra mortality found in the British study. As they put it: "We have gathered data from 10 controlled, long-term studies (some published, some continuing); in seven the duration of treatment was at least 3.5 years; 983 patients received selegiline alone or with levodopa, and 1093 received placebo or other antiparkinsonian drugs. The mortality was 2.8% and 3.3% respectively (Table 1). When only data from the studies of at least 3-5 years duration were analyzed, the mortality was 5.2% for the selegiline group and 5.5% for the control group."18 The British scientists responded that the results of the combined trials are "not directly comparable" to their results because they include trials with deprenyl alone as well as deprenyl and L-Dopa. They also claimed that the mortality data in the trials with more than 3.5 years of follow-up were comparable to their mortality data, but failed to provide evidence to support this contention.
|
 |
The Mt. Sinai Study |
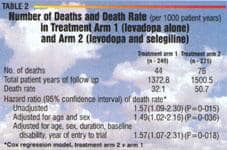
One of the controlled clinical trials with contrasting data was conducted at Mt. Sinai Medical Center in New York.19 Two neurologists who participated in the Mt. Sinai study-C.W. Olanow and James H. Godbold-were among the letter writers who presented alternative data to the findings of the British study. They wrote: "We performed a prospective double blind study in 101 comparable patients with Parkinson's disease. They were randomly assigned to receive selegiline or placebo plus levodopa or bromocriptine. After five years, only eight deaths had occurred (five in patients taking placebo and three in patients taking selegiline)."19 The British Mortality DataThe finding of higher mortality in the deprenyl/L-Dopa group-the first of its kind-must be scrutinized carefully, as it has serious implications for Parkinson's disease patients and others who have relied on the findings of previous studies. A look at the mortality data in the British study leads to several unanswered questions. First is the question of when the deaths referred to in the BMJ paper occurred. According to the authors: "No significant difference in mortality was present at the time of the three year analysis. A further interim analysis in December 1994 showed that the mortality in the group treated with levodopa alone was significantly different from the rate in the group given levodopa in combination with selegiline." Since the BMJ paper, which was published in Dec. 1995, deals with 5-6 years of data, it seems as if the three-year analysis referred to in the paper occurred in 1992 or 1993. Thus, it appears that the 60% greater mortality reported for the deprenyl/L-Dopa group occurred between 1992/1993 and 1994/1995. However, little information is reported about this critical period. Because of their recommendation that the patients in the group stop taking deprenyl, it is clear that the authors presume that deprenyl was responsible for the extra deaths, with little or no consideration for alternative explanations. Yet, there were things going on during this period that suggest other possible explanations for the extra deaths. High Drop-Out Rate, Questions About ComplianceFirst is the fact that many patients left the study during the period in question because they were either lost to follow-up,violated the protocol, deteriorated too much, had adverse reactions, or had their diagnoses revised. In all, 129 (52%) of the L-Dopa only group and 123 (45%) of the deprenyl/L-Dopa group withdrew from the study. This kind of drop out rate raises the possibility that other, unreported drugs could have been taken by the patients during the study, which could have played a role in causing the extra deaths. An additional concern not addressed in the paper is compliance. How many of the patients complied and how was compliance determined? Reassigning PatientsThe authors report that-since it was an open trial-they reassigned patients to other groups when it appeared they were having problems with the treatment regimen in their original group. As they put it: "Patients who were unable to tolerate the trial drug or gain useful functional improvement (initial improvement of 20% or more in rating scales and continuing improvement above baseline levels of disability) could either be randomized again to a different arm of the trial or withdrawn. Patients have been considered in this report only in relation to their original randomization." With this kind of change going on at 93 different medical centers, it's entirely possible that there were mistakes made in tabulating and analyzing the mortality data. Yet not a word is said in the paper about what they did to protect against such mistakes. Differences In Follow-UpThe authors also present data that could explain some of the extra mortality in the deprenyl group. (Table 2) They report 1,372.6 patient years of follow-up for the patients receiving L-Dopa only (treatment arm 1), and 1,500.5 patient years of follow-up for the patients receiving deprenyl and L-Dopa.
Since the deprenyl/L-Dopa group was followed longer than the L-Dopa only group, it's not surprising that more of them died. Nowhere in the paper does it say how many of the extra deaths occurred during the longer follow-up period for the patients receiving deprenyl/L-Dopa. The Reported Causes Of DeathAnother unsettling factor is the authors report that many of the patients in the deprenyl/L-Dopa group died of "Parkinson's Disease". There were 45 reported deaths in the L-Dopa group compared to 76 in the deprenyl/L-Dopa group, but 26 (52%) of those deaths were attributed to Parkinson's disease compared to only 7 (16%) in the L-Dopa group. (Table 3)
The problem is that Parkinson's patients doesn't usually die of Parkinson's disease. In most cases, the disease weakens patients to the extent that they die of other causes such as heart attack, stroke, or cancer. In one of the letters to the editor in the March 16 issue of the British Medical Journal, scientists from the Neurodegenerative Diseases Research Centre at King's College in London wrote: "Most of the excess deaths in arm 2 was directly attributed to Parkinson's disease itself, this information being obtained from death certificates. We were surprised to find that Parkinson's disease featured as a primary case of death, as most patients with the disease die of its complications." Instead of trying to explain this anomaly, the authors responded as follows: "The precise cause of the increased mortality in arm 2 remains to be determined. Selegiline increased the number of early adverse events, and it is conceivable that it may have deleterious effects on the cardiovascular and cerebrovascular system. For example, in the DATATOP study a higher incidence of cardiac rhythm disturbance was reported in patients treated with selegiline." Instead of answering a reasonable question about data in their own study, the British scientists responded with data from another study (the DATATOP trial). In fact, data from their own study contradicts their suggestion that deprenyl might have deleterious effects on the cardio- and cerebrovascular health. Table 3 (from the British study) shows 20 cardiovascular and cerebrovascular deaths in the L-Dopa only group, representing 44% of the deaths reported for this group, and 21 such deaths in the deprenyl/L-Dopa group, representing only 28% of the deaths reported for this group. Hardly evidence that deprenyl may have been causing heart attacks and strokes! Recent Papers From The DATATOP StudyShortly after the results of the British study were published, two papers from the DATATOP study were published in the January 1996 issue of Annals Of Neurology. DATATOP is an acronym for Deprenyl and Tocopherol Antioxidant Therapy of Parkinsonism. It is the largest clinical trial ever conducted in early-stage, previously untreated Parkinson's patients, including (originally) 800 patients at 25 medical centers in the U.S. and Canada. The DATATOP trial started as a controlled, double-blind study including four groups: deprenyl (10 mg a day), vitamin E (2,000 units a day), both deprenyl and vitamin E at these doses, and placebo. The clinical endpoint in the DATATOP trial was the length of time it took for patients to develop severe enough symptoms to require L-Dopa therapy. The decision to prescribe L-Dopa was left to the discretion of the treating physicians, who used well-established tests to measure the degree of disability in their patients. About 18 months after the study started, it was apparent (in spite of the blinding process) that the deprenyl patients were doing much better than the patients in the other groups. As a result, it was decided to break the code, end the study, analyze and publish the data, and enter those patients who wished to continue into an open clinical trial in which every patient would receive deprenyl. Protocol For The Second Phase Of The DATATOP TrialTen months after the original DATATOP trial began, a new protocol was instituted for the patients who already needed L-Dopa. These patients stopped taking anything for a month while they were being evaluated. They were then restarted on their original medications and then, two weeks later, were started on standard L-Dopa therapy (L-Dopa plus Carbidopa). A month later, they came in for a follow-up visit and then again at 3-month intervals. L-Dopa dosage was adjusted during the rest of the trial by the treating physicians for the 371 patients enrolled in this phase of the trial. The other arm of the second phase of the trial was started after the original trial was ended because of the positive results in the patients receiving deprenyl. At the time, there were 423 patients who did not yet require L-Dopa therapy. Of these, 367 agreed to be withdrawn from their assigned treatments (deprenyl and/or vitamin E) for up to 2 months while they were being evaluated. During this 2-month withdrawal period, four patients got worse enough to require L-Dopa, 1 withdrew from the trial, and 52 were given deprenyl because of increased disability from Parkinson's disease. The remaining 310 patients agreed to be restarted on their previous regimen, with those who had been taking vitamin E or placebo given an additional 10 mg a day of deprenyl.
|
 |
Results Of The Trial |
The DATATOP scientists found that the advantages of deprenyl during the first 18-24 months were later lost. Although there were significant delays in the time it took them to reach the point where they needed L-Dopa early on, they eventually reached the point - as their disease progressed - where they needed L-Dopa faster than patients who had received placebo. As they put it: "A striking feature of our data is that...some deprenyl subjects whose symptoms were relatively severe at baseline had received a disproportionate but temporary benefit from deprenyl. That is, the illness of the deprenyl subjects was ameliorated during the original phase of the DATATOP study, but subsequently reverted to its 'natural' course during the open-label phase." The DATATOP scientists found several factors that might have contributed to the decline in function in the patients treated with deprenyl from the start of the trial. First that the deprenyl patients were significantly more impaired to begin with. This was true both for the patients who required L-Dopa early in the trial and for those whose need for L-Dopa was delayed by deprenyl treatment. Another factor was the effect of the 2-month withdrawal of deprenyl from the patients who had been receiving it prior to the start of the second phase of the trial. At the time of their last evaluation-just before the 2-month withdrawal period-the deprenyl-treated patients were significantly less impaired than the patients who had been receiving placebo or vitamin E. However, during the 2-month withdrawal period, the deprenyl patients declined significantly more than the patients who had not received deprenyl. The perils of withdrawal from deprenyl are discussed in one of the letters in the March 16, 1996 BMJ from clinicians familiar with its use in Parkinson's disease patients: "...Ten patients felt no different and one felt better after stopping selegiline. In all cases, no great difference in function was recorded in the diary charts. Five patients, however, felt considerably worse after stopping selegiline, and all had restarted it before review at the clinic. All these patients reported feeling slower and stiffer when not taking selegiline. Three patients reported considerably more 'off' periods (that is, recurrence of symptoms) when not taking selegiline. In these three patients, the average number of hours a day recorded as being 'off' was 4.3 while they were taking selegiline compared with 8.0 after they stopped it." Uncertainty About Deprenyl For Parkinson's PatientsNow that there is clinical evidence that the short-term benefits of deprenyl may be lost as the disease progresses, and that giving patients deprenyl in addition to L-Dopa may be harmful, there is uncertainty about when or in what dose deprenyl should be prescribed for Parkinson's patients, or whether it should be prescribed at all. The "critical question" for the British scientists is "whether the relation between levodopa and selegiline and increased mortality is genuinely causal." While they advised the patients in their study to stop taking deprenyl, their study did not deal with the effects of deprenyl by itself in early stage Parkinson's patients. The DATATOP scientists, whose study did address this issue, re-affirmed the benefits of deprenyl for early-stage Parkinson's patients, but were concerned about the loss of benefit in their patients as the disease progressed, and were guarded in their advice to physicians. As they put it in the first of their Annals of Neurology papers: "Despite the controversies surrounding its mechanisms, controlled studies of deprenyl as monotherapy in early Parkinson's disease are consistent in demonstrating a delay in disability, as measured by the need for levodopa therapy....To the extent that it is desirable to delay levodopa therapy, deprenyl remains a rational therapeutic option for patients with early Parkinson's disease. However, questions linger about the optimal dosage of deprenyl, the sustainability of its benefits, and its impact on other relevant outcomes, such as nigral degeneration and mortality." In discussing the long-term outcome with deprenyl treatment in their study, the DATATOP scientists raised the following questions: "The failure of extended deprenyl treatment to sustain its superior benefits may in part be related to
The Foundation's Recommendations Of DeprenylAt The Foundation, we take the findings of the British and DATATOP studies very seriously. They are the largest clinical trials ever conducted on the use of deprenyl in Parkinson's patients and their results raise questions about the value of deprenyl for such patients. The combination of deprenyl and L-Dopa was found to be harmful to Parkinson's patients in the British study and appeared to be detrimental to some patients in the DATATOP study. As a result, we now recommend against the use of combined deprenyl/L-Dopa therapy in previously untreated patients. We still believe that this combination may be beneficial for Parkinson's patients if lower doses of deprenyl are used. The evidence for this position is given later in the article. Physicians may wish to try low-dose deprenyl and L-Dopa in the later stages of Parkinson's disease on an experimental basis. We do not believe that Parkinson's patients currently on deprenyl/L-Dopa therapy should stop taking deprenyl if they're doing well on this protocol because of the potential harm of withdrawing treatment, but physicians should consider reducing the dose of deprenyl (or eliminating it entirely) as the disease progresses based upon the condition of their patients. (As always, the final decision in such matters should be left in the hands of the treating physician.) Since no evidence has been presented to contradict the findings of the DATATOP study (and other studies) that deprenyl by itself is beneficial for early-stage Parkinson's patients, our recommendation for the use of deprenyl in such patients stands, however we are revising our dosage recommendations (which will be discussed later). Why We Continue To Recommend Deprenyl For Anti-Aging PurposesSince neither the British nor the DATATOP study dealt with the issue of low-dose deprenyl in healthy, normally aging persons, we continue to recommend deprenyl as an anti-aging drug, although we now recommend a dosage level of only 10 mg a week (one-seventh the dosage in the Parkinson's studies). This can be achieved by taking one 5-mg tablet of deprenyl twice a week or one tablet a day of the multi-anti-aging pill offered by Conseil De Sante in Switzerland, which includes 1.5 mg of deprenyl, 7.5 mg of vinpocetin, 4 mg of hydergine and 50 mg of procaine. Our decision to continue recommending deprenyl for anti-aging purposes is based on the considerable body of animal and cell culture studies suggesting that deprenyl may have neuroprotective and anti-aging effects. These include studies by Joseph Knoll, Gwen Ivy of the University of Toronto, and scientists at the University of Frankfort, which have shown that deprenyl can extend both mean and maximum lifespan in laboratory animals. Although studies extending lifespan in animals can only suggest that a similar regimen might have such effects in humans, it remains the best evidence we have at this time. Deprenyl Blocks MPTP NeurotoxicityThere have been many studies showing that deprenyl can block the effects of powerful neurotoxins through several proposed mechanisms of action. MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) is a potent neurotoxin that specifically destroys dopamine-producing neurons in the substantia nigra region of the brain leading to the depletion of dopamine, which causes Parkinson-like symptoms in mice, monkeys and humans. Deprenyl blocks MPTP destruction by inhibiting MAO-B activity, which is necessary to convert MPTP to its toxic metabolite MPP+. The ability of deprenyl to prevent the formation of MPP+ by inhibiting MAO-B has been documented in many studies, but a study from the Department of Neurology at National Taiwan University Hospital showed that deprenyl can also protect (and/or rescue) brain neurons by suppressing hydroxyl (OH) free radicals generated by MPP+ in male Sprague-Dawley rats.23 Hydroxyl radicals are the most toxic radicals known, and are capable of destroying many types of neurons. The study also showed that deprenyl prevents the age-related deposition of neuromelanin in neurons. Neuromelanin is caused by the accumulation of cellular debris. Deprenyl Prevents Cell "Suicide"Another powerful neurotoxin which can be neutralized by deprenyl is 6-hydroxydopamine (6-OHDA),7 which, in contrast to MPTP, is a non-selective destroyer of neurons, but seems to focus most on dopaminergic neurons. Many studies have shown that 6-OHDA can cause massive brain lesions in the substantia nigra when administered to animals in the laboratory. In one study at the University of Manchester School of Biological Sciences in England, scientists showed that 6-OHDA can induce neuronal cell death via a mechanism that has all the earmarks of apoptosis, the method by which neurons die "naturally" during growth and development-a process that's been labeled cell "suicide". 24 Neurons that die from this process exhibit cell shrinkage, chromatin condensation, and membrane disintegration. Scientists have hypothesized that the endogenous formation of 6-OHDA could play a role in the damage to dopaminergic neurons in Parkinson's disease While there is not yet experimental evidence to substantiate this hypothesis, several of the chemical intermediaries in the pathways between dopa, dopamine, and norepinephrine are very similar in structure to 6-OHDA. Deprenyl Protects Against DSP-4 ToxicityDSP-4 [N(2-chloroethyl)-N-2-bromobenzylamine] is a potent, highly selective neurotoxin that induces long-lasting depletion of the essential neurotransmitter noradrenaline and inactivates the essential intra- and interneural messenger nitric oxide, which subsequently leads to cell death. In a recent study in Brain Research, scientists in the Neuropsychiatry Research Unit at the University of Saskatchewan in Canada found that deprenyl protected noradrenergic neurons in the hippocampal dentate gyrus of rats against these types of damage.25 Rescue Of Dying NeuronsIn a series of cell culture experiments, W.G.Tatton and associates at the Centre for Research on Neurodegenerative Disorders at the University of Toronto demonstrated that very low doses of deprenyl can rescue dying neurons in tissue culture and laboratory animals via a different mechanism than inhibition of MAO-B.13-15 In one experiment, the Toronto scientists showed that deprenyl can protect substantia nigra neurons in mice from the killing effects of MPTP at doses too low to block the conversion of MPTP to MPP+.13 In another experiment, they showed that deprenyl can prevent the death of axotomized motoneurons in immature rats. T hey found that deprenyl treatment (10 mg/kg every second day) increased by 2.2 times the number of motoneurons surviving 21 days after surgical separation of the neurons from their muscle targets. The Canadian scientists proposed a mechanism of action for this effect and speculated about its clinical implications: "This study suggests that deprenyl has the capacity to activater some mechanisms which compensates for the loss of target-derived trophic agents. This does not that deprenyl acts a trophic agent, but rather that it somehow reduces the impact of the trophioc loss on the motoneurons. Part of the action of deprenyl in neurodegenerative diseases may reflect a similar compensation for may also suggest a role for deprenyl in treatment of motoneuron death in conditions like amytrophic lateral sclerosis (Lou Gehrig's disease) of after peripheral nerve trauma which damages axon"14 In a later study, they found that concentrations as low as 10 increased the growth of dopamineragic period. They speculated that "these newly discovered 'trophic-like actions of selegiline may involve a high affinity sterospecific interaction with an unknown protein."15
|
 |
Effect Of Long-Term Deprenyl Treatment On Age-Dependent Changes In The Rat Brain |
Recently, scientists at the Camerino in Italy explored the effects of deprenyl treatment on age-related microanatomical changes in the brains of male Sprague-Dawley rats. Deprenyl was given by subcutaneous injection in two doses (1.25 mg/kg/day and 5 mgfl daily) for 5 months (from 19-to- 24-months of age), with age-matched untreated rats used as controls and Il-month-old rats used as an adult reference group 25-26 They found that the number, den- density, and metabolic activity of neurons and glial cells were decreased with age in untreated rats in the hipocampus (which plays a key role in learning and memory), the frontal cortex (which is involved in information processing), and the cerebellar cortex (which coordinates movement and balance). They also observed that deprenyl (at 5 mg, but not 1.25 mg) prevented the decline in neuronal activity in certain areas of the brain, but not in others. The drug was particularly effective in preserving hippocampal neurons and Purkinje neurons in the cerebellar cortex. The lower dose of deprenyl (1.25 mg/kg/day), which did not affect MAO-B activity, prevented the age-related buildup of aging pigment (lipofuscin), but did not prevent the loss the neurons. Their conclusion was that "treatment with L-deprenyl is able to counter some microanatomical changes typical of the aging brain. Some of these facts are probably not related to the inhibitory MAO-B activity of the compound." 26 Deprenyl Boosts SOD And Catalase LevelsDeprenyl has antioxidant properties, but it can also boost levels of the body's own antioxidant enzymes superoxide dismutase (SOD) and catalase in the brains of laboratory rats. The studies demonstrating these effects were conducted by M.C. Carrillo and associates at the Tokyo Metropolitan institute of Gerontology in Japan. 27-28 The Japanese scientists gave 6- month-old Fisher-344 rats daily sub- cutaneous injections of 2 mg/kg of deprenyl for 3 weeks, while control animals received saline injections. They found a 300% increase in SOD and a 60% increase in catalase in the substantia nigra, but not in the hippocampus or cerebellum. They noted that: Effect Of Deprenyl On Nigral Neurons In Parkinson's DiseaseAlthough the tissue culture and animal studies suggesting that deprenyl has a neuroprotective effect on brain neurons are impressive, none of them provide direct evidence of the effect of deprenyl on neurons in the brains of Parkinson's patients. There is one study, however, by researchers at the University of Turku in Finland, that speaks volumes on the subject.29 Since substantia nigra neurons are destroyed in Parkinson's disease and the pathologic hallmark of the disease is neural lesions called Lewy bodies, the Finnish scientists studied a randomly selected sample of 25 brains from patients who had died of Parkinson's disease. Ten of the 25 patients had received P deprenyl and L-Dopa and 15 had received L-Dopa alone. They then counted the neurons and Lewy bodies in the medial section of the substantia nigra of all 25 brains. They found that:
Deprenyl Improves Learning And Memory |
 |
Deprenyl Improves Learning And Memory |
Several animal studies have shown that both deprenyl (and its metabolite 1-amphetamine) improves learning and memory. In one study at the University of Saskatchewan in Canada, both young (2-month old) and middle- aged (10-month old) male Wister rats were tested on a modified Morris Water Maze. Every animal went through ten trials a day for five consecutive days.30 The middle-aged deprenyl-treated animals learned the maze in an average of only 11 trials compared to 19 trials for the control animals. The middle-aged deprenyl rats even did better than the young controls, who took an average of 13 trials to learn the maze. In the April 1996 Progress in Neuropsychopharmacology & Biological Psychiatry , 31 scientists from the University of Toronto showed that the oral administration of deprenyl in doses of 0.5 and 1.0 mg/kg improved the performance of old but not young dogs on a spatial memory task. These findings are supported by studies using recognized neuropsychological test batteries, which show that deprenyl treatment (10 mg/day) improves learning and memory in Alzheimer's patients. The value of deprenyl as a treatment for Alzheimer's disease is currently being evaluated in large clinical trials. Was The Dose Of Deprenyl Too High?One explanation for the excess mortality in the patients receiving deprenyl and L-Dopa in the British study may be that the 10 mg/day of deprenyl they received may have been too high when combined with L-Dopa. Here are some findings that suggest this:
It could be that the combination of deprenyl and L-Dopa in the absence of very many functioning dopaminergic neurons, results in an excessive amount of dopamine in the brain, which becomes toxic to substantia nigra neurons, and which, in turn, leads to the further dysfunction of the remaining neurons, thus hastening disability and death. Evidence For The Toxicity Of DopamineDopamine is one of the most important substances in the brain. It is an essential neurotransmitter that regulates movement, coordination, sex drive, and other critical functions. The lack of it causes Parkinson's Disease, which leads to disability, cognitive decline, and death. However, an excess of dopamine can also be harmful. Researchers have found that one of the byproducts of dopamine metabolism is hydrogen peroxide, which is relatively inert and not toxic to cells.37 However, damage occurs when hydrogen peroxide interacts with the reduced forms of iron and copper, which causes it to decompose to highly damaging hydroxyl free radicals,38 which react with almost every molecular species found in living cells. Such reactions can cause breakage of single- and double-stranded DNA, chemical alteration of purine and pyrimidine DNA bases, and membrane disinte- gration. These events, in turn, lead to damage to the mitochondrial energy system, and excessive release of degradative enzymes, leading to the crippling of cell function and, eventually, to cell death. 39 Although there is not yet proof that this type of damage causes the loss of dopaminergic neurons in Parkinson's disease, there is evidence in animals and humans supporting the concept. This includes abnormally high iron deposits and abnormally low levels of reduced glutathione in the brains of Parkinson's patients as well as significant increases in the secondary products of lipid peroxidation, and a 10-fold increase in lipid hydroperoxides in the substantia nigra of Parkinson's patients.39 Evidence For The Toxicity Of L-DopaA number of studies provide evidence that the dopamine precursor, L-Dopa, is tordc to neurons in both tissue culture and animals.40 In a tissue culture study at the Hospital Ramon y Cajal in Madrid, Spain, incubation with low dose L-Dopa was highly toxic to dopaminergic rat brain neurons.41 Scientists at the University of Manchester in England found that "clinically applicable" doses of L-Dopa caused the death of catecholaminergic cells in vitro by inducing apoptosis (cell "suicide").42 At the University of Virginia Medical School, neurologists found excessive hydroxy radical formation and inhibition of energy production in the substantia nigra of rats given L-Dopa.43 In an in vitro study with L-Dopa study at Mt. Sinai Medical Center in New York, neurologists found "reduced neurite length and overall deterioration" in rat brain neurons, with evidence of greatest toxicity in dopaminergic neurons. 44 Scientists at the Washington University School of Medicine in St. Louis proposed that "an excitotoxic process mediated by L-Dopa or an acidic derivative such as 6-OH-DOPA might be responsible for degeneration of neurons in Parkinson's disease or striatal neurons in Huntington's disease." 45 What Is The Right Dose Of Deprenyl For Parkinson's Disease?When treating Parkinson's patients with L-Dopa, doctors adjust the dose according to their patients' needs. In doing so, they try to give the lowest possible dose of L-Dopa consistent with its therapeutic benefits because of the adverse side effects of the drug. This is the procedure that was followed in the British and DATATOP studies. Until recently, it was assumed that the appropriate dose of deprenyl for all Parkinson's patients is 10 mg/day. Now that the findings of the and DATATOP studies have tioned the safety and efficacy deprenyl, the possibility that 10 mg/day of deprenyl may be too for some patients must be too high for some patients must considered.
|
 |
Evidence For The Efficacy Of Low-Dose Deprenyl |
| The experiments of Tatton, et al. the University of Toronto 13-15 provide significant evidence that deprenyl's ability to protect and rescue dying neurons may take place at well below that required for MAO-B inhibition though an entirely different mechanism of action, which Toronto scientists believe involves "trophic-like" activity in surrounding reactive astrocytes. In a recent paper, they concluded that: "Neuronal rescue by selegiline could contribute to the reported slowing the progression of Alzheimer's disease and Parkinson's disease and should be possible at markedly lower doses than those required to provide neuroprotection through MAO-B inhibition"15 Further evidence for the desirability of lower doses of deprenyl in Parkinson's patients comes from Saskatchewan study,30 in which l-deprenyl and its metabolite l-amphetamine produced enhancing benefits in middled rats. The investigators concluded that-since l-amphetamine was able to produce the same cognitive benefits as deprenyl without MAO-B activity-then "MAO-B inhibition is not necessary for the cognitive enhancement or the protection against the aging related decline in cognitive function such as that seen after chronic L-deprenyl." Current RecommendationsThe Foundation now recomends a lower dose of deprenyl for Parkinson's patients and for antiaging purposes based upon the evidence presented in this article. We recommend that healthy, aging persons take no more than 10 mg of deprenyl per week, and that untreated, early-stage Parkinson's patients take the lowest dose of deprenyl that produces symptomatic relief (1.5 mg-to-l0 mg a day), with the dose of deprenyl reduced or eliminated as the patient moves into the latter stages of the disease. We believe the same strategy should be probably be used in Alzheimer's patients, but await the results of Alzheimer's trials now in progress, which will provide further evidence on the use of deprenyl in such patients. Parkinson's and Alzheimer's patients must be under the care of a doctor, preferably a specialist in treating these diseases. Parkinsonism: An Energy Deficiency DiseaseOne of the characteristics of exposure to neurotoxins is depletion of energy-generating capacity in the mitochondria (the power plants of the cell), especially in Complex I, the largest of the energy chain components, which uses NADH (Nicotinamide Adenine Dinucleotide) in the initial phase of energy production 45 NADH is absolutely critical for the production of energy within our cells. For every molecule of NADH that enters the energy chain, 3 molecules of ATPe energy currency) are produced: There is now solid evidence of seriously impaired energy function in NADH-dependent Complex I due to mitochondrial abnormalities in Parkinson's patients. In one study, there was a 37% decline in Complex I energy function in 17 patients with Parkinson's disease compared to 22 age-matched controls. 47 NADH Therapy For Parkinson's DiseaseThere are studies showing that NADH levels are diminished significantly in Parkinson's patients and that NADH supplementation can stimulate the synthesis of dopamine. Clinical studies in Europe have demonstrated in more than 2,000 early-stage Parkinson's patients that NADH therapy can produce clearcut clinical benefits in up 78.2% of the patients. 48 The amount of NADH used varied according to the severity of the disease. Positive results were also obtained with NADH therapy in Alzheimer's patients. 49 (For an in-depth article on NADH, see the June 1996 issue of LIFE EXTENSION Magazine). Neurotrophic Factors In Parkinson's DiseaseRecent evidence that deprenyl may be able to protect neurons via "trophic-like" effects is indicative of a new approach to the treatment of Parkinson's (and other neurodegenerative diseases)-the use of neurotrophic (growth) factors to stimulate the activity, regeneration, and revitalization of existing neurons in the brain. Until recently, the only such factor that was considered to be important for the health and vigor of brain neurons is Nerve Growth Factor (NGF), but there are now several other factors that are under investi- gation as neurotrophic factors. These include Brain-Derived Neuro- trophic Factor (BDNF), Ciliary Neurotrophic Factor (CNF), and Mitogenic Growth Factors (MGF). There are many studies showing that these growth factors promote the survival and differentiation of nigral dopaminergic neurons and that they protect these neurons from neurotoxic damage.50 Clinical Trials And PracticeThe research with neurotrophic growth factors has reached the point where clinical trials are being initiated in both Parkinson's disease and ALS (Lou Gehrig's disease) by companies such as Regeneron Pharmaceuticals, Synergen, Cephalon, and Amgen.50 One of the Mitogenic Growth Factors being studied as a therapy to regenerate dopaminergic neurons are the insulin growth factors (IFG-1 and IGF-2). Of interest is the fact that IGF-1 is the major metabolite of growth hormone, which is now being used clinically (with other hormones) in attempts to restore lost youth and vigor in healthy, aging persons. Hormone replacement therapy is being investigated for rejuvenation purposes in the U.S., England, Sweden and Denmark. There also is a clinic in the midwest that has reported remarkable results with hormone replacement therapy in Parkinson's, Alzheimer's and Stroke patients. We will be carrying in-depth reports about the latest developments in hormone replacement therapy-- both for neurodegenerative diseases and for aging--in future issues of LIFE EXTENSION MAGAZINE. The Need For New Brain CellsThe major limitation of today's therapies is the fact that they only affect the functioning neurons that remain in the brain of Parkinson's patients. Since 70-80% of the dopaminergic neurons in the substantia nigra of Parkinson's patients have been destroyed by the time the disease is diagnosed, even a therapy that prevents further loss of neurons would not cure the disease. The long-term answer to Parkinson's disease and other neurodegenerative disease's will be the provision of new cells to replace the ones that have been lost. For the past 15 years, there have been promising animal studies using fetal brain grafts to attempt to replace critical neurons. There has also been limited experimentation in humans using this technique, but the result of theis reaserch have not been good enough to warrant its routine use in clinical practice. We will reporting on the latest advances in this field in a future issue of the magazine. Our conclusion about deprenyl is that on balance, it is still a useful drug for Parkinson's disease and for antiaging purposes, but that it should be used at lower doses than previously recommended under the close supervision of a doctor. We will continue bringing you updates on deprenyl and other anti-Parkinson's therapies as the research picture unfolds. |
| References |
1 Lees AJ, Comparison of therapeutic effects and mortality data of levodopa and levodopa combined with selegiline in patients with ealry, mild Parkinson's disease, British Medical Journal 311:1602-1607, December 1995. 2 Sweet RD, McDowell FH, Five years' treatment of Parkinson's disease with levadopa, Annals Intern Med., 83:456-463, 1975. 3 Hornykiewicz O, Brain transmitter changes in Parkinson's disease, in Movement Disorders, eds CD Marsden and Fahn, Butterworth & Co., London, p41, 1982 4 Knoll J, the striatal dopamine dependency of life span in male rats. Longevity study with (-) deprenyl, Mech. Ageing Dev, 46:237-262, 1988. 5 Knoll J, Dallo J, Yen TT, Striatal dopamine, sexual activity and lifespan. Longevity of rats treated with (-)deprenyl. Life Sci. 45:525-531, 1989. 6 Coehn G, Pasik P, Cohen B, et al. Pargyline and deprenyl prevent the neurotoxicity of l-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in monkeys, Eur J Pharmacol, 106:209, 1984. 7 Knoll J, Dallo J, Yen TT, Striatal dopamine, sexual activity and lifespan. Longevity of rats treated with (-)deprenyl. Life Sci. 45:525-531, 1989. 8 Brikmayer W, Knoll J, Riederer P, et al. Increased life expectancy resulting from addition of L-deprenyl to madopar treatment in parkinson's disease: A long termstudy, J Neural Transm, 64:119-127, 1985. 9 Parkinson Study Group, Effect of deprenyl on the progression of disability in early Parkinson's disease, New Engl J Med, 321:1364-1371, 1989. 10 Elsworth JD, Glover V, Reynolds GP, et al. Deprenyl administration in man: selective monoamiline oxidase B inhibitor without the "cheese effect", Psychopharmacology, 57:33-38, 1978. 11 Robinson DS, Changes in monoamine oxidase with human development and aging, Fed Proc, 34:103-107, 1975. 12 Tipton KF, What is it that L-deprenyl (selegiline) might do? Clin Pharmacol Ther, 56:781-796, 1994. 13 Tatton WG and greenwood CE, rescue of dying neurons: a new actionfor deprenyl in MTPT Parkinsonism, J Neurosci Res, 30:P666-672, 1991. 14 Salo PT and Tatton Wg, Deprenyl reduces the death of motoneurons caused by axotomy, J Neurosci Res, 31:394-400. 15 Tatton WG, Ansari K, Ju W, et al. Selegiline Induces "Trophic-Like" Rescue Of Dying Neurons Without MAO Inhibition, Neurochemistry in Clinical applications, eds. Tang L and Ynag S,. p. 15-16, Plenum Press, NY 1995. 16 Olanow CW, the early treatment of parkinson's disease, Neurology, 43 (suppl): S1-30-S1-31, 1993. 17 Mangoni A, Grassi MP, Frattola L, et al. Effects of a MAO-B inhibitor in the treatment of Alzheimer disease, Eur Neurol, 31: 100-107, 1991 18 Maki-Ikola O, Kilkku O, Heinonen E. Effect of adding selegeline to levodopa in early, mild Parkinson's disease. Other studies have not shown increased mortality (letter). BMJ. 1996 Mar 16; 312(7032):702. 19 Maki-Ikola; O,Kilkku O, Heinonen, E, Other studies have not shown increased maortality (letter), British Medical Journal, 312:702, March 1996. 20 Parkinson Study Group, Impact of Deprenyl and Tocopherol Treatment on Parkinson's Disease in DATATOP subjects not patients Requiring Levodopa, Annals of Neurology, 39:1:37-43, January 1996. 21 Parkinson Study Group, Impact of Deprenyl and Tocopherol Treatment on Parkinson's Disease in DATATOP subjects patients Requiring Levadopa, Annals of Neurology, 39:1:37-43, January 1996. 22 Anderson KB, Girdwood AG, WilsonJa, Stopping selegiline may lead to problems for patients (letter), British Medical Joiurnal 312:702, 16 March 1996. 23 Wu,R-M, Chuich CC, Pert A, et al. Apparent antioxidant effect of L-deprenyl on hydroxyl radical formation and nigral formation and nigral injury elicited by MPP+ in vivo, Eur J of Pharmacol, 243:241-247, 1993. 24 Walkinshaw G and Waters CM, Neurotoxin-induced cell death in neuronal PC12 cells is mediated by induction of apoptosis, neuroscience, 63:4:975-987, December 1994. 25 Zhang X and Yu PH, Depletion of Nos Activty in the rat Dentate Gyrus neurons by DSP-4 and protection by Deprenyl, Brain Research Bulletin, 38:4:307-311, 1995. 26 Zeng TC, BongraninS, Bronzetti E, et al. Influence of longterm treatment with L-deprenyl on the age-dependent changes in rat brain micrpanatomy, Mech Ageing Dev, 73:2:113-126, February 1994. 27 Carrillo MC, Kanai S, Nokubo M, et al. (-) Deprenyl induces activities of both superoxide dismutase and catalse but no og glutathanione peroxidae in the striatum of young rats, Life Sci, 48:517 521,1991 28 Carrillo MC, Kanai S, Nokubo M, et al. The ability of (-) deprenyl to increase suoperoxide dismutase activities in the rats ids tissue and brain region selective, Life Sci, 50:1985-1992, 1992 29 Rinne JO, Roytta M, Paljarvi L, et al. Selegiline (deprenyl) treatment and death of nigral neurons in Parkinson's disease, Neurology, 41:859-861,June 1991. 30 Gelowitz, DL Richardson JS, Wishart TB, et al. Chronic L-deprenyl or L-Amphetamine: Equal Cognitive Enhancement, Unequal MAO Inhibition, Pharmacology Biochemistry and behavior, 47:41-45, 1994 31 Head E, Hartley J, Kameka AM, et al. The effects of L-deprenyl on spatial, short term memory in memory in young and ages dogs, Progress in Neuropsychopharmacology & Biological Psychiatry, 20 : 3:515-530, April 1996 32 Knoll J, Deprenyl (selegiline): the history of its development and pharmacologiacl action. Acta Neurol Scand, 68 (Suppl 95) : 57-80, 1993 33 Elizan TS, Yahr MD, Moros DA, et al. Selegiline use to prevent progression of Parkinson's disease, Arch Neurol, 46:1275-1279, 1989. 34 Shaw KM, Lees AJ, Stern GM, The impact of treatment with levadopa on Parkinson's disease, Quar J Med 195:283-293 1980. 35 Chiueh CC, Wu RM, Mohanakumar KP, et al. In vivo generation of hydroxyl radicals and MPTP-induced dopaminergic toxicity in the the basal ganglia, Ann NY Acad.Sci, 738:25-36, Nov 17, 1994 36 Michel PP, Hefti F, Toxicity of 6-hydroxydopamine and dopamine for dopaminergic neurons in culture, J Neurosci Res, 26:4:428-33, August 1990. 37 Halliwell B, Reactive oxygen species and the central nervous system, J Neurochem, 59:1609-1614,1991. 38 Dorit B-S, Riederer P, Youdim MBH, Iron-Melanin Interaction and Lipid Peroxidation: Implications for Parkinson's disease, J Neurochem, 57:5:1609-1614, 1991. 39 Gerlach M, Riederer P, Youdim MBH, Neuroprotective Therapeutic Strategies: Comparison of Experimental and Clincal Results, Biochem Pharmacol, 50:1:1-16, 1993. 40 Zigmond MJ, Hastings TG, Abercrombie ED, Neurochemical responses to 6-hydrodopamine and L-Dopatherapy: implications for Parkinson's Disease, 648:71-86, May 11, 1992. 41 Pardo B, Mena MA, Casarejos MJ, et al. Toxic effects of L-Dopa on mesencephalic cell cultures: protection with antioxidants, Brain Res, 682:1-2:133-143, June 5, 1995. 42 Walkinshaw G and Waters CM, Induction of apoptosis in catecholaminergic PC12 cells by L-DOPA: Implications for the treatment of Parkinson's Disease. 43 Smith TS, Parker WD Jr, Bennnett JP, L-Dopa increases nigral production of hydroxyl radical in vivo: potential L-Dopa toxicty?, Neuroreport, 5:8:1009-1011, April 14,1994. 44 Mytilineou C, Han Sk, Cohen G, Toxic and protective effects of L-Dopa on mesencephalic cell cultures, J Neurochem, 61:4:1470-1478, October 1993. 45 Excitology of L-dopa and 6-OH-dopa: implications for Parkinson's disease and Huntington's disease, Exp Neur, 108:3:269-272, June 1990. 46 Wilson DF, Factors affecting the rate and energetics of mtiochondrial oxidative phosphorylatiobn, Med Sci Sports Exer, 26:1:37-43. 47 Cooper JM, Daniel SE, Marsden CD, et al. L-Dihydroxyphenylalanine and complex I deficiency in Parkinson's disease brain Mov Disord, 10:3:295-297, May 1995. 48 Birkmayer JG, Vrecko C, Vole D, et al. Nicotinamide adenine dinucleotide (NADH)- a new therapeutic approach to Parkinson's disease, a comparison of oral and parenterl application, Acta Neurol Scnad Suppl, 146: 32-35, 1993 49 Life Extension Magazine®, p.23-31, June 1996. 50 Lindsay RM, Altar CA, Cedarbaum JM et al. The therapeutic Potential of Neurotrophic Factors in the Treatment of Parkinson's disease, Exp Neurol, 124:103-11, 1993 |