Sleep Hacking
Sleep Hacking
Last Section Update: 12/2024
Contributor(s): Maureen Williams, ND; Shayna Sandhaus, PhD; Cristina Mathewman, PhD; Chancellor Faloon, Health & Wellness Author; Stephen Tapanes, PhD
1 Introduction
Sleep is vital for every aspect of human health. Adults generally need seven to nine hours per night.1,2 The importance of adequate sleep has been born out in extensive research, and most people are now aware that regularly getting enough quality sleep helps prevent various chronic diseases. Better sleep quality has even been linked to slower biological aging, while chronically sleeping too much or too little has been associated with a shorter lifespan.3-5
Perhaps less well appreciated is that suboptimal sleep undermines the performance of the human mind and body.6,7 For instance, inadequate sleep correlates with worse grades and lower likelihood of graduation among college students.8 Suboptimal sleep also undermines individuals’ work performance—and when extrapolated across populations, the economic performance of businesses and nations.9-11 In fact, Deloitte, a business consultancy firm, has described sleep as “the ultimate performance enhancer.”10
And yet, one in three U.S. adults report sleeping less than seven hours per 24-hour period.12,13 This means that one-third of adults may stand to improve their cognitive and physical performance by sleeping more and better.
This Protocol should interest the one in three adults who do not get optimal sleep and who may be underperforming their well-rested peers as a result. Anyone who gets “enough” sleep, but nevertheless wants to improve the quality of their sleep (and thereby potentially enhance their quality of life and performance), may be interested in reading this Protocol as well.
In this Protocol, we will summarize the scientific evidence related to various means of improving sleep quantity and/or quality. In general, we have attempted to focus on scientific evidence derived from studies in which the participants were generally healthy. While overt sleep disorders like insomnia and sleep difficulties due to serious underlying diseases are not addressed in detail here, this Protocol provides tips and strategies for people who may have some room to improve their sleep regimen. We call this approach Sleep Hacking.
2 Understanding Healthy Sleep
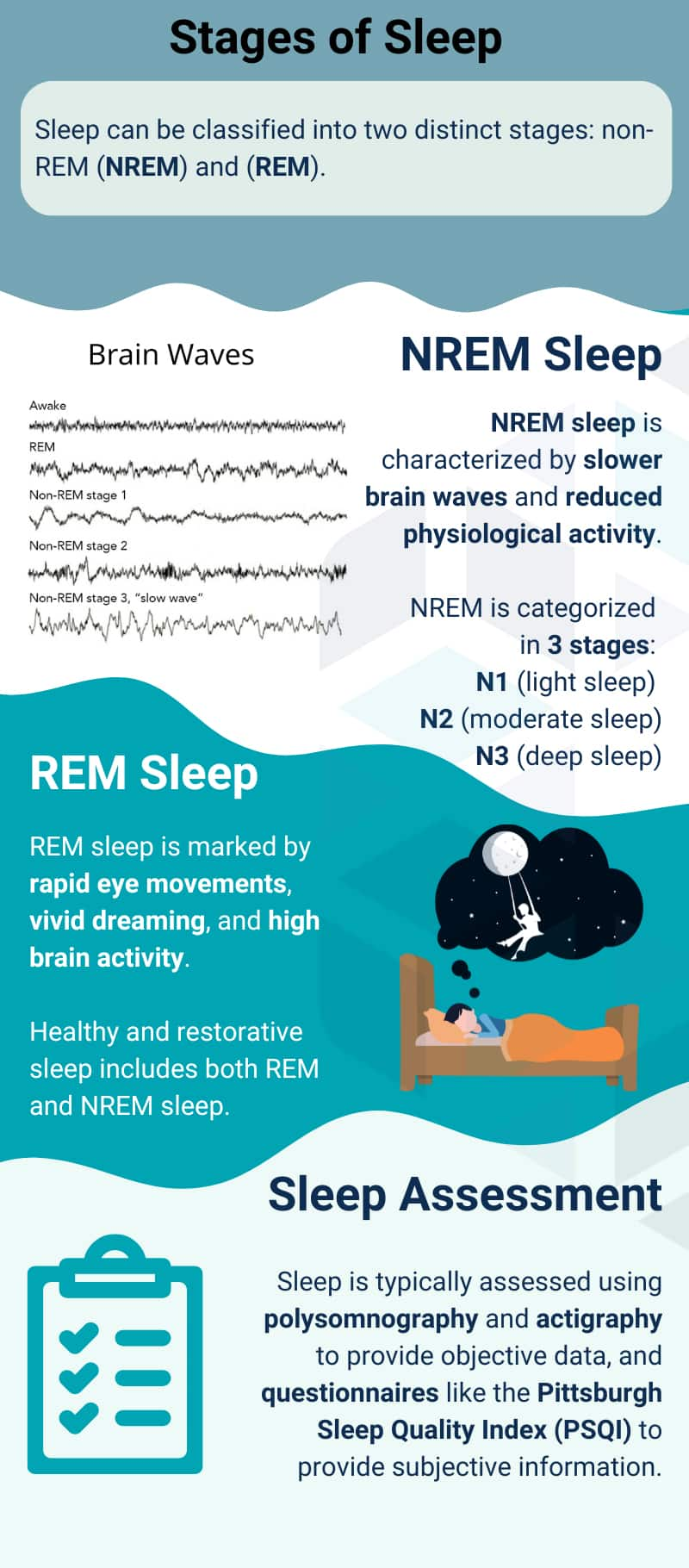
The Stages of Sleep
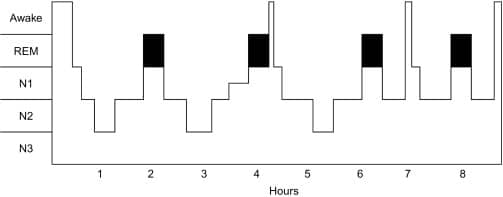
Sleep has two distinct stages that occur cyclically and are marked by different types of brain activity: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. On a typical night, sleep consists of three to six NREM-REM cycles, lasting about 90–120 minutes each and sometimes interrupted by short bouts of wakefulness (Fig. 1).14,15 Healthy, restorative sleep includes both NREM and REM sleep.16
The drive to sleep is normally initiated by the body’s internal circadian clock. On an electroencephalogram (EEG)—a tool used during a sleep study for measuring brain electrical activity—the process of falling asleep appears as a gradual transition from predominantly small, high-frequency waves to larger, slower waves. This shift marks the progression from wakefulness to deep sleep stages. During REM sleep, however, the EEG shows a return to smaller, high-frequency waves, reflecting a more active brain state despite the body remaining at rest.14,16
NREM sleep represents about 75–80% of total sleep time and is characterized by reduced responsiveness to internal and external stimuli, decreased core body and brain temperatures, lower muscle tone, and slower breathing and heart rates. NREM sleep itself is categorized in three stages based on brain wave activity15,16:
- Stage 1 (N1) is when the body is transitioning to sleep. Heartbeat, eye movement, and brain waves begin to slow down.16 Sometimes muscle twitches (“hypnic jerks”) occur during this sleep stage, which lasts only a few minutes, representing 2–5% of total sleep time.15
- Stage 2 (N2) involves deepening of sleep, with a higher threshold for waking, further slowing of heart and breathing rates, and reductions in temperature and muscle activity.14 Short bursts of brain activity (electrical events known as sleep spindles and K-complexes) occur throughout N2 and play a role in keeping us asleep, building memory, and toning brain function.16 Ideally, about 45–55% of total sleep time is spent in N2.15 N2 and N1 sleep are sometimes referred to jointly as core sleep.
- Stage 3 (N3), known as deep or slow-wave sleep, is the most difficult to awaken from. Deep sleep is believed to be important for tissue regeneration and repair, as well as metabolic and immune regulation, hormone balance, and memory.16,17 Most slow-wave sleep occurs in the first few sleep cycles.18 Its duration generally makes up 13–23% of total sleep time in younger adults, but diminishes with age and may be absent in elderly individuals.15
A normal sleep cycle involves gradual transitioning through N1, N2, and N3. Deep sleep then gives way to lighter N2 sleep and finally a period of REM sleep (Fig. 1).15
REM sleep generally occurs in 10–20-minute episodes at the end of sleep cycles, accounting for 20–25% of total sleep time. It is characterized by rapid jerky eye movements and brain electrical activity similar to awake time.16 REM sleep appears to be a time of intellectual and emotional processing, with vivid dreaming as well as muscle twitching and fluctuations in breathing and heart rate.14-16 In contrast with deep sleep, periods of REM sleep tend to become longer with each successive sleep cycle throughout the night.15,16 REM sleep concludes with a return to N1, sometimes with a brief period of wakefulness prior to the next sleep cycle.15
Figure 1: Example of Normal Sleep Architecture
Opportunities for Sleep Optimization: Falling Asleep & Staying Asleep
For many people reading this overview, opportunities to leverage sleep optimization to enhance performance will center around one of two themes, or sometimes both—making it easier to fall asleep or stay asleep.
The length of time it takes to fall asleep initially upon trying is called sleep latency. Normal sleep latency for adults is about 10 to 20 minutes.20 Longer sleep latency over a prolonged period has been associated with cardiovascular health concerns like decreased heart variability and increased blood pressure.21,22
Similarly, chronic trouble staying asleep is linked with several health problems as well.23-25
If you experience frequent (three or more nights per week) trouble falling asleep or staying asleep over a long period of time (three months or longer), you should consult your doctor and ask about an insomnia evaluation.26-28
This overview is not intended to be a resource for people with overt insomnia. Instead, people who experience occasional sleep trouble and/or feel they could benefit from taking steps to optimize their sleep are those for whom sleep hacking is a reasonable framework. Interestingly, research has suggested that sleep performance lies on a continuum ranging from self-identified good sleepers to overt insomniacs, with self-reported poor sleepers falling somewhere in between. Sleep hacking is a reasonable initial approach for those who feel they are poor sleepers but not those who experience severe debilitation due to insomnia.27
Sleep Quantity & Quality
For most adults, seven to nine hours of sleep per night is recommended to optimize health and lower the risks of chronic diseases.1,2 Importantly, healthy sleep is marked not only by sufficient quantity, but also good quality and appropriate timing.36 For instance, a study using accelerometer-derived sleep data from almost 104,000 UK Biobank participants over a period of seven days found that sleep onset time between 10:00 p.m. and 10:59 p.m. was associated with the lowest incidence of cardiovascular disease.37
Sleep health is a multi-dimensional concept that lacks a consistent definition, but can be thought of as sleep-related well-being that is more than simply the absence of sleep pathology.38,39 The following parameters are important to consider when evaluating sleep health36,40:
- Duration: the amount of time asleep. In general, seven to nine hours of sleep per night is optimal for supporting good overall health in most adults.41
- Efficiency: the ease of falling and returning to sleep, measured as the proportion of intended sleep time that is actually spent sleeping. Sleep efficiency decreases with aging, and poor sleep efficiency may be a more important marker of health risks in elderly individuals than low sleep duration. Since sleep efficiency of less than 80% (ie, awake >20% of time in bed) has been correlated with poor health outcomes and increased mortality,42 a common target for sleep efficiency is 85%.43
- Timing: the placement of bedtime and awakening time within the 24-hour day. Our internal circadian clock regulates rhythms of wakefulness and sleep, as well as cardiovascular, digestive, metabolic, and immune functions, and coordinates them with environmental cues such as cycles of light and darkness.44 Synchronizing sleep with circadian rhythms is especially important for cardiometabolic health.39,44
- Regularity/Variability: day-to-day variability in the sleep-wake schedule. Irregular sleep patterns promote circadian de-synchronization, inflammation, nervous system and stress response dysregulation, and gut microbiome disruption, taking a toll on cardiometabolic and overall health. On the other hand, consistent sleep patterns appear to support optimal health. For example, sleep patterns that do not vary by more than 30 to 60 minutes each day have been linked to better cardiovascular health.45
- Satisfaction: the subjective assessment of sleep quality. This includes how one feels about their sleep immediately upon waking and throughout the following day, and may be based on such considerations as how one judges their comfort while sleeping, their ability to fall asleep, the ease with which they fall back to sleep, and the duration of their sleep.46 In one study that included 109 university students, higher sleep satisfaction was more closely aligned with positive mood, sense of well-being, and life satisfaction than objective measures of sleep quality.47
- Alertness/Sleepiness: the ability to remain attentive during waking hours. Excessive daytime sleepiness has been correlated with increased risks of cardiovascular disease and cognitive dysfunction, as well as poorer mental and physical performance and higher risk of accidents.48-52 On the other hand, alertness is associated with better mood and cognitive, mental, and physical performance.53
3 Assessing Your Sleep
Both objective and subjective measures are important parts of a comprehensive sleep assessment. Sleep is typically assessed using polysomnography and actigraphy to provide objective sleep data and questionnaires to provide subjective information.
Polysomnography - The Sleep Study
When any type of sleep disorder is suspected, a diagnosis can be ascertained using polysomnography, also known as a sleep study. Polysomnography is the “gold standard” test in research studies that evaluate the effect of various interventions on sleep architecture and sleep parameters. It combines recordings of brain waves, eye movements, breathing patterns, and heart function to provide insight into body and brain activity during sleep. Polysomnography is generally performed in a supervised setting such as a sleep clinic.54 The components of polysomnography can vary, but typically include54,55:
- Electroencephalography (EEG) to measure brain electrical activity and thereby evaluate sleep architecture
- Electrocardiogram (ECG) to monitor heart electrical activity
- Electro-oculography (EOG) to detect eye movements and provide further information about REM and other sleep stages
- Electromyography (EMG) to provide information about muscle tension and limb movements
- Airflow sensors to assess the movement of air through the nose and mouth to detect episodes of apnea (paused breathing) or hypopnea (shallow breathing) and other disordered breathing patterns
- Pulse oximetry to measure blood oxygen levels and help detect correlations between oxygen levels, breathing, and arousals during sleep
- Plethysmography to monitor respiratory mechanics
- Video and sound recordings to detect sleep position and sleep events such as nightmares or night terrors, sleep talking or walking, and other sleep movements and sounds
After this data is collected, it is synthesized and analyzed in short time frames. Time needed to fall asleep, wakefulness after sleep onset, number and duration of arousals, early morning waking, and total sleep time can be ascertained, and sleep efficiency can be calculated. In addition, the amount of time spent in each sleep stage and frequency of events such as apneas or limb movements can be seen.55
Despite its comprehensive nature, polysomnography’s usefulness is still limited in that it shows only a one- to two-night “snapshot,” which may miss sleep problems that occur intermittently.54 It is also cumbersome, expensive, and removes the patient from their natural sleep environment, such that the test procedure itself may interfere with normal sleep patterns. Home-based units that allow a patient to sleep in their own bed, can be used for multiple consecutive nights, and do not require an attendant are sometimes an option for clinically assessing sleep architecture, but do not provide the comprehensive assessment of a lab-based sleep study.56 Home-based sleep studies may be reasonably accurate for many people. However, those who have many other health conditions or who think their at-home results might be inaccurate should consider a lab-based sleep study.57
Actigraphy
Actigraphy is an objective method of monitoring rest and activity cycles by collecting data about body movement via a wearable device, such as on a wristband, that measures acceleration.58 The actigraphy device can be worn day and night for long periods of time to provide an overview of a range of sleep and activity parameters. It has the advantages of being easy to use, non-invasive, and lower in cost than polysomnography, but does not directly measure sleep, and does not include data regarding sleep architecture or breathing abnormalities.59-61 Although actigraphy has been shown in multiple studies to reasonably reflect sleep-wake cycles, compared with polysomnography, it tends to overestimate total sleep time and is more likely to be inaccurate in individuals with poor sleep. This is mainly because it cannot distinguish non-moving awake time from sleep.60
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI) is the most commonly used sleep questionnaire and is considered the gold standard for measuring self-perceived sleep quality. Used in both clinical and research settings, it consists of 24 questions pertaining to the previous 30 days, five of which can be answered by a partner who shares the same room. In addition to questions about falling asleep, staying asleep, sleep duration, sleep efficiency, and sleep disturbance, there are also questions about daytime sleepiness and sleep medication use.62,63 Although the usefulness of PSQI has been validated in multiple clinical trials, it is limited by its dependence on accurate memory and should be used in conjunction with objective assessments, especially in elderly adults.64
Sleep Disorder Questionnaires
Other questionnaires are used to aid in the diagnosis and evaluation of sleep disorders, such as the Athens Insomnia Scale (AIS), Insomnia Severity Index (ISI), Mini Sleep Questionnaire (MSQ), and Epworth Sleepiness Scale (ESS).62
Sleep Diary
A sleep diary is a widely used method for subjectively describing sleep quality. Entries into a sleep diary are made in the morning immediately after waking and allow for estimates of sleep parameters such as the time between going to bed and falling asleep, time to waking after falling asleep, total sleep time, total time in bed, sleep efficiency, and overall satisfaction.62 A sleep diary may be useful in screening for sleep problems, but depends on daily compliance, memory function, and reporting ability. Notably, there is a common tendency to overestimate sleep duration and underestimate time spent awake in bed.56
4 Nutritional Sleep Hacking
Nutrients
Melatonin
Reported Dosage: 0.3–10 mg, taken about 30 minutes before bedtime
Melatonin is a hormone produced mainly by the pineal gland in the brain in response to darkness. It is found throughout the body and in nearly all body fluids.65 Although levels decline with aging, rhythmicity is generally maintained throughout life, with peak blood levels occurring around 3 AM.66 Because melatonin’s main function is regulating circadian systems, it has potential usefulness in repairing circadian disruption, such as due to shift work or travel through time zones.67,68 It has also been shown to scavenge free radicals, reduce inflammation, modulate immune function, and support mitochondrial function. Furthermore, melatonin levels are lower in those with chronic metabolic, cardiovascular, and neurologic diseases.65,69 The safety of melatonin use in healthy adults, including elderly individuals, at usual doses (generally between 0.3 mg and 10 mg nightly) has been demonstrated in multiple randomized controlled trials and meta-analyses.70 The effectiveness of melatonin supplementation for promoting sleep in healthy people has been demonstrated using doses as low as 0.1 mg and up to 6 mg. For instance, dosages of 0.3 mg were shown in studies conducted in the mid-1990s by researchers at the Massachusetts Institute of Technology to promote sleep onset without disrupting sleep architecture.71,72
A 2014 systematic review of melatonin research included 35 randomized controlled trials with a total of 2,356 subjects. Findings from a subset of 15 of the included trials that had strictly healthy participants indicated melatonin, at doses of 1–6 mg, improved sleep and reduced daytime sleepiness. Other trials in the review showed melatonin helped resolve jet lag, but evidence for its benefits in shift workers was inconclusive.73 A earlier meta-analysis of data from 17 randomized placebo-controlled trials with a total of 284 participants found melatonin supplementation improved sleep parameters, but the effects were small: in a subset of 15 trials in individuals who were either healthy or had insomnia but were otherwise healthy, the time needed to fall asleep decreased by 3.9 minutes, sleep efficiency improved by 3.1%, and total sleep time increased 13.7 minutes.74 In one randomized, placebo-controlled, crossover trial that included 24 healthy participants aged 55 years and older who had no major sleep issues, 5 mg melatonin 30 minutes before bedtime in controlled experimental conditions increased sleep efficiency, mainly by increasing stage 2 NREM sleep and slightly shortening awakenings.75
While standard melatonin supplements rapidly increase blood melatonin levels and can shorten the time needed to fall asleep, newer extended-release formulations have been found to sustain higher melatonin levels through the night in healthy individuals and hold promise for their potential to better maintain sleep through the night.76-78
Magnesium
Reported Dosage: 72–500 mg elemental magnesium daily
Magnesium is involved in regulating nerve and muscle fiber activation, modulating excitability of the nervous system, and relaxing muscle tension. Low magnesium intake is common, and intracellular magnesium levels have been shown to diminish with aging while blood levels remain stable, making it difficult to detect deficiency. Even mild magnesium deficiency can contribute to insomnia, fatigue, and cognitive and mood problems.79 In observational studies, those with the highest dietary magnesium intake reported better sleep quality, including less snoring and less daytime sleepiness. They were also less likely to report having a sleep duration of less than seven hours per night.80,81
In a randomized, controlled, crossover trial in 12 healthy elderly participants, 20 days of magnesium supplementation reduced nighttime levels of the stress hormone cortisol and increased deep sleep (stage N3). The dose was 403 mg magnesium oxide (providing 243 mg of elemental magnesium) once daily for three days, then twice daily for three days, then three times daily for 14 days.82 In a randomized controlled trial in 46 elderly subjects with insomnia, 500 mg of elemental magnesium, taken as two divided doses of magnesium oxide daily for eight weeks, increased blood melatonin levels, decreased cortisol levels, and improved self-reported total sleep time, sleep efficiency, and time to sleep onset.83 Another randomized controlled trial in 100 adults over 50 years of age with poor sleep found 320 mg magnesium (as magnesium citrate) per day for seven weeks improved sleep quality scores; however, those receiving placebo experienced a similar increase in sleep quality.84
Magnesium in the form of magnesium-L-threonate has been shown in preclinical models to increase concentrations of magnesium in the plasma and central nervous system better than other forms.85 In a randomized controlled trial, 80 people between ages 35 and 55 years with self-assessed sleep problems took 1 gram of a branded form of magnesium-L-threonate called Magtein, providing 72 mg of elemental magnesium, or a placebo daily for 21 days. Sleep and daily behaviors were measured subjectively using standardized questionnaires and objectively with an Oura Ring (a “smart” ring that tracks several biometrics and sleep metrics). Based upon the questionnaires, there was a significant improvement in the treatment group in behavior upon awakening, energy, daytime productivity, grouchiness, mood, and mental alertness compared with placebo. Objective assessments via the Oura Ring showed significant improvements in deep sleep score, REM sleep score, and light sleep time, as well as various improvements in activity scores throughout the day.86
Glycine
Reported Dosage: 3 grams taken 30–60 minutes before bedtime
Glycine is a non-essential amino acid with many functions in the body. In the nervous system, glycine acts as an inhibitory neurotransmitter that helps reduce involuntary muscle movement during sleep. It also activates receptors that lead to reduced core body temperature during sleep, and may modulate orexin neuron signaling, which could counteract wakefulness.87-89 Glycine also plays a role in regulating immune function and inflammation and is important for protein synthesis.90
In a randomized crossover trial, seven healthy men took either 3 grams glycine or placebo 30 minutes before bedtime on three consecutive nights; in a second phase of the trial, treatment assignments were reversed for another three nights. During each three-night phase, participants were required to stay up late, shortening their time in bed by 25%. Subjective daytime fatigue and sleepiness were decreased on day 1 and objective measures of alertness were improved on days 1–3 during glycine use compared with placebo, suggesting glycine may mitigate some consequences of acute sleep loss.91 Another crossover trial in 11 healthy volunteers found 3 grams of glycine within 60 minutes before bedtime on two consecutive nights improved subjective sleep quality, sleep efficiency, and daytime sleepiness; shortened objective measurements of time to fall asleep and time to enter slow-wave sleep; and improved performance on memory tests compared with placebo.92 A placebo-controlled crossover trial in 19 female subjects with self-reported sleep difficulties found 3 grams of glycine before bedtime for four days improved subjective measures of daytime fatigue, energy level, and clear-headedness.93
Ashwagandha
Reported Dosage: 120–700 mg of ashwagandha extract daily
Ashwagandha (Withania somnifera) is used in traditional Ayurvedic medicine as a remedy for insomnia, anxiety, stress, and various other ailments, as well as to build physical and mental vitality.94 A meta-analysis that pooled results from five randomized controlled trials found ashwagandha extract improved sleep, increased mental alertness, and decreased anxiety in healthy adults with and without insomnia.95 In one randomized controlled trial involving 144 healthy participants with high non-restorative sleep scores, 120 mg of a standardized extract of ashwagandha root and leaf, called Shoden, daily for six weeks improved time to sleep onset, wakefulness after sleep onset, total sleep time, and sleep efficiency as measured by actigraphy. In addition, self-reported sleep quality scores improved by 72% in those treated with ashwagandha extract, but only 29% in those given placebo.96 A randomized controlled trial that included 40 subjects with insomnia and 40 healthy subjects found eight weeks of treatment with ashwagandha improved sleep parameters more than placebo in both participant groups, although the effects were more pronounced in those with insomnia.97 In a trial in 60 college students, 350 mg of a full-spectrum ashwagandha extract twice daily for 30 days was more effective than placebo at improving self-reported sleep quality and reducing food cravings, but not for reducing self-perceived stress levels.98 Another report from the same trial indicated ashwagandha use also led to greater self-perceived well-being due to better energy levels, mental clarity, and sleep quality compared with placebo.99
Black Cumin Seed Extract
Reported Dosage: 200 mg taken 20–30 minutes before bedtime
Black cumin seed (Nigella sativa) is a culinary spice and a medicinal herb. Its oil has been shown to have anti-inflammatory, oxidative stress-reducing, and neuro-protective effects.100,101 In a randomized placebo-controlled trial that included 72 healthy subjects with self-reported non-refreshing sleep, 200 mg per day of black cumin seed oil standardized to contain 5% thymoquinone (an active compound in black cumin essential oil) for 90 days improved sleep quality and stress levels as measured by questionnaires. In addition, melatonin levels increased while cortisol (indicator of stress response activation) and orexin (neuropeptide that regulates wakefulness) levels decreased in black cumin oil-treated participants.100 An uncontrolled trial that enrolled 15 healthy participants who reported poor sleep quality evaluated the same ingredient and dosage regimen for 28 days. This study found that the black cumin preparation improved scores on scales of sleep quality, anxiety, depression, and stress, and reduced blood levels of cortisol. In addition, polysomnography performed on days one and seven of the trial showed black cumin seed oil increased total sleep time, shortened time to fall asleep, decreased wakefulness after sleep onset, and improved sleep efficiency; it also increased the proportion of slow wave (deep) and REM sleep while decreasing lighter NREM sleep stages.102
Tryptophan
Reported Dosage: 1–4.8 grams taken 20–30 minutes before bedtime
Tryptophan is an essential amino acid needed for synthesis of serotonin and melatonin.103 Interestingly, sleep deprivation has been shown to reduce synthesis of serotonin and melatonin from tryptophan, instead favoring tryptophan breakdown into compounds that may have toxic effects in the brain.104 Tryptophan and its derivative, 5-hydroxytryptophan (5-HTP), have been used to treat depression, anxiety, and sleep disorders,103,105 and higher dietary tryptophan intake was linked to lower risk of depression and increased self-reported sleep duration in an observational study with 29,687 participants.106
A crossover trial examined the effect of 1 gram of tryptophan daily for seven days compared with seven days of placebo in 98 participants with no sleep disorder diagnosis, 47 of whom had a genetic variant associated with changes in serotonin activity and increased risk of sleep impairment. Tryptophan was found to reduce wakefulness after sleep onset and increase sleep efficiency as measured with actigraphy in all participants and improve subjective sleep quality scores in those carrying the genetic variant of interest. In fact, subjective sleep quality was worse in the genetic variant group compared with the non-genetic variant group during the placebo phase, but not during the tryptophan phase.107 Another placebo-controlled crossover trial by the same research group found 3 grams of tryptophan nightly for seven nights improved sleep quality scores in 57 carriers of the genetic variant of interest and high susceptibility to stress.108
A meta-analysis of findings from four randomized controlled trials found tryptophan, at doses of 1 gram or more nightly, was particularly effective at improving indicators of sleep maintenance, such as decreasing wakefulness after sleep onset and increasing sleep efficiency.109 In a placebo-controlled trial with 28 healthy subjects reporting no or mild sleep difficulties, taking a single dose of a protein supplement with 4.8 grams of tryptophan reduced sleepiness and increased sustained alertness the next morning compared with a low-tryptophan protein supplement.110 A study in 10 healthy sleepers found a single, daytime, 2.4-gram dose of tryptophan increased subjective sleepiness and shortened the time needed to fall asleep both one and two hours later.111
Chamomile Extract
Reported Dosage: 200–400 mg twice daily
Chamomile is the common name for several daisy-like flowering plants, including German chamomile (Matricaria recutita) and Roman or English chamomile (Chamaemelum nobile), with similar medicinal properties. Chamomile extracts are widely used to support sleep, soothe tension, and relieve pain.112 A meta-analysis published in 2019 assessed findings from six randomized controlled trials and concluded that chamomile improved sleep quality in people without an insomnia diagnosis.113 A similar systematic review and meta-analysis published in 2024 examined the effects of chamomile on sleep quality across 10 clinical trials with 772 participants. The included studies used a variety of forms and dosages of chamomile preparations, including extract capsules, teas, and drops. The results showed that, in five of the studies that could be pooled and analyzed together, chamomile significantly improved PSQI scores, reflecting better overall sleep quality. However, it did not consistently improve sleep duration or efficiency. Chamomile helped with sleep onset latency in three of four studies, and reduced the number of awakenings during the night in two of three studies, though it did not affect daytime functioning. One randomized controlled trial involving 60 subjects aged 60 years and older found baseline sleep quality, based on PSQI scores, among participants was poor and improved more in those receiving 200 mg chamomile extract twice daily for 28 days than placebo.114 Another trial in 77 older individuals living in nursing homes found 400 mg chamomile twice daily for four weeks improved sleep quality scores compared with no treatment.115 In a randomized controlled trial that included 80 women who had recently given birth and were experiencing poor sleep quality, sleep quality scores improved after two weeks in women instructed to drink chamomile tea.116,117
Theanine
Reported Dosage: 50–400 mg daily OR 200 mg taken before bedtime
Theanine is an amino acid found in green tea (Camellia sinensis). Theanine is not used for protein synthesis, but has many health benefits related to its free radical-scavenging, anti-inflammatory, immune-modulating, and calming effects.118 Clinical research has indicated theanine may support healthy sleep by relieving anxiety rather than inducing drowsiness.119
In a randomized, controlled, crossover trial in 30 healthy adults with stress-related symptoms, self-reported sleep parameters including time needed to fall asleep, sleep disturbance, and sleep medication use improved after four weeks of taking 200 mg theanine nightly compared with placebo.120 In a placebo-controlled trial involving 20 university students going through a period of increased stress, 200 mg theanine twice daily for 17 days lowered salivary levels of a marker of stress; and lower levels of this stress marker were correlated with longer sleep duration.121 In a trial in nine healthy young women, 50 mg theanine reversed the negative effects of caffeine on wakefulness after sleep onset.122
Vitamin D
Reported Dosage: 25–125 mcg (1,000–5,000 IU) daily. Note: vitamin D supplementation dosage should be based on 25-hydroxyvitamin D blood levels.
Vitamin D appears to play a role in serotonin and melatonin regulation, and low vitamin D status has been linked to poor sleep in some, but not all, observational studies.123 In a study that evaluated data from a representative sample of 4,913 U.S. adults derived from the 2011–2016 National Health and Nutrition Examination Survey (NHANES) cohort, higher vitamin D concentrations were associated with a lower likelihood of sleep disorders. The researchers also used a genetic research method called Mendelian randomization (which helps study whether an outcome is caused by a certain trait) and found that vitamin D might be causally linked to sleep disorders.124 Several additional observational studies suggest a potential link between vitamin D deficiency and sleep problems.125-127 Interestingly, some evidence suggests relationships between vitamin D deficiency and higher risks of heart disease and cognitive dysfunction may be due in part to abnormal sleep patterns and poor sleep quality.128-130
A systematic review of 19 clinical trials, three of which were pooled in a meta-analysis, found vitamin D supplementation improved subjective sleep quality.131 A prospective cohort study evaluated the effects of vitamin D supplementation in 152 active-duty soldiers stationed in the U.S. Pacific Northwest. Participants with low serum vitamin D levels received either 25 mcg (1,000 IU) per day or 125 mcg (5,000 IU) per day of vitamin D3 for three months. Participants whose vitamin D levels were not low at baseline did not receive vitamin D supplements. Sleep quality was assessed with a validated patient-reported survey. Subject-reported sleep was improved in the vitamin D-treated groups after three months.132 A small, uncontrolled case series involving 28 U.S. veterans similarly concluded that increasing vitamin D status through supplementation improved subjective sleep quality compared with baseline. Participants in this study were supplemented with 30 mcg (1,200 IU) vitamin D daily if serum 25-hydroxyvitamin D was between 20 and 29 ng/mL or 1,250 mcg (50,000 IU) weekly if serum 25-hydroxyvitamin D was below 20 ng/mL.133
Saffron Extract
Reported Dosage: 14–28 mg, taken one hour before bedtime OR 7.5 mg crocetin taken after the evening meal
Saffron (Crocus sativus) is a well-known culinary herb, and a number of clinical trials have indicated saffron can improve mood and sleep.134 A randomized placebo-controlled trial in 120 subjects who described their sleep as unsatisfactory found treatment with 14 mg or 28 mg of a standardized saffron extract, taken one hour before bedtime for 28 days, improved subjective sleep quality and mood scores.135 Similarly, a trial in 63 healthy adults with self-reported sleep problems found 14 mg saffron extract twice daily for 28 days led to greater improvement in sleep quality scores than placebo.136 In a randomized controlled trial in 66 participants with mild-to-moderate sleep disorders related to anxiety, subjective measures of time needed to fall asleep, sleep duration, and sleep quality improved in those given 15.5 mg saffron extract daily for six weeks, but not in those given placebo.137 A randomized, placebo-controlled, crossover trial involving 30 subjects with mild sleep complaints found 14 days of treatment with 7.5 mg crocetin, a compound extracted from saffron, increased the intensity of sleep drive as measured with EEG; subjective measures showed crocetin also reduced feelings of sleepiness and increased feeling refreshed in the morning.138 Saffron has also been found to be beneficial for insomnia disorder.139
Probiotics
Reported Dosage: Highly variable. Since there are many probiotic strains available, it may be reasonable for most people to try a few different options with the overall goal in mind of supporting gut and overall health, as doing so may be linked to better sleep.
The gut microbiome is tightly interconnected with the nervous system. An imbalance in gut bacteria and metabolites can alter levels of neurotransmitters involved in central sleep-wake regulation, possibly contributing to sleep problems.140 Conversely, poor sleep can change the composition of the gut microbiome, which may contribute to metabolic disturbance and immune, neurologic, and hormonal dysregulation.141-143
A growing body of research indicates probiotics and related supplements can play a role in supporting healthy sleep. Many randomized placebo-controlled trials in healthy adults have shown a range of probiotic strains and dosages can improve sleep quality.144-154 Although it is challenging to synthesize the evidence due to the range of species and formulations used, a meta-analysis of data from 20 clinical trials found treatment with probiotics, killed probiotics, or cellular parts of probiotics improved subjective sleep quality in general, but did not affect objective measures of sleep. The benefits appeared to be slightly stronger in healthy individuals (rather than those with medical problems), when single organisms were used (rather than combinations), and when the treatment duration was eight weeks or longer.155 Another meta-analysis included findings from six placebo-controlled trials that used heat-killed or lyophilized (freeze-dried) Lactobacillus gasseri CP2305 alone in healthy adults with mild-to-moderate stress; the analysis found this strain of L. gasseri improved subjective sleep quality, as well as objective sleep parameters in the two trials that included EEG measurements.156
On the other hand, a meta-analysis of 18 randomized controlled trials found supplementing with probiotics and/or prebiotics (fibers that enhance growth of beneficial bacterial colonies in the gut) had no effect on sleep quality or duration.157
Hops
Reported Dosage: 400 mg of hops extract taken in the evening. Some studies evaluated non-alcoholic beer consumption as a source of hops, although the hops dosage is variable in this context.
Hops, the flower cones from the hop (Humulus lupus) plant, are used as a flavoring agent in beer and have well-known sedative effects. Extracts from hops have been shown to increase gamma aminobutyric acid (GABA) receptor activity, reducing excitability of the nervous system and supporting the onset of sleep.158,159 A randomized, placebo-controlled, double-blind, crossover study assessed the effects of a branded hops dry extract, called Melcalin Hops, on self-reported depression, anxiety, and stress levels in 36 healthy young adults with mild symptoms. Participants received two 200 mg capsules of the hops extract or placebo daily for four weeks, separated by a 2-week washout period. The study found that hops supplementation significantly reduced depression, anxiety, and stress scores compared to placebo, with no changes in cortisol levels or body composition.160 Although this study did not assess sleep outcomes, the improvements in some self-reported mood problems like stress and anxiety suggest that hops extract may provide some benefit for sleep.
In a pilot trial with 97 healthy participants, drinking non-alcoholic beer providing 35 mg of hop bitter acids nightly for three weeks resulted in improved subjective assessments of sleep quality; job performance; and mood, including anxiety, depression, fatigue, and vigor.161 In another trial, 30 healthy university students reported shorter time to sleep onset and better overall sleep quality after having a hop-containing non-alcoholic beer with dinner nightly for two weeks compared with the week before they had the beer.162 A trial in 17 healthy female nurses working rotating or night shifts found drinking 333 mL (about 12 ounces) of a hoppy non-alcoholic beer nightly for two weeks resulted in shorter time to fall asleep and better sleep quality as assessed by actigraphy.160,163
Hops are often used in conjunction with other herbs and nutrients to support healthy sleep. For example, in a placebo controlled trial in 40 subjects with poor sleep, a single dose of a combination of valerian and hops was found to improve subjective and objective measures of sleep quality, including total sleep time and time in deep sleep.164
Valerian
Reported Dosage: 200–1,215 mg of extract daily; some studies reported 600 mg of extract taken one hour before bedtime
Valerian (Valeriana officinalis) is a medicinal plant that is commonly used to promote sleep. A meta-analysis of 10 randomized controlled trials showed valerian improved sleep quality, and the effect was more consistent when the whole valerian root, rather than extract, was used.165 A study published in 2023 evaluated the effects of a standardized Valeriana officinalis extract called Sleeproot on sleep quality in individuals with mild insomnia. Over eight weeks, 80 adults were randomized to receive either the extract or a placebo. Participants randomized to valerian took 200 mg of the extract, standardized to contain 2% total valerenic acid, daily. They were instructed to take one capsule one hour before bedtime for the duration of the eight-week study with sleep improvements tracked through both a subjective questionnaire (PSQI) and objective measures (wrist actigraphy and polysomnography). Participants in the valerian group showed significant improvements in sleep latency, total sleep time, sleep efficiency, reduced anxiety, and reduced daytime sleepiness compared with placebo. By the end of the study, those in the valerian group also reported feeling more refreshed upon waking.166 Another placebo-controlled trial in 14 elderly participants with self-reported poor sleep found 405 mg valerian extract three times daily for seven days increased slow-wave sleep as assessed with polysomnography.167 Another trial in 16 insomnia patients found 600 mg valerian extract nightly increased both slow-wave and REM sleep while decreasing N1 sleep after two weeks of use.168
A clinical trial in which 128 subjects received 400 mg valerian extract, a commercial valerian product (not otherwise described), and placebo in random order and on three non-consecutive nights found the valerian extract increased subjective sleep quality and shortened the time to fall asleep. The effect was stronger in those who self-identified as poor sleepers, reported usually taking a long time to fall asleep, and those who smoked.169 Another clinical trial compared 450 mg and 900 mg valerian extract to placebo in 10 subjects who slept at home and 900 mg of valerian to placebo in eight subjects who were evaluated in a sleep lab. At home, self-reported time to fall asleep and wakefulness after sleep onset were decreased after valerian use, but sleep quality scores did not change; in the lab, valerian did not have a significant effect on sleep compared with placebo.170 In a randomized placebo-controlled trial involving 102 healthy individuals, 600 mg valerian extract an hour before bedtime did not cause morning sleepiness, poor concentration, or reduced reaction time after a single use or nightly use for two weeks, confirming the safety of valerian in healthy people.171
Cherry Products (Tart Cherry & Sweet Cherry)
Reported Dosage:
- Tart Cherry: 200–240 mL of tart cherry juice twice daily or 30 mL of tart cherry concentrate twice daily
- Sweet cherry (Jerte Valley): 200 grams of cherries twice daily or cherry powder equivalent to about 141 grams of cherries twice daily
Both sweet and tart cherries are rich in vitamin C and other free radical-scavenging compounds, and tart cherries are good sources of tryptophan, serotonin, and melatonin.172 Findings regarding the effects of tart cherry on sleep parameters have been mixed. In a randomized placebo-controlled trial in 20 healthy volunteers, tart cherry juice consumption for seven days increased melatonin levels, as well as time in bed, sleep duration, and sleep efficiency.173 A trial that included 19 healthy field hockey players whose sleep was monitored by actigraphy found 200 mL (about 7 ounces) of tart cherry juice (equivalent to about 48 tart cherries), taken five times during a 48-hour period, resulted in increased time in bed, decreased wakefulness after sleep onset, and reduced nighttime movement compared with placebo juice consumption.174 However, in a trial in which 44 healthy subjects received either 240 mL (8 ounces) of tart cherry juice, placebo juice, encapsulated tart cherry powder, or placebo capsules twice daily for 30 days, no differences in sleep parameters were found between the tart cherry and placebo groups.175 In addition, a randomized controlled trial in 50 healthy middle-aged adults found 30 mL of tart cherry juice concentrate twice daily for three months increased alertness, decreased fatigue, and improved sustained attention during a cognitive task, but did not affect sleep compared with placebo.176
Two clinical trials by one research group have investigated the effect of sweet Jerte Valley cherries on sleep. In one trial, six middle-aged and six elderly healthy volunteers added 200 grams (about 7 ounces) of cherries twice daily to their usual diet. Seven regional cherry varieties were tested for three days each. Cherry consumption increased melatonin levels as well as sleep duration and inhibited movement during sleep as measured by actigraphy.177 In the other trial, 10 young, 10 middle-aged, and 10 elderly healthy subjects consumed a cherry powder product equivalent to 141 grams of cherries or placebo twice daily for three days. Actigraphy testing showed cherry powder improved time to fall asleep, number of awakenings, sleep efficiency and duration, and nighttime movement, and the effect on sleep was stronger in older subjects.178
Bioactive Milk Peptides
Reported dosage: 150–300 mg of milk protein hydrolysate
Hydrolysis of the milk protein casein generates bioactive peptides (small amino acid chains), including some that have been studied for their effects on mood and sleep. For example, a hydrolyzed milk protein known as casein tryptic hydrolysate has been found to prolong sleep duration in mice.179 In preclinical research, alpha-casozepine, a 10-amino acid peptide derived from casein tryptic hydrolysate, has been found to sensitize GABA receptors and relieve anxiety related to stress without triggering dependence.180
A randomized, double-blind, placebo-controlled trial investigated the effects of a branded alpha-casozepine called Lactium on sleep difficulties in Japanese adults. The study involved 32 participants who received either the casein hydrolysate (150 mg daily for four weeks) or a placebo. The casein hydrolysate significantly improved subjective sleep quality.181
In another study, 43 Korean adults with mild-to-moderate sleep problems took either 300 mg of Lactium or a placebo every day for four weeks. Participants then underwent a four-week washout period and switched to the other treatment for four additional weeks. Although standard sleep quality tests did not show substantial differences between treatments, subjective sleep diaries revealed that Lactium supplementation led to greater total sleep duration, shorter time to fall asleep, and fewer wake-ups.182
In a different study, 40 adults with sleep problems took either a placebo or a combination of 300 mg Lactium and 204 mg L-theanine (an amino acid from tea with relaxing properties) daily for eight weeks. While there were no significant differences between the groups on sleep quality and insomnia scale characteristics, self-reported sleep diaries revealed that the group taking the Lactium-theanine combination slept longer, fell asleep faster, had fewer wake-ups, and went to bed earlier. The researchers also found changes in the beneficial bacteria in the gut of those who took the supplement.183 Another trial in 39 subjects with poor sleep quality scores found a branded supplement containing 150 mg of casein tryptic hydrolysate plus 50 mg theanine nightly for four weeks improved self-reported sleep duration, sleep efficiency, daytime dysfunction, and overall sleep quality scores more than placebo.184
Diet
Both the timing and composition of meals can profoundly impact the function of the internal circadian clock and regulation of sleep. Nutrients and nutrient metabolites can directly alter nervous system signaling related to sleep health. In addition, diet can trigger inflammatory processes that may lead to dysfunction in the nervous system and other body systems that may ultimately harm sleep.185,186
Chrono-Nutrition: Eating for Circadian Health
Eating has a close and circular relationship with the body’s internal circadian system. Normal circadian rhythms drive healthy appetite, digestive function, and metabolic processes during the daytime, while sleep loss can trigger abnormal appetite patterns and nutrient metabolism that, over time, can contribute to digestive and metabolic diseases.187 On the other hand, poor eating habits, digestive problems, and metabolic disorders can disrupt gut microbial balance and circadian synchrony, potentially triggering sleep disorders.186,188
Chrono-nutrition is a strategy to align eating with circadian systems in order to take advantage of optimal digestive and metabolic activity and support sleep health.186 Guidelines include186:
- Eat the majority of the day’s calories in the daytime (rather than at night). Eating most of the day’s calories at night has been associated with poor sleep quantity and quality, chronic insomnia, unhealthy eating behaviors, and metabolic health problems.187,189
- Avoid eating and drinking within two hours of bedtime. Observational studies have found eating and drinking close to bedtime was correlated with increased wakefulness and increased chance of abnormal (short or long) sleep duration.190,191
- If you need to snack at night, choose small portions of unprocessed foods. While eating close to bedtime is generally not advised, a carefully chosen bedtime snack may be helpful for avoiding nighttime hunger in some circumstances, especially in individuals prone to low blood glucose levels during the night.192 Low-calorie, nutrient-dense, simple snacks (rather than complex meals) do not appear to harm sleep parameters and may be beneficial for metabolic health in some individuals.193-196 Examples of good bedtime snacks include small portions of fruit, unsalted nuts, unsweetened yogurt, or a protein drink.197
- Stick to consistent mealtimes, ideally three times per day. Fewer meals and more frequent snacking, especially at night, has been associated with shorter sleep duration.198
Dietary Patterns
Getting too little sleep has consistently been shown to be linked to poor eating habits, including eating too many calories, too much fat, and too little fruit, as well as a shift away from three meals a day to smaller, more frequent, high-calorie snacks, especially at night.198 On the other hand, a healthy diet is essential to optimal circadian function, and nutrient imbalance may contribute to poor sleep.199-201 Dietary patterns that support cardiovascular, metabolic, and overall health, such as a Mediterranean diet and Dietary Approaches to Stop Hypertension (DASH), have also been found to be associated with high sleep quality in most observational studies.199,202-204 For example, in a study that scored adherence to a Mediterranean diet in 1,031 adults in Turkey under 65 years of age, a higher Mediterranean diet score was correlated with higher sleep quantity and quality.205
A plant-based diet is often considered to be healthful, but not all plant-based eaters consume high amounts of whole, nutrient-dense, unprocessed foods. In a study in 2,424 middle-aged and older adults in China, eating a healthy plant-based diet (eg, generally a Mediterranean-style diet rich in plant fibers, whole grains, vegetables, and minimally processed food) was associated with better sleep quality, while eating an unhealthy plant-based diet (ie, highly processed) was linked to poorer sleep quality.206,207
Diet Composition
The composition of the daily diet may affect sleep patterns. Several clinical trials have indicated high-carbohydrate diets may shorten the time needed to fall asleep and periods of wakefulness, and increased fiber in the diet may increase deep slow-wave sleep.208 One crossover trial that compared a high-protein diet to a high-carbohydrate diet in 24 healthy men found the high-carbohydrate diet led to a small increase in melatonin production, less time in light (N1) sleep, less time needed to fall asleep, and better sleep efficiency compared with the high-protein diet.209 On the other hand, meta-analyses of clinical trials have found a low-carbohydrate diet increased the length and proportion of slow-wave sleep, decreased REM sleep, reduced time to sleep onset, and increased sleep efficiency.210,211 The quality of carbohydrates in the diet are also important to consider, since a diet rich in fiber-dense carbohydrates may promote optimal sleep through a range of mechanisms.212
Ketogenic diets are very low in carbohydrate, high in fat, and adequate in protein, and are used to treat epilepsy and obesity. People following this diet generate large amounts of ketone bodies, byproducts of fat metabolism made in excess when glucose levels are very low. Ketogenic diets have been found to reduce appetite and food intake and may improve sleep quality, although the data on sleep is inconclusive.213 A clinical trial in 324 women with overweight and obesity found adhering to a very low-calorie ketogenic diet for 31 days led to improved subjective sleep quality, and sleep improvement was associated with the degree of body fat loss.214 Emerging evidence suggests ketone bodies may alter circadian signals affecting appetite and the sleep-wake cycle.213,215
One study examined the diets of 15,991 Americans and scored them based on the balance of pro-oxidants (foods high in iron, omega-6 fatty acids, and saturated fat) and antioxidants (foods high in carotenes and carotenoids, selenium, vitamins C and E, and omega-3 fatty acids). After following the participants for a median of 7.4 years, those with short sleep duration and a balance favoring dietary antioxidants were found to have a lower mortality rate than short sleepers with a pro-oxidant-favoring diet.207 Another study that used data from 6,300 participants in the NHANES found a higher antioxidant to pro-oxidant balance was correlated with longer sleep duration and lower risk of sleep disorders.216 These findings suggest eating an antioxidant-rich diet may not only increase sleep duration but may also protect against some of the negative health effects of short sleep.
Specific Foods
Certain specific foods have been linked to better sleep. For example, studies have shown milk, tart cherries, kiwis, and fatty fish are foods that can promote sleep.186,217 This may be partly due to their natural melatonin content. Other food sources of melatonin include eggs, wheat, oats, grapes, strawberries, peppers, tomatoes, and mushrooms.217
Other foods and beverages can worsen sleep.186 For example, alcohol is a nervous system depressant and can shorten the time needed to fall asleep. Although many individuals use alcohol to help them fall asleep, it can also alter sleep architecture and interfere with circadian rhythms, increasing the risk of sleep problems.218 Furthermore, in animal research, intermediate and heavy alcohol intakes were found to temporarily but dramatically suppress glymphatic function, potentially leading to brain cell damage, whereas light alcohol intake was shown to increase glymphatic clearance.219
Nicotine is another important consideration: though not found in significant amounts in food, nicotine has complex effects on neurotransmitter activity and negatively impacts sleep. Nicotine in tobacco products can lengthen the time needed to fall asleep, decrease sleep efficiency, increase sleep fragmentation, and reduce sleep quality.186 Limiting or avoiding alcohol and nicotine, especially in the four hours prior to bedtime, may help optimize sleep.218,220
5 Hack Your Habits & Lifestyle for Better Sleep
A growing body of research shows several key lifestyle factors are associated with better sleep quantity and quality. Adopting these sleep-promoting habits may help individuals live healthier and more vibrant lives. It is also important to identify and treat or modify any obstacles to healthy sleep that may be present, such as an undiagnosed sleep disorder, a mental health disorder, or use of a medication that can harm sleep.
Check for Undiagnosed Sleep Disorders
Many common sleep disorders go unrecognized, undiagnosed, and untreated.226 Common sleep disorders, which frequently co-occur, include:
- Chronic insomnia (lasting three months or longer) is estimated to affect about 10% of the population.227,228
- Obstructive sleep apnea (frequent bouts of airway narrowing or collapse, breathing interruption [apnea], and waking during sleep) affects an estimated 10% of the population.227,229
- Sleep bruxism (jaw clenching and teeth grinding during sleep) affects up to 15% of adults and as many as 49% of children.230
- Restless legs syndrome (muscle restlessness with a desire to move the limbs, especially at night) is estimated to affect 3% of the general population, with higher prevalence in women and older individuals.231
Nocturia (waking at night to urinate) can contribute to poor sleep quality and often coexists with chronic insomnia disorder, especially in older individuals.232,233 Nocturia is the most common cause of sleep interruption in elderly adults, and may be attributable to changes in hormone balance, bladder capacity, and circadian function.234-236 Waking to urinate two or more times per night has been associated with lower subjective sense of well-being, lower workplace performance, and poorer general health status.237-239
Sleep disorders occur more frequently in individuals with neurological, psychiatric, and other health problems; in turn, chronic sleep disturbance is correlated with increased risks of a range of health problems, including cardiovascular, metabolic, neurologic, and psychiatric conditions, as well as frailty and mortality.2,240,241 If you suffer from frequent poor sleep, it is important to consult a health care provider to investigate the possibility of a sleep disorder and initiate treatment if appropriate.
More information about sleep disorders can be found in Life Extension’s Insomnia, Sleep Apnea, and Restless Legs Syndrome protocols.
Check for Depression, Anxiety, & Stress
Sleep has a bi-directional relationship with mental health, such that chronic sleep disorders increase the risks of depression, anxiety, and related disorders, while in turn mental health disorders increase the risk of sleep disorders.242-244 Even occasional bouts of poor sleep have a negative impact on mood and may increase the risk of developing anxiety disorder, depression, and exhaustion syndrome.242 Interestingly, in one study that included 115 participants with insomnia, lower scores on subjective assessments of sleep quality and “morningness” (seeing oneself as a “morning person”) were more closely associated with depressive symptoms than objective sleep studies (polysomnography) or measures of circadian clock type.245
Sleep loss is known to activate the body’s stress signaling network, which can further aggravate sleep disruption.246 Prolonged stress and burnout have been shown to impair sleep quality, and those affected by short-term and long-term sleep disturbances have reported higher levels of stress and burnout.242,243 For example, one study that followed 59 medical students for 90 days found subjective measures of work-related stress were higher on workdays following nights with low sleep duration.247 The relationship between poor sleep and a dysregulated stress response has been proposed as an underlying mechanism by which sleep loss contributes to physical and mental health problems.16 Chronic stress signaling even appears to inhibit glymphatic function, leading to a buildup of neurotoxins that may contribute to neurologic disorders.30 On the other hand, restoring sleep health is an important part of treatment for mental health disorders through its ability to regulate stress signaling, reduce brain inflammation, and improve neuroplasticity.16,244
Treating underlying depressive and anxiety disorders and managing stress effectively can be helpful for improving sleep. More information about these conditions can be found in Life Extension’s Depression and Depressive Disorders, Anxiety and Anxiety Disorders, and Stress Management protocols.
Are Medications Disrupting Your Sleep?
Drug prescriptions and the regular use of multiple medications at the same time have increased substantially over the past two decades. As of 2016, approximately 17% of Americans were using at least one medication with insomnia as a potential side effect, and about 7% were using two or more such drugs.248
A wide range of drugs may interfere with sleep in susceptible individuals. Some commonly prescribed examples include:
- Thyroid medications, such as levothyroxine (Synthroid)248
- Antidepressants and anti-anxiety drugs, such selective serotonin reuptake inhibitors (SSRIs) like fluoxetine (Prozac), citalopram (Celexa), and escitalopram (Lexapro); and serotonin norepinephrine reuptake inhibitors (SNRIs) like venlafaxine (Effexor), duloxetine (Cymbalta), and desvenlafaxine (Pristiq)248,249
- Stimulants (ie, a class of drugs usually used to treat attention deficit disorder), such as methylphenidate (Ritalin) and amphetamine-dextroamphetamine (Adderall)248
- Sedatives, such as diazepam (Valium) and triazolam (Halcion)250
- Drugs used to treat cognitive disorders, such as donepezil (Aricept), rivastigmine (Exelon), and galantamine (Razadyne)251-253
- Cold medications, particularly pseudoephedrine (Sudafed) and combination products with pseudoephedrine248
- Glucocorticoids, such as prednisone (Deltasone), dexamethasone (Decadron), and methylprednisolone (Medrol)254,255
- Smoking cessation therapies, such as varenicline (Champix), bupropion (Zyban), and nicotine replacement patches (Nicoderm), lozenges (Nicorette), and gum (Nicorette)248
- Opioid pain relievers, such as morphine (MS-Contin and others), tramadol (Ultram), oxycodone (Oxycontin), hydrocodone/acetaminophen (Vicodin), oxymorphone (Opana), and fentanyl (Duragesic)248,256
- Some asthma medications, eg, theophylline (Elixophyllin and others) and albuterol (Ventolin and others)257
- Some blood pressure-lowering drugs, eg, beta-blockers like atenolol (Tenormin) and metoprolol (Lopressor)258,259
Although sedatives in the drug class called benzodiazepines, including diazepam (Valium), alprazolam (Xanax), lorazepam (Ativan), and clonazepam (Klonopin), are frequently used to treat insomnia and anxiety, their use can disrupt normal sleep architecture by increasing time in N2 sleep and reducing restorative N3 slow-wave sleep and REM sleep.260 A study in two healthy subjects showed their use can suppress melatonin production.261 Benzodiazepines are also well known to cause tolerance (the need for increasing doses to experience the same effect) and addiction with potentially life-threatening consequences. Because of these problems, benzodiazepines are only indicated for short-term use, although many people remain on them for years or even decades.262
If you are experiencing difficulty sleeping and are using one or more of the drugs listed above, speak with your health care provider before making any changes in your medication regimen.
Optimize Sleep Hygiene
Sleep hygiene is a general term for bedtime habits that enhance sleep. The components of sleep hygiene recommendations vary, but there are some consistent themes273,274:
Avoid arousing and emotionally charged activities before bedtime. An anxious state of mind, or hyperarousal, is considered a key factor in insomnia.275 In addition to setting aside emotional topics in the evening, creating a to-do list for the next day before going to sleep may be a useful strategy for letting go of worry and getting good sleep.276
Have consistent routines around bedtime, including timing and rituals. Adhering to a structured sleep schedule with set sleep and wake times has been found to improve circadian alignment in healthy young adults, which may help optimize sleep.277 Social jetlag, a term that refers to the difference between sleep timing that is adjusted for socially necessary schedules (eg, during the work or school week) and natural sleep timing (eg, on the weekend when there are no social pressures), can be a cause of sleep loss and has been linked to negative health outcomes.278-280 Although consistent earlier and less variable bedtimes have been associated with better health, it may be possible to partially mitigate the negative effects of sleep time variability and social jetlag through “catch-up” sleep, such as sleeping longer on the weekends.280,281
Avoid smoking or drinking alcohol before bed; keep nighttime snacks early, small, and simple; and hydrate with water early in the night. Nighttime nicotine and alcohol use can diminish sleep quality.186 In addition, eating or drinking close to bedtime has been correlated with increased wakefulness and higher likelihood of short or long sleep duration.191 However, it may sometimes be appropriate or even beneficial to eat a light simple snack before bedtime.193,282 Good choices include foods and drinks shown to improve sleep like tart cherry juice, kiwi fruit, or a small glass of milk.283
Create a bedroom environment that supports sleep, with attention to factors such as comfortable bed and bedding, as well as ambient temperature, air quality, noise level, and light. Higher ambient temperature and increased levels of noise, carbon dioxide, particulate pollution, and light pollution have all been associated with worse sleep quality in healthy adults.284,285
- Comfortable bed. While bed preferences vary between individuals, a medium-firm mattress has generally been found to provide the most comfort, reduce the risk of back pain, and support optimal sleep quality.286 Weighted blankets are sometimes promoted for their calming effect, and clinical evidence indicates they may be especially helpful in adults and children with attention deficit hyperactivity disorder (ADHD) and/or autism spectrum disorder.287-289 An uncontrolled clinical trial in 68 elderly nursing home residents found the use of a weighted blanket improved sleep, cognitive function, and overall health and quality of life.290 Other research suggests their use may increase melatonin production.291
- Temperature. An overly warm air temperature, especially combined with humidity, may interfere with natural nighttime body cooling, disrupt normal sleep architecture, and reduce sleep quality.284,292 Some recommendations suggest an ideal sleep temperature range of 60–68ºF.293,294 On the other hand, warming the feet by using a warm foot bath before bed or socks in bed has been shown to further improve sleep health.295
- Air quality. Using a bedroom air purifier and opening a bedroom window or door are strategies that have been found to reduce carbon dioxide and particulate levels and improve objective and subjective sleep measurements.296,297
- Noise. Noisy neighborhoods and traffic noise have been linked to poor sleep and negative health outcomes, with shorter sleep duration, increased sleep fragmentation, lower sleep efficiency, and greater daytime sleepiness.285,298 Earplugs and white (background) noise generators may help reduce the effects of noise on sleep, but findings from clinical trials are inconclusive.299,300
- Light. Exposure to artificial light at night can suppress melatonin release, disrupting circadian processes and making it harder to fall asleep.285 Moreover, exposure to light at night has been shown to be associated with a host of health problems beyond just sleep issues.301,302 Eye masks are a simple strategy for reducing nighttime light exposure and have been shown to lengthen slow-wave deep sleep and improve alertness and cognitive function the next day in healthy young adults.303 Anecdotally, “blackout” or light-blocking curtains may be helpful.
Get plenty of exercise during the day. Regular daytime exercise has consistently been shown to improve subjective sleep quality and reduce health risks associated with poor sleep.304-306 Animal research also suggests exercise may protect against neural injury that could contribute to poor sleep by strengthening glymphatic activity.307,308 Because of its powerful effects, regular exercise is an important component of sleep hygiene programs; however, avoiding strenuous physical activity close to bedtime is frequently advised. Meta-analyses of clinical trials have shown high-intensity exercise in the hour before bedtime reduced REM sleep, increased the time needed to fall asleep, and reduced sleep duration and sleep efficiency in healthy young and middle-aged adults; but these negative effects were not seen with light- and moderate-intensity exercise or when exercise occurred two to four hours before bedtime.309-311
Spend time in sunlight. Time in the sun is important for maintaining healthy circadian function and has been found to be associated with better sleep.312 A growing body of evidence suggests getting adequate sunlight, whether outdoors or through windows, during the day may be more important than artificial light exposure at night for circadian and sleep health.312,313 Of course, skin protection or sunscreen should be used during extended exposure to direct outdoor sunlight.
Avoid screen-time in bed or around bedtime. The use of light-emitting devices such as televisions, computers, and smartphones near bedtime has been linked to difficulty falling asleep, staying asleep, and worse sleep quality. One reason may be the light-emitting diodes (LEDs) in these devices, which generate light that is enriched in blue light. Light receptors in the circadian system are especially sensitive to blue light, which suppresses melatonin secretion and increases alertness.314 Despite the popularity of blue light-blocking filters and glasses, there is limited evidence for their ability to improve sleep in nighttime users of digital devices.314-316 Another factor may be social media engagement through screen time (social media may also fall under the “arousing and emotionally charged activities” category). Excessive use of social media has complex effects on the nervous system that lead to sleep loss and can trigger digital addiction in both adolescents and adults.317-319
Engage in relaxing activities before bed. Findings from multiple studies indicate relaxing activities like mindfulness and other forms of meditation, breathing exercises, and progressive muscle relaxation may lead to better sleep quality.320,321 Specialized apps that guide the user in mindfulness meditation and deep breathing, such as Headspace and Calm, are widely used to reduce stress and enhance sleep, and preliminary findings from clinical trials suggest they may be effective.322,323 Music has been used for centuries as a method of enhancing relaxation and treating sleep problems, and modern clinical trials have found music-assisted relaxation can improve subjective measures of sleep quality.324,325 Mind-body exercise like yoga, tai chi, and qigong may also support healthy sleep. One meta-analysis found mind-body exercise at least three times per week increased subjective sleep quality in older adults with sleep difficulties.326 A warm (not hot) shower or bath may also be conducive to sound sleep. One meta-analysis of 13 clinical trials found a warm shower or bath one to two hours before bedtime for as little as 10 minutes significantly shortened the time needed to fall asleep and improved self-reported sleep quality and sleep efficiency.327
Remove the bedroom clock. “Clock-watching” is a common practice during periods of wakefulness in the night. Although monitoring awake time may be perceived as a way to control sleep duration, in actuality, clock-watching has been shown to heighten frustration and exacerbate insomnia.328,329 Removing clocks and other timekeeping devices from the bedroom and developing skills for dealing with awake time in the night are key to managing short- and long-term sleep difficulties.328
What are the Most Important Recommendations?
Sleep hygiene interventions have been shown to improve sleep in young adults,330,331 older individuals,332,333 and athletes334-336 with sleep difficulties. An observational study involving 300 participants without sleep disorder diagnoses evaluated the relationships between sleep hygiene practices and subjective sleep quality using the PSQI. Of 35 sleep hygiene habits studied, 18 were independently associated with worse sleep quality273:
- Worrying about falling asleep while in bed
- Inconsistent total sleep times
- Using sleep medications
- Worrying about sleep during the day
- Going to bed feeling stressed or other negative emotions
- Checking the time during the night
- Going to bed hungry
- Having no sunlight exposure or time outside during the day
- Going to bed thirsty
- Inconsistent bedtimes
- Engaging in activities other than sleep in bed
- Inconsistent wake times
- Sleeping with uncomfortable bed or pillows
- Not taking time to relax before bedtime
- Napping during the day
- Having an unpleasant conversation near bedtime
- Sleeping in a poorly ventilated bedroom
- Pondering unresolved matters before bed
Sleep hygiene for shift-workers may include slightly different recommendations. A panel of experts recently compiled a list of recommendations and considerations specifically for shift workers to optimize the quality of their sleep337:
- Prioritize sleep (consider rescheduling non-essential tasks to not cut into sleep time)
- Aim for seven to nine hours of sleep per 24 hours
- Develop a sleep schedule
- Develop a bedtime routine
- Plan your transition to days off
- Use napping, in 15- to 20-minute bouts, as a helpful tool
- When planning sleep time, remember that sleep inertia (the groggy time between ending sleep and being fully awake) impairs performance and can raise the risk of accidents
- Create a comfortable sleep environment
- Use your bed only for sleep and intimacy
- Consider whether the amount of light in the sleep environment is affecting sleep
- Consider whether caffeine intake is affecting sleep
- Consider whether nicotine consumption is affecting sleep
- Consider whether alcohol intake is affecting sleep
- Be mindful of medications that may interfere with sleep
- Consider whether nighttime hunger or fullness is affecting sleep
- Consider whether the timing of fluid intake is affecting sleep
- Engage in regular exercise
- Develop strategies for sleep problems
Breathe Well During Sleep
Breathing through the nose is important for warming, humidifying, and filtering inspired air, and the proportion of breathing that occurs through the nose (as opposed to the mouth) normally increases during sleep.338 Too much open-mouth breathing during sleep can lead to drying of mouth and throat, periodontal disease and cavities, snoring, poor sleep, and onset and worsening of sleep apnea.339-342
Mouth taping may be an effective solution for mouth-breathers: in a clinical trial involving 20 subjects with mild sleep apnea and open-mouth breathing, taping the mouth closed at night resulted in reduced snoring and sleep apnea, with greater benefits seen in those with worse baseline symptoms.338 A single strip of medical silicone tape, placed vertically under the nose and across both lips, was used to seal the mouth closed in the study. Nasal dilation is another method of encouraging nose breathing. Nasal dilators worn in the nostrils may be more effective at reducing snoring and sleep apnea and improving subjective sleep quality than externally worn nasal strips.343,344
Nasal congestion, whether caused by allergic or non-allergic inflammation of the nasal passages or sinuses, reduces nose breathing and can disrupt normal sleep cycle architecture and degrade sleep quality.339,340 Furthermore, nasal congestion is a common contributor to obstructive sleep apnea and can interfere with its treatment.339,342 If you suspect airflow through your nose and sinuses may be suboptimal, consultation with an otolaryngologist (ie, ear, nose, and throat [ENT] doctor) may be worthwhile.
Consider Lavender Aromatherapy
Lavender (Lavandula angustifolia) is an aromatic plant that has demonstrated neuroprotective effects in preclinical studies.345 It is usually used in aromatherapy, or inhalation therapy, and is one of the most widely used plants for treating sleep problems.346 Aromatherapy using lavender has been shown to be beneficial in subjects with primary sleep disorders as well as those with other conditions that can be complicated by insomnia, such as neurological, psychiatric, heart, kidney, respiratory, and metabolic diseases, as well as cancer.346,347
Multiple randomized controlled trials have shown lavender essential oil can improve objective and subjective measures of sleep quality in people without frank sleep disorders.348 In a randomized controlled trial in 24 healthy Japanese women with an average age of 20 years, those who received lavender aromatherapy via skin patches worn nightly for seven nights had greater reductions in fatigue and anxiety scores and improvement in mood, but not sleep quality, compared with those given skin patches with no aroma. Interestingly, questionnaires showed 50% of the participants had previously undiagnosed sleep disorders when they enrolled in the trial.349 In a controlled trial in 79 college students with self-reported sleep issues, wearing a lavender-infused aromatherapy skin patch nightly for five nights enhanced the positive effects of a sleep hygiene program on sleep quality compared with a placebo skin patch, and the effect was still significant two weeks after the end of the intervention.350 A controlled trial in 15 students found lavender aromatherapy for five nights reduced morning sleepiness scores.351 Another study that enrolled 80 university students found lavender oil aromatherapy for one week improved subjective measures of sleep quality and fatigue. In this study, subjects in the intervention group placed lavender-scented stones near their beds at night.352 Polysomnographic testing showed exposure to lavender aroma during sleep on one night increased the amount of slow-wave deep sleep in healthy young subjects without sleep problems.353,354 In one trial, the increase in slow-wave sleep was correlated with increased subjective next-morning vigor.354
Lavender aromatherapy has been found to increase blood melatonin levels in older adults.355 In an uncontrolled trial in 39 older subjects living in a nursing home, lavender aromatherapy for one week reduced daytime sleepiness scores.356 In postmenopausal women, both oral lavender and lavender aromatherapy have been found to improve sleep and relieve other menopausal symptoms.357,358
Adopt a Healthy Sleep Posture
There does not appear to be a strong consensus on which sleep position is best for sleep quality and overall health; choosing a sleep position often comes down to what is most comfortable for the individual. There is, however, some evidence that side-sleeping may be more beneficial than other positions. A study in 13 healthy sleepers found those who showed a preference for right side-sleeping had better sleep quality, as measured by actigraphy and questionnaire, than those who showed a preference for supine (on the back) sleeping.359 Side-sleeping appears to promote better cleansing of brain tissue through increased glymphatic drainage.33 Interestingly, a preliminary observational study found 45 subjects with neurodegenerative diseases (Alzheimer disease, Parkinson disease, Lewy body dementia, and other dementias) spent more time sleeping on their backs and less time on their sides when compared with 120 healthy age-matched subjects.360 Other research in Parkinson disease patients has indicated greater sleep time in the supine position is associated with this condition and increases with disease duration and severity.361-363 Conversely, a supine sleep position is frequently associated with snoring and is a contributing factor in the majority of cases of sleep apnea, both of which substantially diminish sleep quality.364,365 Many devices have been developed to discourage supine sleeping and maintain side-sleeping—from specialized pillows to objects worn on the back and devices that vibrate gently when activated.366 Clinical trials in sleep apnea patients suggest positional therapy using such devices can be helpful.364,366,367 In addition, those who cannot side-sleep may benefit from simply rotating the head to a side, possibly with the help of a specialized pillow, while sleeping in a supine position.368,369
Synchronize Your Circadian Clock
The human body’s circadian network, which consists of a central circadian “clock” in the brain and peripheral circadian regulating cells in other tissues, synchronizes biologic processes throughout the body and shapes our behaviors within the external 24-hour cycle of light and dark.370,371
Alignment between the circadian clock and environmental and physiologic cycles—or circadian synchrony—can be disturbed by a range of common behaviors and conditions, including shiftwork, late-night social or other activities, and travel through time zones. Light and noise exposure, nighttime eating and drinking, and temperature changes during the night can also interrupt circadian synchrony.372 In addition, neurologic and psychiatric disorders can cause circadian network dysfunction and sleep-wake cycle disturbance.240 Chronic circadian rhythm disruption has been linked to increased risks of neurologic, psychiatric, cardiovascular, metabolic, digestive, and infectious diseases, as well as some cancers and mortality.373-376
Circadian rhythms are expressed differently between individuals, resulting in a range of chronotypes—inherent tendencies for timing of activities and sleep. A morning chronotype has a natural inclination for morning activity, an early bedtime, and rising early, while an evening chronotype performs better later in the day and prefers a later bedtime and awakening time. About 40% of adults have a chronotype that falls somewhere on the spectrum from morning to evening, but most people have a “neither” chronotype, exhibiting no circadian preferences. Observational research shows morning chronotypes are more likely to sleep well and enjoy better mental and physical health compared with evening chronotypes.377
Chronotype appears to have genetic and epigenetic underpinnings and varies with age and between genders.377,378 A test called dim light melatonin onset assesses the circadian timing of melatonin release and may be used as an objective indicator of chronotype and circadian alignment, but its role in diagnosing and monitoring sleep problems is still not well understood.379 Adapting lifestyle habits, social activities, and work commitments to more closely match chronotype is sometimes recommended as a strategy for avoiding circadian desynchronization.377 On the other hand, circadian rhythms can, to some degree, be adjusted and strengthened by establishing and adhering to a regular schedule of sleep, activity, and eating.380
Circadian rhythm disturbances may be treatable through chronotherapy, a technique that seeks to manipulate circadian rhythms, often using morning bright light exposure to establish a healthy sleep-wake cycle and improve circadian alignment between the body’s central clock and peripheral circadian networks throughout the body.381 Bright light therapy is sometimes combined with one day of sleep deprivation followed by several days of structured early bedtimes and waketimes. This is called triple chronotherapy and has been shown to improve sleep parameters in people with circadian rhythm disorders and those with depression and bipolar disorder.382,383 Daytime blue light therapy is sometimes added to chronotherapy to support daytime alertness and enhance melatonin function in the evening, and may improve measures of daytime functioning and sleep quality.381,384
Napping & Sleep Inertia
Napping is sometimes used as a way to catch up on lost sleep, yet poor sleepers are frequently warned against daytime naps based on the belief that a nap can disrupt the normal sleep-wake cycle. Although habitual napping has been correlated with negative cognitive and physical health outcomes, especially in older individuals, occasional short naps in the early afternoon may improve mental and emotional function without disrupting the sleep-wake cycle.385
Clinical evidence shows a nap can be safe and restorative if it is timed correctly and is not too long. An afternoon nap, especially in the context of a sleep deficit, can effectively relieve fatigue, suppress the sleep drive, and improve cognitive function for hours; however, timed too late in the afternoon, a nap could interfere with falling asleep at bedtime.385 A short 10- to 20-minute nap has been shown to result in an immediate increase in alertness and mental function, possibly due to the inclusion of only lighter stages of sleep386,387; on the other hand, a two-hour nap, which is likely to include deep slow-wave sleep, is typically followed by a period of grogginess known as sleep inertia.385,387 Sleep inertia describes the time immediately following sleep, when one is no longer asleep but is not yet fully awake. It is a state marked by sleepiness, disorientation, and decreased cognitive performance and is aggravated by sleep loss, which causes more severe and prolonged sleep inertia.387
6 Sleep Tech
Interest in at-home sleep-tracking devices has grown tremendously over the past decade. An ever-growing number and diversity of devices are currently available offering various combinations of sleep-hacking technologies.
Wearables
Wearable devices that use actigraphy to assess sleep-wake dynamics have increased in popularity and availability over the past decade. Typically worn on the wrist (like a watch) or finger (like a ring), such devices sometimes supplement information about movement with other readings such as heart rate, skin temperature, blood oxygen levels, and skin conductivity. Many devices use algorithms to synthesize collected data and provide easy-to-understand information about sleep patterns. They may also be paired with a user interface, such as on a smart phone, to administer questionnaires that add context and may increase accuracy.58
Data from commercial wearable sleep trackers (eg, Fitbit, Apple Watch, Garmin, Whoop, Jawbone, and Polar wrist devices; Somfit forehead patch and Dreem headband; and Oura Ring) has been shown to be consistent with clinical actigraphy measurements, but also overestimates sleep and underestimates wakefulness in bed compared with polysomnography.56,58,392 Although some products, particularly head-worn devices, claim to be able to measure sleep architecture, they have not yet been shown to accurately discern sleep stages.56,392 The newest type of wearable sleep-tracking device is clothing, specifically pajamas, made from fabric with an embedded network of sensors. So-called “smart” pajamas can detect body position, movement, breathing rate, and heart rate. More research is needed to validate the usefulness of sleep-tracking pajamas.56
The Oura Ring recently became eligible for coverage with pre-tax funds in health savings accounts (HSAs) and flexible spending accounts (FSAs) in the United States.393 To access HSA and FSA funds for purchasing other wearable sleep and fitness tracking devices, a letter of medical necessity from a qualified health care provider is still required as of October 2023.394
Nearables
Nearables are contactless devices that are placed near the user during sleep, such as on a bedside table or the mattress. Sensors placed on or under mattresses can detect motion, respiration, and pulse, while bedside devices use light and sound sensors to measure sleep parameters.56,395 A meta-analysis included findings from 22 clinical trials attempting to validate nearable products against polysomnography. There was a high degree of variability in performance between brands, but the contactless devices, in general, were found to overestimate sleep and underestimate wakefulness, and were relatively inaccurate at identifying sleep stages. Nevertheless, the contactless devices studied, especially those using mattress-based pressure sensors, were more accurate than actigraphy for measuring time to sleep onset, wakefulness after sleep onset, total sleep time, and sleep efficiency, and performed relatively well at sleep-tracking in healthy people.395
Sleep-Enhancing Technology
Many sleep-tracking devices use the data they collect to develop personalized programs for sleep enhancement. For example, a smart phone app that determines an individual’s circadian rhythm won the National Sleep Foundation 2022 SleepTech Award for Sleep Health and Wellness.396 The app uses circadian rhythm data to determine chronotype and develop personalized recommendations regarding timing of light exposure, food, coffee, mental activity, physical activity, and sleep to improve circadian synchrony. The app is also paired with a wearable device that uses blue light therapy intended to reset the circadian rhythm.397 The 2021 SleepTech Award was given to a product with sleep-monitoring earbuds that measure sleep parameters.396 The earbuds can also deliver personalized audio that fades as the wearer falls asleep and optional white noise during sleep.398
7 Frequently Asked Questions
How much sleep do you need by age?
Recommended sleep durations are as follows41:
-
Adults
- 7–9 hours for adults
- 7–8 hours for older adults
-
Children
- 14–17 hours for newborns
- 12–15 hours for infants
- 11–14 hours for toddlers
- 10–13 hours for preschoolers
- 9–11 hours for school-aged children
- 8–10 hours for teenagers
Is it better to sleep at night or in the day?
Sleeping at night is preferred over sleeping in the daytime because it synchronizes internal circadian systems with evolutionary external cues. Circadian synchrony is necessary for healthy function of all the body’s systems.44,370
How to improve REM sleep?
Healthy sleep depends on good sleep architecture, with adequate amounts of both REM and non-REM sleep. Avoiding heavy alcohol use and taking targeted supplements such as black cumin seed oil can help increase REM sleep.102,218
How to sleep better away from home?
Maintaining your usual sleep-wake routine and timing can help reduce the chance of disrupting healthy sleep patterns while away from home.280
Why it is better to sleep in the cold
The body’s temperature naturally decreases during the night, and a sleep environment that keeps the body too warm has been shown to reduce sleep quality.284,292
Do you fall asleep faster sleeping with someone?
Compared to people who sleep alone, those who share their bed with a partner reported falling asleep more easily, being less wakeful, getting more sleep, and feeling less daytime fatigue. They also reported lower risk of sleep apnea and reduced insomnia severity.399 What’s more, co-sleeping has been shown to increase continuous REM sleep and synchronization of sleep architecture between sleep partners.400 However, if your partner has sleep apnea and/or snores, moves a lot during sleep, has to urinate frequently in the night, or interrupts your sleep for other reasons, your sleep quantity and quality may be compromised.401
Does your body get used to a lack of sleep?
Chronic sleep loss takes a toll on all body systems, even if you get used to feeling tired all the time.1
Can you make up for a lack of sleep?
Catching up on sleep, such as by sleeping late on weekends, appears to mitigate, though may not completely reverse, some of the negative health effects of sleep loss.280,281
Is how long you sleep all that matters?
Getting enough sleep is a critical part of sleep health, but the quality and timing of your sleep are equally important.36
Are naps a substitute for lack of sleep?
Naps can help you recover from short-term sleep loss, but chronic sleep loss disrupts the body’s internal circadian system, which cannot be resolved with daytime napping.44,370
Does alcohol before bed improve sleep?
Alcohol before bed may make you sleepy and help you fall asleep faster, but it can also cause abnormal sleep architecture and disrupt circadian rhythms.218
Should you stay in bed if you cannot fall asleep?
It depends. Many sleep hygiene recommendations include using the bed only for sleep and intimacy. What’s more, evidence suggests worrying about not falling asleep can actually make sleep worse.273 So, if your time awake in bed is fraught with worry, getting up for a while to do something relaxing is probably a good idea; but if you can use the time in bed for meditation or relaxation, that may be the better choice.
Disclaimer and Safety Information
This information (and any accompanying material) is not intended to replace the attention or advice of a physician or other qualified health care professional. Anyone who wishes to embark on any dietary, drug, exercise, or other lifestyle change intended to prevent or treat a specific disease or condition should first consult with and seek clearance from a physician or other qualified health care professional. Pregnant women in particular should seek the advice of a physician before using any protocol listed on this website. The protocols described on this website are for adults only, unless otherwise specified. Product labels may contain important safety information and the most recent product information provided by the product manufacturers should be carefully reviewed prior to use to verify the dose, administration, and contraindications. National, state, and local laws may vary regarding the use and application of many of the therapies discussed. The reader assumes the risk of any injuries. The authors and publishers, their affiliates and assigns are not liable for any injury and/or damage to persons arising from this protocol and expressly disclaim responsibility for any adverse effects resulting from the use of the information contained herein.
The protocols raise many issues that are subject to change as new data emerge. None of our suggested protocol regimens can guarantee health benefits. Life Extension has not performed independent verification of the data contained in the referenced materials, and expressly disclaims responsibility for any error in the literature.
- Ramar K, Malhotra RK, Carden KA, et al. Sleep is essential to health: an American Academy of Sleep Medicine position statement. J Clin Sleep Med . Oct 1 2021;17(10):2115-2119. doi:10.5664/jcsm.9476. https://www.ncbi.nlm.nih.gov/pubmed/34170250
- Kumar M, Orkaby A, Tighe C, et al. Life's Essential 8: Optimizing Health in Older Adults. JACC Adv. Sep 2023;2(7)doi:10.1016/j.jacadv.2023.100560. https://www.ncbi.nlm.nih.gov/pubmed/37664644
- Gao X, Huang N, Guo X, Huang T. Role of sleep quality in the acceleration of biological aging and its potential for preventive interaction on air pollution insults: Findings from the UK Biobank cohort. Aging Cell. May 2022;21(5):e13610. doi:10.1111/acel.13610. https://www.ncbi.nlm.nih.gov/pubmed/35421261
- Carroll JE, Prather AA. Sleep and Biological Aging: A Short Review. Curr Opin Endocr Metab Res. Jun 2021;18:159-164. doi:10.1016/j.coemr.2021.03.021. https://www.ncbi.nlm.nih.gov/pubmed/34901521
- Siegel JM. Sleep function: an evolutionary perspective. Lancet Neurol . Oct 2022;21(10):937-946. doi:10.1016/S1474-4422(22)00210-1. https://www.ncbi.nlm.nih.gov/pubmed/36115365
- Khan MA, Al-Jahdali H. The consequences of sleep deprivation on cognitive performance. Neurosciences (Riyadh, Saudi Arabia). Apr 2023;28(2):91-99. doi:10.17712/nsj.2023.2.20220108. https://www.ncbi.nlm.nih.gov/pubmed/37045455
- Tahmasian M, Samea F, Khazaie H, et al. The interrelation of sleep and mental and physical health is anchored in grey-matter neuroanatomy and under genetic control. Commun Biol. Apr 9 2020;3(1):171. doi:10.1038/s42003-020-0892-6. https://www.ncbi.nlm.nih.gov/pubmed/32273564
- Chen WL, Chen JH. Consequences of inadequate sleep during the college years: Sleep deprivation, grade point average, and college graduation. Prev Med. Jul 2019;124:23-28. doi:10.1016/j.ypmed.2019.04.017. https://www.ncbi.nlm.nih.gov/pubmed/31034864
- Hillman D, Mitchell S, Streatfeild J, Burns C, Bruck D, Pezzullo L. The economic cost of inadequate sleep. Sleep. Aug 1 2018;41(8):zsy083. doi:10.1093/sleep/zsy083. https://www.ncbi.nlm.nih.gov/pubmed/29868785
- Jen Fisher, Susan K Hogan, Fields A. Why organizations should prioritize having a well-rested workforce. Deloitte. Accessed Dec. 21, 2023, https://www2.deloitte.com/uk/en/insights/focus/behavioral-economics/sleep-benefits-impact-employee-performance.html
- Newsom R, Wright H. The Link Between Sleep and Job Performance. National Sleep Foundation. Accessed Dec. 21, 2023, https://www.sleepfoundation.org/sleep-hygiene/good-sleep-and-job-performance
- Ramos AR, Wheaton AG, Johnson DA. Sleep Deprivation, Sleep Disorders, and Chronic Disease. Preventing chronic disease. Aug 31 2023;20:E77. doi:10.5888/pcd20.230197. https://www.ncbi.nlm.nih.gov/pubmed/37651644
- Pankowska MM, Lu H, Wheaton AG, et al. Prevalence and Geographic Patterns of Self-Reported Short Sleep Duration Among US Adults, 2020. Preventing chronic disease . Jun 29 2023;20:E53. doi:10.5888/pcd20.220400. https://www.ncbi.nlm.nih.gov/pubmed/37384831
- Nollet M, Franks NP, Wisden W. Understanding Sleep Regulation in Normal and Pathological Conditions, and Why It Matters. J Huntingtons Dis . 2023;12(2):105-119. doi:10.3233/JHD-230564. https://www.ncbi.nlm.nih.gov/pubmed/37302038
- Schwab RJ. Approach to the Patient With Sleep or Wakefulness Disorder. Accessed 9/17/2024, https://www.msdmanuals.com/professional/neurologic-disorders/sleep-and-wakefulness-disorders/approach-to-the-patient-with-a-sleep-or-wakefulness-disorder
- Wright CJ, Milosavljevic S, Pocivavsek A. The stress of losing sleep: Sex-specific neurobiological outcomes. Neurobiology of stress . May 2023;24:100543. doi:10.1016/j.ynstr.2023.100543. https://www.ncbi.nlm.nih.gov/pubmed/37252645
- Leger D, Debellemaniere E, Rabat A, Bayon V, Benchenane K, Chennaoui M. Slow-wave sleep: From the cell to the clinic. Sleep Med Rev . Oct 2018;41:113-132. doi:10.1016/j.smrv.2018.01.008. https://www.ncbi.nlm.nih.gov/pubmed/29490885
- Wilckens KA, Ferrarelli F, Walker MP, Buysse DJ. Slow-Wave Activity Enhancement to Improve Cognition. Trends Neurosci. Jul 2018;41(7):470-482. doi:10.1016/j.tins.2018.03.003. https://www.ncbi.nlm.nih.gov/pubmed/29628198
- Miller CB, Kyle SD, Melehan KL, Bartlett DJ. Methodology for the Assessment of Sleep. Sleep and Affect. 2015:65-90.
- Thomas D, Anderson WM. Multiple Sleep Latency Test (MSLT). In: Kushida CA, ed. Encyclopedia of Sleep. Academic Press; 2013:96-99.
- Zhong X, Gou F, Jiao H, Zhao D, Teng J. Association between night sleep latency and hypertension: A cross-sectional study. Medicine (Baltimore) . Oct 21 2022;101(42):e31250. doi:10.1097/MD.0000000000031250. https://www.ncbi.nlm.nih.gov/pubmed/36281125
- Tsai HJ, Kuo TB, Lin YC, Yang CC. The association between prolonged sleep onset latency and heart rate dynamics among young sleep-onset insomniacs and good sleepers. Psychiatry Res. Dec 30 2015;230(3):892-8. doi:10.1016/j.psychres.2015.11.030. https://www.sciencedirect.com/science/article/abs/pii/S0165178115306983?via%3Dihub
- Ohayon MM. Nocturnal awakenings and difficulty resuming sleep: their burden in the European general population. J Psychosom Res. Dec 2010;69(6):565-71. doi:10.1016/j.jpsychores.2010.03.010. https://www.ncbi.nlm.nih.gov/pubmed/21109044
- Taylor KS, Murai H, Millar PJ, et al. Arousal From Sleep and Sympathetic Excitation During Wakefulness. Hypertension. Dec 2016;68(6):1467-1474. doi:10.1161/HYPERTENSIONAHA.116.08212. https://www.ncbi.nlm.nih.gov/pubmed/27698070
- Wu Y, Huang R, Zhong X, Xiao Y. Cardiovascular Consequences of Repetitive Arousals over the Entire Sleep Duration. Biomed Res Int. 2017;2017:4213861. doi:10.1155/2017/4213861. https://www.ncbi.nlm.nih.gov/pubmed/29018813
- Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. May 2015;14(5):547-58. doi:10.1016/s1474-4422(15)00021-6.
- Conte F, Malloggi S, De Rosa O, et al. Sleep Continuity, Stability and Cyclic Organization Are Impaired in Insomniacs: A Case-Control Study. Int J Environ Res Public Health. Jan 10 2023;20(2)doi:10.3390/ijerph20021240. https://www.ncbi.nlm.nih.gov/pubmed/36673991
- Morin CM, Buysse DJ. Management of Insomnia. N Engl J Med. Jul 18 2024;391(3):247-258. doi:10.1056/NEJMcp2305655. https://www.ncbi.nlm.nih.gov/pubmed/39018534
- Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med. Aug 15 2012;4(147):147ra111. doi:10.1126/scitranslmed.3003748. https://www.ncbi.nlm.nih.gov/pubmed/22896675
- Reddy OC, van der Werf YD. The Sleeping Brain: Harnessing the Power of the Glymphatic System through Lifestyle Choices. Brain Sci . Nov 17 2020;10(11)doi:10.3390/brainsci10110868. https://www.ncbi.nlm.nih.gov/pubmed/33212927
- Bork PAR, Ladron-de-Guevara A, Christensen AH, Jensen KH, Nedergaard M, Bohr T. Astrocyte endfeet may theoretically act as valves to convert pressure oscillations to glymphatic flow. J R Soc Interface . Jul 2023;20(204):20230050. doi:10.1098/rsif.2023.0050. https://www.ncbi.nlm.nih.gov/pubmed/37434503
- Voumvourakis KI, Sideri E, Papadimitropoulos GN, et al. The Dynamic Relationship between the Glymphatic System, Aging, Memory, and Sleep. Biomedicines. Jul 25 2023;11(8)doi:10.3390/biomedicines11082092. https://www.ncbi.nlm.nih.gov/pubmed/37626589
- Gedek A, Koziorowski D, Szlufik S. Assessment of factors influencing glymphatic activity and implications for clinical medicine. Front Neurol. 2023;14:1232304. doi:10.3389/fneur.2023.1232304. https://www.ncbi.nlm.nih.gov/pubmed/37767530
- Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The Glymphatic System: A Beginner's Guide. Neurochem Res. Dec 2015;40(12):2583-99. doi:10.1007/s11064-015-1581-6. https://www.ncbi.nlm.nih.gov/pubmed/25947369
- Wen J, Satyanarayanan SK, Li A, et al. Unraveling the impact of Omega-3 polyunsaturated fatty acids on blood-brain barrier (BBB) integrity and glymphatic function. Brain Behav Immun. Jan 2024;115:335-355. doi:10.1016/j.bbi.2023.10.018. https://www.ncbi.nlm.nih.gov/pubmed/37914102
- Chaput JP, Dutil C, Sampasa-Kanyinga H. Sleeping hours: what is the ideal number and how does age impact this? Nature and science of sleep . 2018;10:421-430. doi:10.2147/NSS.S163071. https://www.ncbi.nlm.nih.gov/pubmed/30568521
- Nikbakhtian S, Reed AB, Obika BD, et al. Accelerometer-derived sleep onset timing and cardiovascular disease incidence: a UK Biobank cohort study. Eur Heart J Digit Health. Dec 2021;2(4):658-666. doi:10.1093/ehjdh/ztab088. https://www.ncbi.nlm.nih.gov/pubmed/36713092
- Buysse DJ. Sleep health: can we define it? Does it matter? Sleep . Jan 1 2014;37(1):9-17. doi:10.5665/sleep.3298. https://www.ncbi.nlm.nih.gov/pubmed/24470692
- Hale L, Troxel W, Buysse DJ. Sleep Health: An Opportunity for Public Health to Address Health Equity. Annu Rev Public Health. Apr 2 2020;41(1):81-99. doi:10.1146/annurev-publhealth-040119-094412. https://www.ncbi.nlm.nih.gov/pubmed/31900098
- van de Langenberg SCN, Kocevska D, Luik AI. The multidimensionality of sleep in population-based samples: a narrative review. J Sleep Res. Aug 2022;31(4):e13608. doi:10.1111/jsr.13608. https://www.ncbi.nlm.nih.gov/pubmed/35429087
- Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep health . Dec 2015;1(4):233-243. doi:10.1016/j.sleh.2015.10.004. https://www.ncbi.nlm.nih.gov/pubmed/29073398
- Desjardins S, Lapierre S, Hudon C, Desgagne A. Factors involved in sleep efficiency: a population-based study of community-dwelling elderly persons. Sleep. May 1 2019;42(5)doi:10.1093/sleep/zsz038. https://www.ncbi.nlm.nih.gov/pubmed/30768200
- Reed DL, Sacco WP. Measuring Sleep Efficiency: What Should the Denominator Be? J Clin Sleep Med. Feb 2016;12(2):263-6. doi:10.5664/jcsm.5498. https://www.ncbi.nlm.nih.gov/pubmed/26194727
- Mentzelou M, Papadopoulou SK, Papandreou D, et al. Evaluating the Relationship between Circadian Rhythms and Sleep, Metabolic and Cardiovascular Disorders: Current Clinical Evidence in Human Studies. Metabolites . Mar 1 2023;13(3)doi:10.3390/metabo13030370. https://www.ncbi.nlm.nih.gov/pubmed/36984810
- Zhang C, Qin G. Irregular sleep and cardiometabolic risk: Clinical evidence and mechanisms. Front Cardiovasc Med. 2023;10:1059257. doi:10.3389/fcvm.2023.1059257. https://www.ncbi.nlm.nih.gov/pubmed/36873401
- Ohayon MM, Chen MC, Bixler E, et al. A provisional tool for the measurement of sleep satisfaction. Sleep health. Feb 2018;4(1):6-12. doi:10.1016/j.sleh.2017.11.002. https://www.ncbi.nlm.nih.gov/pubmed/29332682
- Lenneis A, Das-Friebel A, Tang NKY, et al. The influence of sleep on subjective well-being: An experience sampling study. Emotion . Mar 2024;24(2):451-464. doi:10.1037/emo0001268. https://www.ncbi.nlm.nih.gov/pubmed/37535565
- Wu J, Wu Z, Xie C, et al. A high propensity for excessive daytime sleepiness independent of lifestyle is associated with cognitive performance in community-dwelling older adults. Front Psychiatry. 2023;14:1190353. doi:10.3389/fpsyt.2023.1190353. https://www.ncbi.nlm.nih.gov/pubmed/37636818
- Perez-Carbonell L, Mignot E, Leschziner G, Dauvilliers Y. Understanding and approaching excessive daytime sleepiness. Lancet. Sep 24 2022;400(10357):1033-1046. doi:10.1016/S0140-6736(22)01018-2. https://www.ncbi.nlm.nih.gov/pubmed/36115367
- Bock J, Covassin N, Somers V. Excessive daytime sleepiness: an emerging marker of cardiovascular risk. Heart. Oct 28 2022;108(22):1761-1766. doi:10.1136/heartjnl-2021-319596. https://www.ncbi.nlm.nih.gov/pubmed/35102000
- Gharibi V, Mokarami H, Cousins R, Jahangiri M, Eskandari D. Excessive Daytime Sleepiness and Safety Performance: Comparing Proactive and Reactive Approaches. Int J Occup Environ Med. Apr 2020;11(2):95-107. doi:10.34172/ijoem.2020.1872. https://www.ncbi.nlm.nih.gov/pubmed/32218557
- Pagel JF. Excessive daytime sleepiness. Am Fam Physician. Mar 1 2009;79(5):391-6. https://www.ncbi.nlm.nih.gov/pubmed/19275068
- Lok R, Smolders K, Beersma DGM, de Kort YAW. Light, Alertness, and Alerting Effects of White Light: A Literature Overview. J Biol Rhythms . Dec 2018;33(6):589-601. doi:10.1177/0748730418796443. https://www.ncbi.nlm.nih.gov/pubmed/30191746
- Markun LC, Sampat A. Clinician-Focused Overview and Developments in Polysomnography. Curr Sleep Med Rep. 2020;6(4):309-321. doi:10.1007/s40675-020-00197-5. https://www.ncbi.nlm.nih.gov/pubmed/33251088
- Frase L, Nissen C, Spiegelhalder K, Feige B. The importance and limitations of polysomnography in insomnia disorder-a critical appraisal. J Sleep Res. Dec 2023;32(6):e14036. doi:10.1111/jsr.14036. https://www.ncbi.nlm.nih.gov/pubmed/37680011
- Driller MW, Dunican IC, Omond SET, et al. Pyjamas, Polysomnography and Professional Athletes: The Role of Sleep Tracking Technology in Sport. Sports (Basel). Jan 5 2023;11(1)doi:10.3390/sports11010014. https://www.ncbi.nlm.nih.gov/pubmed/36668718
- Cagle JL, Young BD, Shih MC, et al. Portable Sleep Study Device Versus Polysomnography: A Meta-analysis. Otolaryngol Head Neck Surg . May 2023;168(5):944-955. doi:10.1002/ohn.179. https://www.ncbi.nlm.nih.gov/pubmed/36939562
- Depner CM, Cheng PC, Devine JK, et al. Wearable technologies for developing sleep and circadian biomarkers: a summary of workshop discussions. Sleep. Feb 13 2020;43(2)doi:10.1093/sleep/zsz254. https://www.ncbi.nlm.nih.gov/pubmed/31641776
- De Weerd AW. Actigraphy, the alternative way? Front Psychiatry . 2014;5:155. doi:10.3389/fpsyt.2014.00155. https://www.ncbi.nlm.nih.gov/pubmed/25520671
- Fekedulegn D, Andrew ME, Shi M, Violanti JM, Knox S, Innes KE. Actigraphy-Based Assessment of Sleep Parameters. Ann Work Expo Health . Apr 30 2020;64(4):350-367. doi:10.1093/annweh/wxaa007. https://www.ncbi.nlm.nih.gov/pubmed/32053169
- Walia HK, Mehra R. Practical aspects of actigraphy and approaches in clinical and research domains. Handb Clin Neurol. 2019;160:371-379. doi:10.1016/B978-0-444-64032-1.00024-2. https://www.ncbi.nlm.nih.gov/pubmed/31277861
- Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring Subjective Sleep Quality: A Review. Int J Environ Res Public Health . Jan 26 2021;18(3)doi:10.3390/ijerph18031082. https://www.ncbi.nlm.nih.gov/pubmed/33530453
- Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. May 1989;28(2):193-213. doi:10.1016/0165-1781(89)90047-4. https://www.ncbi.nlm.nih.gov/pubmed/2748771
- Landry GJ, Best JR, Liu-Ambrose T. Measuring sleep quality in older adults: a comparison using subjective and objective methods. Front Aging Neurosci . 2015;7:166. doi:10.3389/fnagi.2015.00166. https://www.ncbi.nlm.nih.gov/pubmed/26441633
- Minich DM, Henning M, Darley C, Fahoum M, Schuler CB, Frame J. Is Melatonin the "Next Vitamin D"?: A Review of Emerging Science, Clinical Uses, Safety, and Dietary Supplements. Nutrients. Sep 22 2022;14(19)doi:10.3390/nu14193934. https://www.ncbi.nlm.nih.gov/pubmed/36235587
- Godfrey S, Iversen HK, West AS. Melatonin profile in healthy, elderly subjects - A systematic literature review. Chronobiol Int. Apr 2022;39(4):476-492. doi:10.1080/07420528.2021.2016794. https://www.ncbi.nlm.nih.gov/pubmed/34983254
- Tortorolo F, Farren F, Rada G. Is melatonin useful for jet lag? Medwave. Dec 21 2015;15 Suppl 3:e6343. doi:10.5867/medwave.2015.6343. https://www.ncbi.nlm.nih.gov/pubmed/26731279
- Zisapel N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br J Pharmacol. Aug 2018;175(16):3190-3199. doi:10.1111/bph.14116. https://www.ncbi.nlm.nih.gov/pubmed/29318587
- Cardinali DP. Melatonin and healthy aging. Vitam Horm. 2021;115:67-88. doi:10.1016/bs.vh.2020.12.004. https://www.ncbi.nlm.nih.gov/pubmed/33706965
- Tuft C, Matar E, Menczel Schrire Z, Grunstein RR, Yee BJ, Hoyos CM. Current Insights into the Risks of Using Melatonin as a Treatment for Sleep Disorders in Older Adults. Clin Interv Aging. 2023;18:49-59. doi:10.2147/CIA.S361519. https://www.ncbi.nlm.nih.gov/pubmed/36660543
- Zhdanova IV, Wurtman RJ. Efficacy of melatonin as a sleep-promoting agent. J Biol Rhythms. Dec 1997;12(6):644-50. doi:10.1177/074873049701200620. https://www.ncbi.nlm.nih.gov/pubmed/9406040
- Zhdanova IV, Wurtman RJ, Lynch HJ, et al. Sleep-inducing effects of low doses of melatonin ingested in the evening. Clin Pharmacol Ther . May 1995;57(5):552-8. doi:10.1016/0009-9236(95)90040-3. https://www.ncbi.nlm.nih.gov/pubmed/7768078
- Costello RB, Lentino CV, Boyd CC, et al. The effectiveness of melatonin for promoting healthy sleep: a rapid evidence assessment of the literature. Nutr J. Nov 7 2014;13:106. doi:10.1186/1475-2891-13-106. https://www.ncbi.nlm.nih.gov/pubmed/25380732
- Brzezinski A, Vangel MG, Wurtman RJ, et al. Effects of exogenous melatonin on sleep: a meta-analysis. Sleep Med Rev. Feb 2005;9(1):41-50. doi:10.1016/j.smrv.2004.06.004. https://www.ncbi.nlm.nih.gov/pubmed/15649737
- Duffy JF, Wang W, Ronda JM, Czeisler CA. High dose melatonin increases sleep duration during nighttime and daytime sleep episodes in older adults. J Pineal Res. Aug 2022;73(1):e12801. doi:10.1111/jpi.12801. https://www.ncbi.nlm.nih.gov/pubmed/35436355
- Mun JG, Wang D, Doerflein Fulk DL, et al. A Randomized, Double-Blind, Crossover Study to Investigate the Pharmacokinetics of Extended-Release Melatonin Compared to Immediate-Release Melatonin in Healthy Adults. J Diet Suppl. May 7 2024;21(2):182-194. doi:10.1080/19390211.2023.2206475. https://www.ncbi.nlm.nih.gov/pubmed/37150895
- Ait Abdellah S, Raverot V, Gal C, et al. Bioavailability of Melatonin after Administration of an Oral Prolonged-Release Tablet and an Immediate-Release Sublingual Spray in Healthy Male Volunteers. Drugs R D . Sep 2023;23(3):257-265. doi:10.1007/s40268-023-00431-9. https://www.ncbi.nlm.nih.gov/pubmed/37438493
- Roman Martinez M, Garcia Aguilar E, Martin Vilchez S, et al. Bioavailability of Oniria((R)), a Melatonin Prolonged-Release Formulation, Versus Immediate-Release Melatonin in Healthy Volunteers. Drugs R D . Sep 2022;22(3):235-243. doi:10.1007/s40268-022-00394-3. https://www.ncbi.nlm.nih.gov/pubmed/35918587
- Barbagallo M, Veronese N, Dominguez LJ. Magnesium in Aging, Health and Diseases. Nutrients. Jan 30 2021;13(2)doi:10.3390/nu13020463. https://www.ncbi.nlm.nih.gov/pubmed/33573164
- Zhang Y, Chen C, Lu L, et al. Association of magnesium intake with sleep duration and sleep quality: findings from the CARDIA study. Sleep. Apr 11 2022;45(4)doi:10.1093/sleep/zsab276. https://www.ncbi.nlm.nih.gov/pubmed/34883514
- Arab A, Rafie N, Amani R, Shirani F. The Role of Magnesium in Sleep Health: a Systematic Review of Available Literature. Biol Trace Elem Res . Jan 2023;201(1):121-128. doi:10.1007/s12011-022-03162-1. https://www.ncbi.nlm.nih.gov/pubmed/35184264
- Held K, Antonijevic IA, Kunzel H, et al. Oral Mg(2+) supplementation reverses age-related neuroendocrine and sleep EEG changes in humans. Pharmacopsychiatry. Jul 2002;35(4):135-43. doi:10.1055/s-2002-33195. https://www.ncbi.nlm.nih.gov/pubmed/12163983
- Abbasi B, Kimiagar M, Sadeghniiat K, Shirazi MM, Hedayati M, Rashidkhani B. The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences . Dec 2012;17(12):1161-9. https://www.ncbi.nlm.nih.gov/pubmed/23853635
- Nielsen FH, Johnson LK, Zeng H. Magnesium supplementation improves indicators of low magnesium status and inflammatory stress in adults older than 51 years with poor quality sleep. Magnes Res. Dec 2010;23(4):158-68. doi:10.1684/mrh.2010.0220. https://www.ncbi.nlm.nih.gov/pubmed/21199787
- Sadir S, Tabassum S, Emad S, et al. Neurobehavioral and biochemical effects of magnesium chloride (MgCl2), magnesium sulphate (MgSO4) and magnesium-L-threonate (MgT) supplementation in rats: A dose dependent comparative study. Pakistan journal of pharmaceutical sciences . Jan 2019;32(1(Supplementary)):277-283. https://www.ncbi.nlm.nih.gov/pubmed/30829204
- Hausenblas HA, Lynch T, Hooper S, Shrestha A, Rosendale D, Gu J. Magnesium-L-threonate improves sleep quality and daytime functioning in adults with self-reported sleep problems: A randomized controlled trial. Sleep Med X. Dec 15 2024;8:100121. doi:10.1016/j.sleepx.2024.100121.
- Kawai N, Sakai N, Okuro M, et al. The sleep-promoting and hypothermic effects of glycine are mediated by NMDA receptors in the suprachiasmatic nucleus. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology . 2015;40(6):1405-1416. doi:10.1038/npp.2014.326. https://www.ncbi.nlm.nih.gov/pubmed/25533534 https://www.ncbi.nlm.nih.gov/pmc/PMC4397399/
- Bannai M, Kawai N. New therapeutic strategy for amino acid medicine: glycine improves the quality of sleep. J Pharmacol Sci. 2012;118(2):145-8. doi:10.1254/jphs.11r04fm. https://www.ncbi.nlm.nih.gov/pubmed/22293292
- Hondo M, Furutani N, Yamasaki M, Watanabe M, Sakurai T. Orexin neurons receive glycinergic innervations. PLoS One. 2011;6(9):e25076. doi:10.1371/journal.pone.0025076. https://www.ncbi.nlm.nih.gov/pubmed/21949857
- Razak MA, Begum PS, Viswanath B, Rajagopal S. Multifarious Beneficial Effect of Nonessential Amino Acid, Glycine: A Review. Oxid Med Cell Longev . 2017;2017:1716701. doi:10.1155/2017/1716701. https://www.ncbi.nlm.nih.gov/pubmed/28337245
- Bannai M, Kawai N, Ono K, Nakahara K, Murakami N. The effects of glycine on subjective daytime performance in partially sleep-restricted healthy volunteers. Frontiers in neurology. 2012;3:61-61. doi:10.3389/fneur.2012.00061. https://www.ncbi.nlm.nih.gov/pubmed/22529837 https://www.ncbi.nlm.nih.gov/pmc/PMC3328957/
- Yamadera W, Inagawa K, Chiba S, Bannai M, Takahashi M, Nakayama K. Glycine ingestion improves subjective sleep quality in human volunteers, correlating with polysomnographic changes. Sleep and Biological Rhythms . 2007;5(2):126-131. doi:10.1111/j.1479-8425.2007.00262.x. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1479-8425.2007.00262.x https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/j.1479-8425.2007.00262.x?download=true
- Inagawa K, Hiraoka T, Kohda T, Yamadera W, Takahashi M. Subjective effects of glycine ingestion before bedtime on sleep quality. Sleep and Biological Rhythms. 2006;4(1):75-77. doi:10.1111/j.1479-8425.2006.00193.x. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1479-8425.2006.00193.x
- Speers AB, Cabey KA, Soumyanath A, Wright KM. Effects of Withania somnifera (Ashwagandha) on Stress and the Stress- Related Neuropsychiatric Disorders Anxiety, Depression, and Insomnia. Current neuropharmacology . 2021;19(9):1468-1495. doi:10.2174/1570159X19666210712151556. https://www.ncbi.nlm.nih.gov/pubmed/34254920
- Cheah KL, Norhayati MN, Husniati Yaacob L, Abdul Rahman R. Effect of Ashwagandha (Withania somnifera) extract on sleep: A systematic review and meta-analysis. PLoS One. 2021;16(9):e0257843. doi:10.1371/journal.pone.0257843. https://www.ncbi.nlm.nih.gov/pubmed/34559859
- Deshpande A, Irani N, Balkrishnan R, Benny IR. A randomized, double blind, placebo controlled study to evaluate the effects of ashwagandha (Withania somnifera) extract on sleep quality in healthy adults. Sleep Med. Aug 2020;72:28-36. doi:10.1016/j.sleep.2020.03.012. https://www.ncbi.nlm.nih.gov/pubmed/32540634
- Langade D, Thakare V, Kanchi S, Kelgane S. Clinical evaluation of the pharmacological impact of ashwagandha root extract on sleep in healthy volunteers and insomnia patients: A double-blind, randomized, parallel-group, placebo-controlled study. J Ethnopharmacol. Jan 10 2021;264:113276. doi:10.1016/j.jep.2020.113276. https://www.ncbi.nlm.nih.gov/pubmed/32818573
- O'Connor J, Lindsay K, Baker C, Kirby J, Hutchins A, Harris M. The Impact of Ashwagandha on Stress, Sleep Quality, and Food Cravings in College Students: Quantitative Analysis of a Double-Blind Randomized Control Trial. J Med Food. Dec 2022;25(12):1086-1094. doi:10.1089/jmf.2022.0040. https://www.ncbi.nlm.nih.gov/pubmed/35984871
- Baker C, Kirby JB, O'Connor J, Lindsay KG, Hutchins A, Harris M. The Perceived Impact of Ashwagandha on Stress, Sleep Quality, Energy, and Mental Clarity for College Students: Qualitative Analysis of a Double-Blind Randomized Control Trial. J Med Food. Dec 2022;25(12):1095-1101. doi:10.1089/jmf.2022.0042. https://www.ncbi.nlm.nih.gov/pubmed/35984870
- Mohan ME, Thomas JV, Mohan MC, Das SS, Prabhakaran P, Pulikkaparambil Sasidharan BC. A proprietary black cumin oil extract (Nigella sativa) (BlaQmax((R))) modulates stress-sleep-immunity axis safely: Randomized double-blind placebo-controlled study. Front Nutr . 2023;10:1152680. doi:10.3389/fnut.2023.1152680. https://www.ncbi.nlm.nih.gov/pubmed/37139438
- Thomas JV, Mohan ME, Prabhakaran P, Das SS, Maliakel B, I MK. A phase I clinical trial to evaluate the safety of thymoquinone-rich black cumin oil (BlaQmax(R)) on healthy subjects: Randomized, double-blinded, placebo-controlled prospective study. Toxicol Rep. 2022;9:999-1007. doi:10.1016/j.toxrep.2022.04.020. https://www.ncbi.nlm.nih.gov/pubmed/36518481
- Das S S, R K, George S, et al. Thymoquinone-rich black cumin oil improves sleep quality, alleviates anxiety/stress on healthy subjects with sleep disturbances– A pilot polysomnography study. Journal of Herbal Medicine . 2022/03/01/ 2022;32:100507. doi:10.1016/j.hermed.2021.100507. https://www.sciencedirect.com/science/article/pii/S2210803321000877
- Kaluzna-Czaplinska J, Gatarek P, Chirumbolo S, Chartrand MS, Bjorklund G. How important is tryptophan in human health? Crit Rev Food Sci Nutr . 2019;59(1):72-88. doi:10.1080/10408398.2017.1357534. https://www.ncbi.nlm.nih.gov/pubmed/28799778
- Bhat A, Pires AS, Tan V, Babu Chidambaram S, Guillemin GJ. Effects of Sleep Deprivation on the Tryptophan Metabolism. Int J Tryptophan Res . 2020;13:1178646920970902. doi:10.1177/1178646920970902. https://www.ncbi.nlm.nih.gov/pubmed/33281456
- Maffei ME. 5-Hydroxytryptophan (5-HTP): Natural Occurrence, Analysis, Biosynthesis, Biotechnology, Physiology and Toxicology. Int J Mol Sci . Dec 26 2020;22(1)doi:10.3390/ijms22010181. https://www.ncbi.nlm.nih.gov/pubmed/33375373
- Lieberman HR, Agarwal S, Fulgoni VL, 3rd. Tryptophan Intake in the US Adult Population Is Not Related to Liver or Kidney Function but Is Associated with Depression and Sleep Outcomes. J Nutr. Dec 2016;146(12):2609S-2615S. doi:10.3945/jn.115.226969. https://www.ncbi.nlm.nih.gov/pubmed/27934652
- van Dalfsen JH, Markus CR. The serotonin transporter gene-linked polymorphic region (5-HTTLPR) and the sleep-promoting effects of tryptophan: A randomized placebo-controlled crossover study. J Psychopharmacol . Aug 2019;33(8):948-954. doi:10.1177/0269881119855978. https://www.ncbi.nlm.nih.gov/pubmed/31237183
- van Dalfsen JH, Markus CR. Interaction between 5-HTTLPR genotype and cognitive stress vulnerability on sleep quality: effects of sub-chronic tryptophan administration. Int J Neuropsychopharmacol. Feb 2 2015;18(3)doi:10.1093/ijnp/pyu057. https://www.ncbi.nlm.nih.gov/pubmed/25644221
- Sutanto CN, Loh WW, Kim JE. The impact of tryptophan supplementation on sleep quality: a systematic review, meta-analysis, and meta-regression. Nutr Rev. Jan 10 2022;80(2):306-316. doi:10.1093/nutrit/nuab027. https://www.ncbi.nlm.nih.gov/pubmed/33942088
- Markus CR, Jonkman LM, Lammers JH, Deutz NE, Messer MH, Rigtering N. Evening intake of alpha-lactalbumin increases plasma tryptophan availability and improves morning alertness and brain measures of attention. Am J Clin Nutr. May 2005;81(5):1026-33. doi:10.1093/ajcn/81.5.1026. https://www.ncbi.nlm.nih.gov/pubmed/15883425
- George CF, Millar TW, Hanly PJ, Kryger MH. The effect of L-tryptophan on daytime sleep latency in normals: correlation with blood levels. Sleep. Aug 1989;12(4):345-53. doi:10.1093/sleep/12.4.345. https://www.ncbi.nlm.nih.gov/pubmed/2669092
- NIH. Chamomile. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury . 2012.
- Hieu TH, Dibas M, Surya Dila KA, et al. Therapeutic efficacy and safety of chamomile for state anxiety, generalized anxiety disorder, insomnia, and sleep quality: A systematic review and meta-analysis of randomized trials and quasi-randomized trials. Phytother Res. Jun 2019;33(6):1604-1615. doi:10.1002/ptr.6349. https://www.ncbi.nlm.nih.gov/pubmed/31006899
- Adib-Hajbaghery M, Mousavi SN. The effects of chamomile extract on sleep quality among elderly people: A clinical trial. Complement Ther Med . Dec 2017;35:109-114. doi:10.1016/j.ctim.2017.09.010. https://www.ncbi.nlm.nih.gov/pubmed/29154054
- Abdullahzadeh M, Matourypour P, Naji SA. Investigation effect of oral chamomilla on sleep quality in elderly people in Isfahan: A randomized control trial. J Educ Health Promot. 2017;6:53. doi:10.4103/jehp.jehp_109_15. https://www.ncbi.nlm.nih.gov/pubmed/28616420
- Chang SM, Chen CH. Effects of an intervention with drinking chamomile tea on sleep quality and depression in sleep disturbed postnatal women: a randomized controlled trial. J Adv Nurs. Feb 2016;72(2):306-15. doi:10.1111/jan.12836. https://www.ncbi.nlm.nih.gov/pubmed/26483209
- Abbasinia H, Alizadeh Z, Vakilian K, Jafari Z, poor P, Ranjbaran M. Effect of Chamomile extract on sleep disorder in menopausal women. The Iranian Journal of Obstetrics, Gynecology and Infertility . 01/01 2016;19:1-7. doi:10.22038/ijogi.2016.7631. https://www.researchgate.net/publication/309266429_Effect_of_Chamomile_extract_on_sleep_disorder_in_menopausal_women
- Li MY, Liu HY, Wu DT, et al. L-Theanine: A Unique Functional Amino Acid in Tea (Camellia sinensis L.) With Multiple Health Benefits and Food Applications. Front Nutr. 2022;9:853846. doi:10.3389/fnut.2022.853846. https://www.ncbi.nlm.nih.gov/pubmed/35445053
- Rao TP, Ozeki M, Juneja LR. In Search of a Safe Natural Sleep Aid. J Am Coll Nutr. 2015;34(5):436-47. doi:10.1080/07315724.2014.926153. https://www.ncbi.nlm.nih.gov/pubmed/25759004
- Hidese S, Ogawa S, Ota M, et al. Effects of L-Theanine Administration on Stress-Related Symptoms and Cognitive Functions in Healthy Adults: A Randomized Controlled Trial. Nutrients. Oct 3 2019;11(10)doi:10.3390/nu11102362. https://www.ncbi.nlm.nih.gov/pubmed/31623400
- Unno K, Tanida N, Ishii N, et al. Anti-stress effect of theanine on students during pharmacy practice: positive correlation among salivary alpha-amylase activity, trait anxiety and subjective stress. Pharmacology, biochemistry, and behavior . Oct 2013;111:128-35. doi:10.1016/j.pbb.2013.09.004. https://www.ncbi.nlm.nih.gov/pubmed/24051231
- Baba Y, Takihara T, Okamura N. Theanine maintains sleep quality in healthy young women by suppressing the increase in caffeine-induced wakefulness after sleep onset. Food Funct. Jul 31 2023;14(15):7109-7116. doi:10.1039/d3fo01247f. https://www.ncbi.nlm.nih.gov/pubmed/37458751
- Huiberts LM, Smolders K. Effects of vitamin D on mood and sleep in the healthy population: Interpretations from the serotonergic pathway. Sleep Med Rev. Feb 2021;55:101379. doi:10.1016/j.smrv.2020.101379. https://www.ncbi.nlm.nih.gov/pubmed/32987320
- Jiang J, Tan H, Xia Z, Li J, Zhou S, Huang T. Serum vitamin D concentrations and sleep disorders: insights from NHANES 2011-2016 and Mendelian Randomization analysis. Sleep Breath. Aug 2024;28(4):1679-1690. doi:10.1007/s11325-024-03031-2. https://www.ncbi.nlm.nih.gov/pubmed/38739211
- Zhao K, Luan X, Liu Y, et al. Low serum 25-hydroxyvitamin D concentrations in chronic insomnia patients and the association with poor treatment outcome at 2months. Clin Chim Acta. Dec 2017;475:147-151. doi:10.1016/j.cca.2017.10.024. https://www.ncbi.nlm.nih.gov/pubmed/29080688
- Massa J, Stone KL, Wei EK, et al. Vitamin D and actigraphic sleep outcomes in older community-dwelling men: the MrOS sleep study. Sleep . Feb 1 2015;38(2):251-7. doi:10.5665/sleep.4408. https://www.ncbi.nlm.nih.gov/pubmed/25581929
- Beydoun MA, Ng AE, Fanelli-Kuczmarski MT, et al. Vitamin D status and its longitudinal association with changes in patterns of sleep among middle-aged urban adults. J Affect Disord. Mar 1 2021;282:858-868. doi:10.1016/j.jad.2020.12.145. https://www.ncbi.nlm.nih.gov/pubmed/33601729
- Wu Z, Hu H, Wang C, et al. Sleep Patterns Modify the Association between Vitamin D Status and Coronary Heart Disease: Results from NHANES 2005-2008. J Nutr. May 2023;153(5):1398-1406. doi:10.1016/j.tjnut.2022.11.028. https://www.ncbi.nlm.nih.gov/pubmed/36863481
- Xie Y, Bai C, Feng Q, Gu D. Serum Vitamin D(3) Concentration, Sleep, and Cognitive Impairment among Older Adults in China. Nutrients . Sep 28 2023;15(19)doi:10.3390/nu15194192. https://www.ncbi.nlm.nih.gov/pubmed/37836477
- Song EK, Wu JR. Associations of Vitamin D Intake and Sleep Quality With Cognitive Dysfunction in Older Adults With Heart Failure. J Cardiovasc Nurs. Jul/Aug 2018;33(4):392-399. doi:10.1097/JCN.0000000000000469. https://www.ncbi.nlm.nih.gov/pubmed/29601370
- Abboud M. Vitamin D Supplementation and Sleep: A Systematic Review and Meta-Analysis of Intervention Studies. Nutrients. Mar 3 2022;14(5)doi:10.3390/nu14051076. https://www.ncbi.nlm.nih.gov/pubmed/35268051
- McCarthy MS, Elshaw EB, Szekely BM, Raju D. A Prospective Cohort Study of Vitamin D Supplementation in AD Soldiers: Preliminary Findings. Mil Med. Mar 1 2019;184(Suppl 1):498-505. doi:10.1093/milmed/usy393. https://www.ncbi.nlm.nih.gov/pubmed/30901440
- Huang W, Shah S, Long Q, Crankshaw AK, Tangpricha V. Improvement of pain, sleep, and quality of life in chronic pain patients with vitamin D supplementation. Clin J Pain. Apr 2013;29(4):341-7. doi:10.1097/AJP.0b013e318255655d. https://www.ncbi.nlm.nih.gov/pubmed/22699141
- Sadat Rafiei SK, Abolghasemi S, Frashidi M, et al. Saffron and Sleep Quality: A Systematic Review of Randomized Controlled Trials. Nutr Metab Insights . 2023;16:11786388231160317. doi:10.1177/11786388231160317. https://www.ncbi.nlm.nih.gov/pubmed/37484523
- Lopresti AL, Smith SJ, Drummond PD. An investigation into an evening intake of a saffron extract (affron(R)) on sleep quality, cortisol, and melatonin concentrations in adults with poor sleep: a randomised, double-blind, placebo-controlled, multi-dose study. Sleep Med. Oct 2021;86:7-18. doi:10.1016/j.sleep.2021.08.001. https://www.ncbi.nlm.nih.gov/pubmed/34438361
- Lopresti AL, Smith SJ, Metse AP, Drummond PD. Effects of saffron on sleep quality in healthy adults with self-reported poor sleep: a randomized, double-blind, placebo-controlled trial. J Clin Sleep Med . Jun 15 2020;16(6):937-947. doi:10.5664/jcsm.8376. https://www.ncbi.nlm.nih.gov/pubmed/32056539
- Pachikian BD, Copine S, Suchareau M, Deldicque L. Effects of Saffron Extract on Sleep Quality: A Randomized Double-Blind Controlled Clinical Trial. Nutrients. Apr 27 2021;13(5)doi:10.3390/nu13051473. https://www.ncbi.nlm.nih.gov/pubmed/33925432
- Umigai N, Takeda R, Mori A. Effect of crocetin on quality of sleep: A randomized, double-blind, placebo-controlled, crossover study. Complement Ther Med. Dec 2018;41:47-51. doi:10.1016/j.ctim.2018.09.003. https://www.ncbi.nlm.nih.gov/pubmed/30477864
- Munirah MP, Norhayati MN, Noraini M. Crocus Sativus for Insomnia: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health . Sep 16 2022;19(18)doi:10.3390/ijerph191811658. https://www.ncbi.nlm.nih.gov/pubmed/36141931
- Li L, Liang T, Jiang T, et al. Gut microbiota: Candidates for a novel strategy for ameliorating sleep disorders. Crit Rev Food Sci Nutr . Jul 21 2024;64(29):10772-10788. doi:10.1080/10408398.2023.2228409. https://www.ncbi.nlm.nih.gov/pubmed/37477274
- Han M, Yuan S, Zhang J. The interplay between sleep and gut microbiota. Brain research bulletin. Mar 2022;180:131-146. doi:10.1016/j.brainresbull.2021.12.016. https://www.ncbi.nlm.nih.gov/pubmed/35032622
- Matenchuk BA, Mandhane PJ, Kozyrskyj AL. Sleep, circadian rhythm, and gut microbiota. Sleep Med Rev. Oct 2020;53:101340. doi:10.1016/j.smrv.2020.101340. https://www.ncbi.nlm.nih.gov/pubmed/32668369
- Lopez-Santamarina A, Mondragon ADC, Cardelle-Cobas A, et al. Effects of Unconventional Work and Shift Work on the Human Gut Microbiota and the Potential of Probiotics to Restore Dysbiosis. Nutrients. Jul 7 2023;15(13)doi:10.3390/nu15133070. https://www.ncbi.nlm.nih.gov/pubmed/37447396
- Boehme M, Remond-Derbez N, Lerond C, et al. Bifidobacterium longum subsp. longum Reduces Perceived Psychological Stress in Healthy Adults: An Exploratory Clinical Trial. Nutrients. Jul 13 2023;15(14)doi:10.3390/nu15143122. https://www.ncbi.nlm.nih.gov/pubmed/37513541
- Rode J, Edebol Carlman HMT, Konig J, et al. Multi-Strain Probiotic Mixture Affects Brain Morphology and Resting State Brain Function in Healthy Subjects: An RCT. Cells. Sep 19 2022;11(18)doi:10.3390/cells11182922. https://www.ncbi.nlm.nih.gov/pubmed/36139496
- Wu SI, Wu CC, Tsai PJ, et al. Psychobiotic Supplementation of PS128(TM) Improves Stress, Anxiety, and Insomnia in Highly Stressed Information Technology Specialists: A Pilot Study. Front Nutr. 2021;8:614105. doi:10.3389/fnut.2021.614105. https://www.ncbi.nlm.nih.gov/pubmed/33842519
- Lee HJ, Hong JK, Kim JK, et al. Effects of Probiotic NVP-1704 on Mental Health and Sleep in Healthy Adults: An 8-Week Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. Jul 30 2021;13(8)doi:10.3390/nu13082660. https://www.ncbi.nlm.nih.gov/pubmed/34444820
- Marotta A, Sarno E, Del Casale A, et al. Effects of Probiotics on Cognitive Reactivity, Mood, and Sleep Quality. Front Psychiatry . 2019;10:164. doi:10.3389/fpsyt.2019.00164. https://www.ncbi.nlm.nih.gov/pubmed/30971965
- Takada M, Nishida K, Gondo Y, et al. Beneficial effects of Lactobacillus casei strain Shirota on academic stress-induced sleep disturbance in healthy adults: a double-blind, randomised, placebo-controlled trial. Benef Microbes. Apr 26 2017;8(2):153-162. doi:10.3920/BM2016.0150. https://www.ncbi.nlm.nih.gov/pubmed/28443383
- Zhu R, Fang Y, Li H, et al. Psychobiotic Lactobacillus plantarum JYLP-326 relieves anxiety, depression, and insomnia symptoms in test anxious college via modulating the gut microbiota and its metabolism. Front Immunol . 2023;14:1158137. doi:10.3389/fimmu.2023.1158137. https://www.ncbi.nlm.nih.gov/pubmed/37033942
- Moloney GM, Long-Smith CM, Murphy A, et al. Improvements in sleep indices during exam stress due to consumption of a Bifidobacterium longum. Brain Behav Immun Health. Jan 2021;10:100174. doi:10.1016/j.bbih.2020.100174. https://www.ncbi.nlm.nih.gov/pubmed/34589719
- Quero CD, Manonelles P, Fernandez M, et al. Differential Health Effects on Inflammatory, Immunological and Stress Parameters in Professional Soccer Players and Sedentary Individuals after Consuming a Synbiotic. A Triple-Blinded, Randomized, Placebo-Controlled Pilot Study. Nutrients. Apr 16 2021;13(4)doi:10.3390/nu13041321. https://www.ncbi.nlm.nih.gov/pubmed/33923663
- Harnett JE, Pyne DB, McKune AJ, Penm J, Pumpa KL. Probiotic supplementation elicits favourable changes in muscle soreness and sleep quality in rugby players. Journal of science and medicine in sport / Sports Medicine Australia . Feb 2021;24(2):195-199. doi:10.1016/j.jsams.2020.08.005. https://www.ncbi.nlm.nih.gov/pubmed/32847731
- Patterson E, Tan HTT, Groeger D, et al. Bifidobacterium longum 1714 improves sleep quality and aspects of well-being in healthy adults: a randomized, double-blind, placebo-controlled clinical trial. Sci Rep . Feb 14 2024;14(1):3725. doi:10.1038/s41598-024-53810-w. https://www.ncbi.nlm.nih.gov/pubmed/38355674
- Irwin C, McCartney D, Desbrow B, Khalesi S. Effects of probiotics and paraprobiotics on subjective and objective sleep metrics: a systematic review and meta-analysis. Eur J Clin Nutr. Nov 2020;74(11):1536-1549. doi:10.1038/s41430-020-0656-x. https://www.ncbi.nlm.nih.gov/pubmed/32433598
- Chu A, Samman S, Galland B, Foster M. Daily consumption of Lactobacillus gasseri CP2305 improves quality of sleep in adults - A systematic literature review and meta-analysis. Clin Nutr. Aug 2023;42(8):1314-1321. doi:10.1016/j.clnu.2023.06.019. https://www.ncbi.nlm.nih.gov/pubmed/37413809
- Gil-Hernandez E, Ruiz-Gonzalez C, Rodriguez-Arrastia M, et al. Effect of gut microbiota modulation on sleep: a systematic review and meta-analysis of clinical trials. Nutr Rev. Nov 10 2023;81(12):1556-1570. doi:10.1093/nutrit/nuad027. https://www.ncbi.nlm.nih.gov/pubmed/37023468
- Benkherouf AY, Eerola K, Soini SL, Uusi-Oukari M. Humulone Modulation of GABA(A) Receptors and Its Role in Hops Sleep-Promoting Activity. Front Neurosci. 2020;14:594708. doi:10.3389/fnins.2020.594708. https://www.ncbi.nlm.nih.gov/pubmed/33177986
- Min B, Ahn Y, Cho HJ, Kwak WK, Jo K, Suh HJ. Chemical compositions and sleep-promoting activities of hop (Humulus lupulus L.) varieties. J Food Sci. May 2023;88(5):2217-2228. doi:10.1111/1750-3841.16544. https://www.ncbi.nlm.nih.gov/pubmed/37038885
- Kyrou I, Christou A, Panagiotakos D, et al. Effects of a hops (Humulus lupulus L.) dry extract supplement on self-reported depression, anxiety and stress levels in apparently healthy young adults: a randomized, placebo-controlled, double-blind, crossover pilot study. Hormones (Athens) . Apr 2017;16(2):171-180. doi:10.14310/horm.2002.1738. https://link.springer.com/content/pdf/10.14310%2Fhorm.2002.1738.pdf
- Fukuda T, Akiyama S, Takahashi K, Iwadate Y, Ano Y. Effect of non-alcoholic beer containing matured hop bitter acids on mood states in healthy adults: A single-arm pilot study. Nurs Health Sci. Mar 2022;24(1):7-16. doi:10.1111/nhs.12898. https://www.ncbi.nlm.nih.gov/pubmed/34741379
- Franco L, Bravo R, Galan C, Rodriguez AB, Barriga C, Cubero J. Effect of non-alcoholic beer on Subjective Sleep Quality in a university stressed population. Acta physiologica Hungarica. Sep 2014;101(3):353-61. doi:10.1556/APhysiol.101.2014.3.10. https://www.ncbi.nlm.nih.gov/pubmed/25183509
- Franco L, Sanchez C, Bravo R, et al. The sedative effect of non-alcoholic beer in healthy female nurses. PLoS One. 2012;7(7):e37290. doi:10.1371/journal.pone.0037290. https://www.ncbi.nlm.nih.gov/pubmed/22815680
- Dimpfel W, Suter A. Sleep improving effects of a single dose administration of a valerian/hops fluid extract - a double blind, randomized, placebo-controlled sleep-EEG study in a parallel design using electrohypnograms. Eur J Med Res. May 26 2008;13(5):200-4. https://www.ncbi.nlm.nih.gov/pubmed/18559301
- Shinjyo N, Waddell G, Green J. Valerian Root in Treating Sleep Problems and Associated Disorders-A Systematic Review and Meta-Analysis. J Evid Based Integr Med. Jan-Dec 2020;25:2515690X20967323. doi:10.1177/2515690X20967323. https://www.ncbi.nlm.nih.gov/pubmed/33086877
- Chandra Shekhar H, Joshua L, Thomas JV. Standardized Extract of Valeriana officinalis Improves Overall Sleep Quality in Human Subjects with Sleep Complaints: A Randomized, Double-Blind, Placebo-Controlled, Clinical Study. Advances in Therapy. 2024/01/01 2024;41(1):246-261. doi:10.1007/s12325-023-02708-6. https://doi.org/10.1007/s12325-023-02708-6 https://pmc.ncbi.nlm.nih.gov/articles/PMC10796483/pdf/12325_2023_Article_2708.pdf
- Schulz H, Stolz C, Muller J. The effect of valerian extract on sleep polygraphy in poor sleepers: a pilot study. Pharmacopsychiatry . Jul 1994;27(4):147-51. doi:10.1055/s-2007-1014295. https://www.ncbi.nlm.nih.gov/pubmed/7972346
- Donath F, Quispe S, Diefenbach K, Maurer A, Fietze I, Roots I. Critical evaluation of the effect of valerian extract on sleep structure and sleep quality. Pharmacopsychiatry. Mar 2000;33(2):47-53. doi:10.1055/s-2000-7972. https://www.ncbi.nlm.nih.gov/pubmed/10761819
- Leathwood PD, Chauffard F, Heck E, Munoz-Box R. Aqueous extract of valerian root (Valeriana officinalis L.) improves sleep quality in man. Pharmacology, biochemistry, and behavior. Jul 1982;17(1):65-71. doi:10.1016/0091-3057(82)90264-7. https://www.ncbi.nlm.nih.gov/pubmed/7122669
- Balderer G, Borbely AA. Effect of valerian on human sleep. Psychopharmacology (Berl) . 1985;87(4):406-9. doi:10.1007/BF00432503. https://www.ncbi.nlm.nih.gov/pubmed/3936097
- Kuhlmann J, Berger W, Podzuweit H, Schmidt U. The influence of valerian treatment on "reaction time, alertness and concentration" in volunteers. Pharmacopsychiatry. Nov 1999;32(6):235-41. doi:10.1055/s-2007-991100. https://www.ncbi.nlm.nih.gov/pubmed/10599933
- Kelley DS, Adkins Y, Laugero KD. A Review of the Health Benefits of Cherries. Nutrients. Mar 17 2018;10(3)doi:10.3390/nu10030368. https://www.ncbi.nlm.nih.gov/pubmed/29562604
- Howatson G, Bell PG, Tallent J, Middleton B, McHugh MP, Ellis J. Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality. Eur J Nutr. Dec 2012;51(8):909-16. doi:10.1007/s00394-011-0263-7. https://www.ncbi.nlm.nih.gov/pubmed/22038497
- Chung J, Choi M, Lee K. Effects of Short-Term Intake of Montmorency Tart Cherry Juice on Sleep Quality after Intermittent Exercise in Elite Female Field Hockey Players: A Randomized Controlled Trial. Int J Environ Res Public Health . Aug 18 2022;19(16)doi:10.3390/ijerph191610272. https://www.ncbi.nlm.nih.gov/pubmed/36011907
- Hillman AR, Trickett O, Brodsky C, Chrismas B. Montmorency tart cherry supplementation does not impact sleep, body composition, cellular health, or blood pressure in healthy adults. Nutr Health. Jul 5 2022:2601060221111230. doi:10.1177/02601060221111230. https://www.ncbi.nlm.nih.gov/pubmed/35790450
- Kimble R, Keane KM, Lodge JK, Cheung W, Haskell-Ramsay CF, Howatson G. Polyphenol-rich tart cherries (Prunus Cerasus, cv Montmorency) improve sustained attention, feelings of alertness and mental fatigue and influence the plasma metabolome in middle-aged adults: a randomised, placebo-controlled trial. Br J Nutr. Feb 3 2022;128(12):1-12. doi:10.1017/S0007114522000460. https://www.ncbi.nlm.nih.gov/pubmed/35109960
- Garrido M, Paredes SD, Cubero J, et al. Jerte Valley cherry-enriched diets improve nocturnal rest and increase 6-sulfatoxymelatonin and total antioxidant capacity in the urine of middle-aged and elderly humans. J Gerontol A Biol Sci Med Sci. Sep 2010;65(9):909-14. doi:10.1093/gerona/glq099. https://www.ncbi.nlm.nih.gov/pubmed/20547498
- Garrido M, Gonzalez-Gomez D, Lozano M, Barriga C, Paredes SD, Rodriguez AB. A Jerte valley cherry product provides beneficial effects on sleep quality. Influence on aging. J Nutr Health Aging. 2013;17(6):553-60. doi:10.1007/s12603-013-0029-4. https://www.ncbi.nlm.nih.gov/pubmed/23732552
- Qian J, Zheng L, Su G, Huang M, Luo D, Zhao M. Identification and Screening of Potential Bioactive Peptides with Sleep-Enhancing Effects in Bovine Milk Casein Hydrolysate. J Agric Food Chem. Sep 29 2021;69(38):11246-11258. doi:10.1021/acs.jafc.1c03937. https://www.ncbi.nlm.nih.gov/pubmed/34543014
- Manna SSS. Possible influence of neurosteroids in the anxiolytic effects of alpha-casozepine. Med Hypotheses. Oct 2021;155:110655. doi:10.1016/j.mehy.2021.110655. https://www.ncbi.nlm.nih.gov/pubmed/34392107
- de Saint-Hilaire ZM, M.; Desor, D.; Kobayashi, T. Effects of a Bovine Alpha S1-Casein Tryptic Hydrolysate (CTH) on Sleep Disorder in Japanese General Population. Open Sleep J. 2009;2:26–32. https://benthamopenarchives.com/abstract.php?ArticleCode=TOSLPJ-2-26
- Kim HJ, Kim J, Lee S, et al. A Double-Blind, Randomized, Placebo-Controlled Crossover Clinical Study of the Effects of Alpha-s1 Casein Hydrolysate on Sleep Disturbance. Nutrients. Jun 27 2019;11(7)doi:10.3390/nu11071466. https://www.ncbi.nlm.nih.gov/pubmed/31252661
- Lim SE, Kim HS, Lee S, et al. Dietary supplementation with Lactium and L-theanine alleviates sleep disturbance in adults: a double-blind, randomized, placebo-controlled clinical study. Front Nutr . 2024;11:1419978. doi:10.3389/fnut.2024.1419978.
- Thiagarajah K, Chee HP, Sit NW. Effect of Alpha-S1-Casein Tryptic Hydrolysate and L-Theanine on Poor Sleep Quality: A Double Blind, Randomized Placebo-Controlled Crossover Trial. Nutrients. Feb 3 2022;14(3)doi:10.3390/nu14030652. https://www.ncbi.nlm.nih.gov/pubmed/35277011
- Zhao M, Tuo H, Wang S, Zhao L. The Effects of Dietary Nutrition on Sleep and Sleep Disorders. Mediators Inflamm. 2020;2020:3142874. doi:10.1155/2020/3142874. https://www.ncbi.nlm.nih.gov/pubmed/32684833
- Pattnaik H, Mir M, Boike S, Kashyap R, Khan SA, Surani S. Nutritional Elements in Sleep. Cureus. Dec 2022;14(12):e32803. doi:10.7759/cureus.32803. https://www.ncbi.nlm.nih.gov/pubmed/36694494
- Patterson RE, Sears DD. Metabolic Effects of Intermittent Fasting. Annu Rev Nutr. Aug 21 2017;37:371-393. doi:10.1146/annurev-nutr-071816-064634. https://www.ncbi.nlm.nih.gov/pubmed/28715993
- Vernia F, Di Ruscio M, Ciccone A, et al. Sleep disorders related to nutrition and digestive diseases: a neglected clinical condition. Int J Med Sci . 2021;18(3):593-603. doi:10.7150/ijms.45512. https://www.ncbi.nlm.nih.gov/pubmed/33437194
- van der Merwe C, Munch M, Kruger R. Chronotype Differences in Body Composition, Dietary Intake and Eating Behavior Outcomes: A Scoping Systematic Review. Adv Nutr. Dec 22 2022;13(6):2357-2405. doi:10.1093/advances/nmac093. https://www.ncbi.nlm.nih.gov/pubmed/36041181
- Chung N, Bin YS, Cistulli PA, Chow CM. Does the Proximity of Meals to Bedtime Influence the Sleep of Young Adults? A Cross-Sectional Survey of University Students. Int J Environ Res Public Health. Apr 14 2020;17(8)doi:10.3390/ijerph17082677. https://www.ncbi.nlm.nih.gov/pubmed/32295235
- Iao SI, Jansen E, Shedden K, et al. Associations between bedtime eating or drinking, sleep duration and wake after sleep onset: findings from the American time use survey. Br J Nutr. Sep 13 2021;127(12):1-10. doi:10.1017/S0007114521003597. https://www.ncbi.nlm.nih.gov/pubmed/34511160
- Desjardins K, Brazeau AS, Strychar I, Rabasa-Lhoret R. Are bedtime nutritional strategies effective in preventing nocturnal hypoglycaemia in patients with type 1 diabetes? Diabetes, obesity & metabolism . Jul 2014;16(7):577-87. doi:10.1111/dom.12232. https://www.ncbi.nlm.nih.gov/pubmed/24320159
- Kinsey AW, Ormsbee MJ. The health impact of nighttime eating: old and new perspectives. Nutrients. Apr 9 2015;7(4):2648-62. doi:10.3390/nu7042648. https://www.ncbi.nlm.nih.gov/pubmed/25859885
- Schattinger CM, Leonard JT, Pappas CL, Ormsbee MJ, Panton LB. The effects of pre-sleep consumption of casein protein on next-morning measures of RMR and appetite compared between sedentary pre- and postmenopausal women. Br J Nutr. Jan 28 2021;125(2):121-128. doi:10.1017/S0007114520001506. https://www.ncbi.nlm.nih.gov/pubmed/32364091
- Madzima TA, Panton LB, Fretti SK, Kinsey AW, Ormsbee MJ. Night-time consumption of protein or carbohydrate results in increased morning resting energy expenditure in active college-aged men. Br J Nutr . Jan 14 2014;111(1):71-7. doi:10.1017/S000711451300192X. https://www.ncbi.nlm.nih.gov/pubmed/23768612
- Bermingham KM, May A, Asnicar F, et al. Snack quality and snack timing are associated with cardiometabolic blood markers: the ZOE PREDICT study. Eur J Nutr. Feb 2024;63(1):121-133. doi:10.1007/s00394-023-03241-6. https://www.ncbi.nlm.nih.gov/pubmed/37709944
- Pacheco DGL. Sleep Foundation: Healthy Bedtime Snacks to Eat Before Sleep. Accessed 10/7/2024, https://www.sleepfoundation.org/nutrition/healthy-bedtime-snacks
- Dashti HS, Scheer FA, Jacques PF, Lamon-Fava S, Ordovas JM. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr. Nov 2015;6(6):648-59. doi:10.3945/an.115.008623. https://www.ncbi.nlm.nih.gov/pubmed/26567190
- Scoditti E, Tumolo MR, Garbarino S. Mediterranean Diet on Sleep: A Health Alliance. Nutrients. Jul 21 2022;14(14)doi:10.3390/nu14142998. https://www.ncbi.nlm.nih.gov/pubmed/35889954
- Zuraikat FM, Wood RA, Barragan R, St-Onge MP. Sleep and Diet: Mounting Evidence of a Cyclical Relationship. Annu Rev Nutr. Oct 11 2021;41:309-332. doi:10.1146/annurev-nutr-120420-021719. https://www.ncbi.nlm.nih.gov/pubmed/34348025
- Ji X, Grandner MA, Liu J. The relationship between micronutrient status and sleep patterns: a systematic review. Public Health Nutr. Mar 2017;20(4):687-701. doi:10.1017/S1368980016002603. https://www.ncbi.nlm.nih.gov/pubmed/27702409
- Mohammadi S, Lotfi K, Mokhtari E, Hajhashemy Z, Heidari Z, Saneei P. Association between Mediterranean dietary pattern with sleep duration, sleep quality and brain derived neurotrophic factor (BDNF) in Iranian adults. Sci Rep. Aug 18 2023;13(1):13493. doi:10.1038/s41598-023-40625-4. https://www.ncbi.nlm.nih.gov/pubmed/37596403
- Mantzorou M, Mentzelou M, Vasios GK, et al. Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population. Antioxidants (Basel). Apr 22 2023;12(5)doi:10.3390/antiox12050983. https://www.ncbi.nlm.nih.gov/pubmed/37237849
- Shiraseb F, Mirzababaei A, Daneshzad E, Khosravinia D, Clark CCT, Mirzaei K. The association of dietary approaches to stop hypertension (DASH) and Mediterranean diet with mental health, sleep quality and chronotype in women with overweight and obesity: a cross-sectional study. Eating and weight disorders : EWD. Jul 3 2023;28(1):57. doi:10.1007/s40519-023-01581-0. https://www.ncbi.nlm.nih.gov/pubmed/37395824
- Sahin-Bodur G, Kemaneci S, Tuncer E, Keser A. Evaluation of the relationship between the Mediterranean diet adherence and sleep quality in adults. Sleep Breath. Mar 2024;28(1):511-518. doi:10.1007/s11325-023-02890-5. https://www.ncbi.nlm.nih.gov/pubmed/37603232
- Tang S, Zhou J, Liu C, et al. Association of plant-based diet index with sleep quality in middle-aged and older adults: The Healthy Dance Study. Sleep health. Oct 2023;9(5):698-703. doi:10.1016/j.sleh.2023.04.003. https://www.ncbi.nlm.nih.gov/pubmed/37280140
- Liu J, Wang W, Wen Y. Association of dietary oxidative balance score and sleep duration with the risk of mortality: prospective study in a representative US population. Public Health Nutr. Oct 2023;26(10):2066-2075. doi:10.1017/S1368980023001155. https://www.ncbi.nlm.nih.gov/pubmed/37309207
- Binks H, G EV, Gupta C, Irwin C, Khalesi S. Effects of Diet on Sleep: A Narrative Review. Nutrients. Mar 27 2020;12(4)doi:10.3390/nu12040936. https://www.ncbi.nlm.nih.gov/pubmed/32230944
- Saidi O, Rochette E, Del Sordo G, et al. Isocaloric Diets with Different Protein-Carbohydrate Ratios: The Effect on Sleep, Melatonin Secretion and Subsequent Nutritional Response in Healthy Young Men. Nutrients . Dec 13 2022;14(24)doi:10.3390/nu14245299. https://www.ncbi.nlm.nih.gov/pubmed/36558458
- Vlahoyiannis A, Giannaki CD, Sakkas GK, Aphamis G, Andreou E. A Systematic Review, Meta-Analysis and Meta-Regression on the Effects of Carbohydrates on Sleep. Nutrients. Apr 14 2021;13(4)doi:10.3390/nu13041283. https://www.ncbi.nlm.nih.gov/pubmed/33919698
- Benton D, Bloxham A, Gaylor C, Young H. Influence of Carbohydrate on the Stages of Sleep – A Meta-Analysis. Current Developments in Nutrition . 2021/06/01/ 2021;5:896. doi:10.1093/cdn/nzab049_009. https://www.sciencedirect.com/science/article/pii/S2475299123114144 https://www.sciencedirect.com/science/article/pii/S2475299123114144?via%3Dihub
- Tang M, Song X, Zhong W, Xie Y, Liu Y, Zhang X. Dietary fiber ameliorates sleep disturbance connected to the gut-brain axis. Food Funct . Nov 28 2022;13(23):12011-12020. doi:10.1039/d2fo01178f. https://www.ncbi.nlm.nih.gov/pubmed/36373848
- Masi D, Spoltore ME, Rossetti R, et al. The Influence of Ketone Bodies on Circadian Processes Regarding Appetite, Sleep and Hormone Release: A Systematic Review of the Literature. Nutrients. Mar 28 2022;14(7)doi:10.3390/nu14071410. https://www.ncbi.nlm.nih.gov/pubmed/35406023
- Barrea L, Verde L, Di Lorenzo C, Savastano S, Colao A, Muscogiuri G. Can the ketogenic diet improve our dreams? Effect of very low-calorie ketogenic diet (VLCKD) on sleep quality. J Transl Med. Jul 18 2023;21(1):479. doi:10.1186/s12967-023-04280-7. https://www.ncbi.nlm.nih.gov/pubmed/37464397
- O'Hearn LA. The therapeutic properties of ketogenic diets, slow-wave sleep, and circadian synchrony. Curr Opin Endocrinol Diabetes Obes . Oct 1 2021;28(5):503-508. doi:10.1097/MED.0000000000000660. https://www.ncbi.nlm.nih.gov/pubmed/34269711
- Lei X, Xu Z, Chen W. Association of oxidative balance score with sleep quality: NHANES 2007-2014. J Affect Disord. Oct 15 2023;339:435-442. doi:10.1016/j.jad.2023.07.040. https://www.ncbi.nlm.nih.gov/pubmed/37442450
- Pereira N, Naufel MF, Ribeiro EB, Tufik S, Hachul H. Influence of Dietary Sources of Melatonin on Sleep Quality: A Review. J Food Sci . Jan 2020;85(1):5-13. doi:10.1111/1750-3841.14952. https://www.ncbi.nlm.nih.gov/pubmed/31856339
- He S, Hasler BP, Chakravorty S. Alcohol and sleep-related problems. Current opinion in psychology. Dec 2019;30:117-122. doi:10.1016/j.copsyc.2019.03.007. https://www.ncbi.nlm.nih.gov/pubmed/31128400
- Lundgaard I, Wang W, Eberhardt A, et al. Beneficial effects of low alcohol exposure, but adverse effects of high alcohol intake on glymphatic function. Sci Rep. Feb 2 2018;8(1):2246. doi:10.1038/s41598-018-20424-y. https://www.ncbi.nlm.nih.gov/pubmed/29396480
- Spadola CE, Guo N, Johnson DA, et al. Evening intake of alcohol, caffeine, and nicotine: night-to-night associations with sleep duration and continuity among African Americans in the Jackson Heart Sleep Study. Sleep . Oct 21 2019;42(11)doi:10.1093/sleep/zsz136. https://www.ncbi.nlm.nih.gov/pubmed/31386152
- Huang L, Zhu W, Li N, et al. Functions and mechanisms of adenosine and its receptors in sleep regulation. Sleep Med. Mar 2024;115:210-217. doi:10.1016/j.sleep.2024.02.012. https://www.ncbi.nlm.nih.gov/pubmed/38373361
- Clark I, Landolt HP. Coffee, caffeine, and sleep: A systematic review of epidemiological studies and randomized controlled trials. Sleep Med Rev . Feb 2017;31:70-78. doi:10.1016/j.smrv.2016.01.006. https://www.ncbi.nlm.nih.gov/pubmed/26899133
- Landolt HP, Werth E, Borbely AA, Dijk DJ. Caffeine intake (200 mg) in the morning affects human sleep and EEG power spectra at night. Brain Res. Mar 27 1995;675(1-2):67-74. doi:10.1016/0006-8993(95)00040-w. https://www.ncbi.nlm.nih.gov/pubmed/7796154
- Shilo L, Sabbah H, Hadari R, et al. The effects of coffee consumption on sleep and melatonin secretion. Sleep Med. May 2002;3(3):271-3. doi:10.1016/s1389-9457(02)00015-1. https://www.ncbi.nlm.nih.gov/pubmed/14592218
- Karacan I, Thornby JI, Anch M, Booth GH, Williams RL, Salis PJ. Dose-related sleep disturbances induced by coffee and caffeine. Clin Pharmacol Ther . Dec 1976;20(6):682-9. doi:10.1002/cpt1976206682. https://www.ncbi.nlm.nih.gov/pubmed/186223
- Ogeil RP, Chakraborty SP, Young AC, Lubman DI. Clinician and patient barriers to the recognition of insomnia in family practice: a narrative summary of reported literature analysed using the theoretical domains framework. BMC Fam Pract. Jan 4 2020;21(1):1. doi:10.1186/s12875-019-1070-0. https://www.ncbi.nlm.nih.gov/pubmed/31901226
- Sweetman A, Frank O, Stocks N, Mukherjee S, Lack L. General practitioner management of comorbid insomnia and sleep apnoea. Aust J Gen Pract . Sep 2023;52(9):607-612. doi:10.31128/AJGP-12-22-6648. https://www.ncbi.nlm.nih.gov/pubmed/37666781
- Morin CM, Jarrin DC. Epidemiology of Insomnia: Prevalence, Course, Risk Factors, and Public Health Burden. Sleep Med Clin. Jun 2022;17(2):173-191. doi:10.1016/j.jsmc.2022.03.003. https://www.ncbi.nlm.nih.gov/pubmed/35659072
- Verbraecken J. More than sleepiness: prevalence and relevance of nonclassical symptoms of obstructive sleep apnea. Curr Opin Pulm Med . Nov 1 2022;28(6):552-558. doi:10.1097/MCP.0000000000000915. https://www.ncbi.nlm.nih.gov/pubmed/36101923
- Melo G, Duarte J, Pauletto P, et al. Bruxism: An umbrella review of systematic reviews. J Oral Rehabil. Jul 2019;46(7):666-690. doi:10.1111/joor.12801. https://www.ncbi.nlm.nih.gov/pubmed/30993738
- Brostrom A, Alimoradi Z, Lind J, Ulander M, Lundin F, Pakpour A. Worldwide estimation of restless legs syndrome: a systematic review and meta-analysis of prevalence in the general adult population. J Sleep Res . Jun 2023;32(3):e13783. doi:10.1111/jsr.13783. https://www.ncbi.nlm.nih.gov/pubmed/36600470
- Vaughan CP, Markland AD, Huang AJ, et al. Considerations for integrated cognitive behavioural treatment for older adults with coexisting nocturia and insomnia. Age Ageing. Feb 2 2022;51(2)doi:10.1093/ageing/afac024. https://www.ncbi.nlm.nih.gov/pubmed/35165690
- Haddad R, Decalf V, Monaghan TF, et al. Nocturia severely impairs the sleep quality of nursing home residents: results from a multi-center study. Geriatr Nurs. Nov-Dec 2022;48:164-168. doi:10.1016/j.gerinurse.2022.09.009. https://www.ncbi.nlm.nih.gov/pubmed/36257221
- Tyagi S, Resnick NM, Clarkson BD, et al. Impact of sleep on chronobiology of micturition among healthy older adults. Am J Physiol Renal Physiol . Oct 1 2023;325(4):F407-F417. doi:10.1152/ajprenal.00025.2023. https://www.ncbi.nlm.nih.gov/pubmed/37560770
- Pauwaert K, Goessaert AS, Ghijselings L, Bower W, Depypere H, Everaert K. Characterizing nocturia among Belgian healthy postmenopausal women: Prevalence, degree of bother, etiology and risk factors for nocturia. Maturitas. Jan 2021;143:41-46. doi:10.1016/j.maturitas.2020.08.008. https://www.ncbi.nlm.nih.gov/pubmed/33308635
- Oelke M, Fangmeyer B, Zinke J, Witt JH. [Nocturia in men with benign prostatic hyperplasia]. Aktuelle Urol. Aug 2018;49(4):319-327. Nykturie beim Benignen Prostatasyndrom. doi:10.1055/a-0650-3700. https://www.ncbi.nlm.nih.gov/pubmed/30086589
- Hafner M, Andersson FL, Burtea T, et al. Assessing the burden of nocturia in the workplace: the associations between nocturnal voiding, subjective well-being, work engagement and productivity. J Med Econ . Sep 2020;23(9):994-1003. doi:10.1080/13696998.2020.1767631. https://www.ncbi.nlm.nih.gov/pubmed/32397770
- Dutoglu E, Soysal P, Smith L, et al. Nocturia and its clinical implications in older women. Arch Gerontol Geriatr. Nov-Dec 2019;85:103917. doi:10.1016/j.archger.2019.103917. https://www.ncbi.nlm.nih.gov/pubmed/31400648
- Endeshaw YW, Schwartz AV, Stone K, et al. Nocturia, Insomnia Symptoms and Mortality among Older Men: The Health, Aging and Body Composition Study. J Clin Sleep Med. Jun 15 2016;12(6):789-96. doi:10.5664/jcsm.5870. https://www.ncbi.nlm.nih.gov/pubmed/26951411
- de Bergeyck R, Geoffroy PA. Insomnia in neurological disorders: Prevalence, mechanisms, impact and treatment approaches. Revue neurologique . Oct 2023;179(7):767-781. doi:10.1016/j.neurol.2023.08.008. https://www.ncbi.nlm.nih.gov/pubmed/37620177
- Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nature and science of sleep. 2017;9:151-161. doi:10.2147/NSS.S134864. https://www.ncbi.nlm.nih.gov/pubmed/28579842
- Enkvist H, Ohman A, Pitkanen M, Nordin M, Nordin S. Stress, mental ill-health and functional somatic syndromes in incident and chronic sleep disturbance in a general adult population. Health Psychol Behav Med . 2023;11(1):2184372. doi:10.1080/21642850.2023.2184372. https://www.ncbi.nlm.nih.gov/pubmed/36925761
- Rothe N, Schulze J, Kirschbaum C, et al. Sleep disturbances in major depressive and burnout syndrome: A longitudinal analysis. Psychiatry Res . Feb 18 2020;286:112868. doi:10.1016/j.psychres.2020.112868. https://www.ncbi.nlm.nih.gov/pubmed/32163819
- Palagini L, Hertenstein E, Riemann D, Nissen C. Sleep, insomnia and mental health. J Sleep Res. Aug 2022;31(4):e13628. doi:10.1111/jsr.13628. https://www.ncbi.nlm.nih.gov/pubmed/35506356
- Comas M, Solis Flores A, Lovato N, et al. The Relationship between Anxiety, Subjective and Objective Sleep, Chronotype and Circadian Rhythms with Depressive Symptoms in Insomnia Disorder. Brain Sci. Apr 4 2023;13(4)doi:10.3390/brainsci13040613. https://www.ncbi.nlm.nih.gov/pubmed/37190578
- Nollet M, Wisden W, Franks NP. Sleep deprivation and stress: a reciprocal relationship. Interface Focus. Jun 6 2020;10(3):20190092. doi:10.1098/rsfs.2019.0092. https://www.ncbi.nlm.nih.gov/pubmed/32382403
- von Gall C, Muth T, Angerer P. Sleep Duration on Workdays Is Correlated with Subjective Workload and Subjective Impact of High Workload on Sleep in Young Healthy Adults. Brain Sci. May 18 2023;13(5)doi:10.3390/brainsci13050818. https://www.ncbi.nlm.nih.gov/pubmed/37239290
- Do D. Trends in the use of medications with insomnia side effects and the implications for insomnia among US adults. J Sleep Res . Aug 2020;29(4):e13075. doi:10.1111/jsr.13075. https://www.ncbi.nlm.nih.gov/pubmed/32410359
- Wichniak A, Wierzbicka A, Walecka M, Jernajczyk W. Effects of Antidepressants on Sleep. Curr Psychiatry Rep. Aug 9 2017;19(9):63. doi:10.1007/s11920-017-0816-4. https://www.ncbi.nlm.nih.gov/pubmed/28791566
- Merrill RM, Ashton MK, Angell E. Sleep disorders related to index and comorbid mental disorders and psychotropic drugs. Annals of general psychiatry . May 27 2023;22(1):23. doi:10.1186/s12991-023-00452-3. https://www.ncbi.nlm.nih.gov/pubmed/37245028
- Hsieh CF, Tseng PT, Chen TY, et al. The association of changes of sleep architecture related to donepezil: A systematic review and meta-analysis. J Formos Med Assoc. Aug 2022;121(8):1466-1477. doi:10.1016/j.jfma.2021.10.013.
- Schredl M, Weber B, Braus D, et al. The effect of rivastigmine on sleep in elderly healthy subjects. Exp Gerontol. Mar 2000;35(2):243-9. doi:10.1016/s0531-5565(00)00077-2.
- Biard K, Douglass AB, De Koninck J. The effects of galantamine and buspirone on sleep structure: Implications for understanding sleep abnormalities in major depression. J Psychopharmacol. Oct 2015;29(10):1106-11. doi:10.1177/0269881115598413.
- Galati A, Brown ES, Bove R, Vaidya A, Gelfand J. Glucocorticoids for therapeutic immunosuppression: Clinical pearls for the practicing neurologist. J Neurol Sci. Nov 15 2021;430:120004. doi:10.1016/j.jns.2021.120004. https://www.ncbi.nlm.nih.gov/pubmed/34598056
- Cole JL. Steroid-Induced Sleep Disturbance and Delirium: A Focused Review for Critically Ill Patients. Fed Pract. Jun 2020;37(6):260-267. https://www.ncbi.nlm.nih.gov/pubmed/32669778
- Cutrufello NJ, Ianus VD, Rowley JA. Opioids and sleep. Curr Opin Pulm Med . Nov 2020;26(6):634-641. doi:10.1097/MCP.0000000000000733. https://www.ncbi.nlm.nih.gov/pubmed/32925368
- Bercovitch RS, Tsai SC. Respiratory medications and sleep. journal article. Current Respiratory Care Reports. June 01 2012;1(2):123-130. doi:10.1007/s13665-012-0013-1. https://doi.org/10.1007/s13665-012-0013-1 https://link.springer.com/content/pdf/10.1007/s13665-012-0013-1.pdf
- Tikhomirova OV, Zybina NN, Kozhevnikova VV. [The effect of long-term beta-blockers on melatonin secretion, sleep quality, and vascular brain damage]. Zh Nevrol Psikhiatr Im S S Korsakova. 2021;121(8):7-12. Vliyanie dlitel'nogo priema beta-adrenoblokatorov na sekretsiyu melatonina, kachestvo sna i sosudistoe porazhenie golovnogo mozga. doi:10.17116/jnevro20211210817. https://www.ncbi.nlm.nih.gov/pubmed/34481429
- Scheer FA, Morris CJ, Garcia JI, et al. Repeated melatonin supplementation improves sleep in hypertensive patients treated with beta-blockers: a randomized controlled trial. Sleep. Oct 1 2012;35(10):1395-402. doi:10.5665/sleep.2122. https://www.ncbi.nlm.nih.gov/pubmed/23024438
- de Mendonca FMR, de Mendonca G, Souza LC, et al. Benzodiazepines and Sleep Architecture: A Systematic Review. CNS & neurological disorders drug targets . 2023;22(2):172-179. doi:10.2174/1871527320666210618103344. https://www.ncbi.nlm.nih.gov/pubmed/34145997
- Kabuto M, Namura I, Saitoh Y. Nocturnal enhancement of plasma melatonin could be suppressed by benzodiazepines in humans. Endocrinol Jpn . Jun 1986;33(3):405-14. doi:10.1507/endocrj1954.33.405. https://www.ncbi.nlm.nih.gov/pubmed/3757924
- Edinoff AN, Nix CA, Hollier J, et al. Benzodiazepines: Uses, Dangers, and Clinical Considerations. Neurol Int. Nov 10 2021;13(4):594-607. doi:10.3390/neurolint13040059. https://www.ncbi.nlm.nih.gov/pubmed/34842811
- Yared L, Rodrigues K, Mangal R, Stead TS, Ganti L. Sleep Hygiene, Daytime Sleepiness, and Coping Mechanisms Amongst US Adults. Cureus . Sep 2023;15(9):e45608. doi:10.7759/cureus.45608. https://www.ncbi.nlm.nih.gov/pubmed/37868531
- Amaral C, Carvalho C, Scaranelo A, Chapman K, Chatkin J, Ferreira I. Cannabis and sleep disorders: not ready for prime time? A qualitative scoping review. J Clin Sleep Med. May 1 2023;19(5):975-990. doi:10.5664/jcsm.10428. https://www.ncbi.nlm.nih.gov/pubmed/36692176
- Maddison KJ, Kosky C, Walsh JH. Is There a Place for Medicinal Cannabis in Treating Patients with Sleep Disorders? What We Know so Far. Nature and science of sleep. 2022;14:957-968. doi:10.2147/NSS.S340949. https://www.ncbi.nlm.nih.gov/pubmed/35611178
- Velzeboer R, Malas A, Boerkoel P, et al. Cannabis dosing and administration for sleep: a systematic review. Sleep. Nov 9 2022;45(11)doi:10.1093/sleep/zsac218. https://www.ncbi.nlm.nih.gov/pubmed/36107800
- Miranda A, Peek E, Ancoli-Israel S, Young JW, Perry W, Minassian A. The Role of Cannabis and The Endocannabinoid System in Sleep Regulation and Cognition: A Review of Human and Animal Studies. Behav Sleep Med . Mar 3 2024;22(2):217-233. doi:10.1080/15402002.2023.2232497. https://www.ncbi.nlm.nih.gov/pubmed/37401160
- Linares IMP, Guimaraes FS, Eckeli A, et al. No Acute Effects of Cannabidiol on the Sleep-Wake Cycle of Healthy Subjects: A Randomized, Double-Blind, Placebo-Controlled, Crossover Study. Front Pharmacol . 2018;9:315. doi:10.3389/fphar.2018.00315. https://www.ncbi.nlm.nih.gov/pubmed/29674967
- Nicholson AN, Turner C, Stone BM, Robson PJ. Effect of Delta-9-tetrahydrocannabinol and cannabidiol on nocturnal sleep and early-morning behavior in young adults. J Clin Psychopharmacol. Jun 2004;24(3):305-13. doi:10.1097/01.jcp.0000125688.05091.8f. https://www.ncbi.nlm.nih.gov/pubmed/15118485
- Pivik RT, Zarcone V, Dement WC, Hollister LE. Delta-9-tetrahydrocannabinol and synhexl: effects on human sleep patterns. Clin Pharmacol Ther. May-Jun 1972;13(3):426-35. doi:10.1002/cpt1972133426. https://www.ncbi.nlm.nih.gov/pubmed/4337346
- AminiLari M, Wang L, Neumark S, et al. Medical cannabis and cannabinoids for impaired sleep: a systematic review and meta-analysis of randomized clinical trials. Sleep. Feb 14 2022;45(2)doi:10.1093/sleep/zsab234. https://www.ncbi.nlm.nih.gov/pubmed/34546363
- Kolla BP, Hayes L, Cox C, Eatwell L, Deyo-Svendsen M, Mansukhani MP. The Effects of Cannabinoids on Sleep. J Prim Care Community Health . Jan-Dec 2022;13:21501319221081277. doi:10.1177/21501319221081277. https://www.ncbi.nlm.nih.gov/pubmed/35459406
- McAlpine T, Mullan B, Clarke PJF. Re-considering the Role of Sleep Hygiene Behaviours in Sleep: Associations Between Sleep Hygiene, Perceptions and Sleep. International journal of behavioral medicine . Oct 2024;31(5):705-717. doi:10.1007/s12529-023-10212-y. https://www.ncbi.nlm.nih.gov/pubmed/37672195
- Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis. Mar-Apr 2023;77:59-69. doi:10.1016/j.pcad.2023.02.005. https://www.ncbi.nlm.nih.gov/pubmed/36841492
- Dressle RJ, Riemann D. Hyperarousal in insomnia disorder: Current evidence and potential mechanisms. J Sleep Res. Dec 2023;32(6):e13928. doi:10.1111/jsr.13928. https://www.ncbi.nlm.nih.gov/pubmed/37183177
- Scullin MK, Krueger ML, Ballard HK, Pruett N, Bliwise DL. The effects of bedtime writing on difficulty falling asleep: A polysomnographic study comparing to-do lists and completed activity lists. J Exp Psychol Gen . Jan 2018;147(1):139-146. doi:10.1037/xge0000374. https://www.ncbi.nlm.nih.gov/pubmed/29058942
- McMahon WR, Ftouni S, Phillips AJK, et al. The impact of structured sleep schedules prior to an in-laboratory study: Individual differences in sleep and circadian timing. PLoS One. 2020;15(8):e0236566. doi:10.1371/journal.pone.0236566. https://www.ncbi.nlm.nih.gov/pubmed/32785281
- Garefelt J, Gershagen S, Kecklund G, Westerlund H, Platts LG. How does cessation of work affect sleep? Prospective analyses of sleep duration, timing and efficiency from the Swedish Retirement Study. J Sleep Res . Jun 2021;30(3):e13157. doi:10.1111/jsr.13157. https://www.ncbi.nlm.nih.gov/pubmed/32815209
- Seton C, Fitzgerald DA. Chronic sleep deprivation in teenagers: Practical ways to help. Paediatr Respir Rev. Dec 2021;40:73-79. doi:10.1016/j.prrv.2021.05.001. https://www.ncbi.nlm.nih.gov/pubmed/34144910
- Chaput JP, Dutil C, Featherstone R, et al. Sleep timing, sleep consistency, and health in adults: a systematic review. Appl Physiol Nutr Metab . Oct 2020;45(10 (Suppl. 2)):S232-S247. doi:10.1139/apnm-2020-0032. https://www.ncbi.nlm.nih.gov/pubmed/33054339
- Pizinger TM, Aggarwal B, St-Onge MP. Sleep Extension in Short Sleepers: An Evaluation of Feasibility and Effectiveness for Weight Management and Cardiometabolic Disease Prevention. Front Endocrinol (Lausanne) . 2018;9:392. doi:10.3389/fendo.2018.00392. https://www.ncbi.nlm.nih.gov/pubmed/30072950
- Niu CC, Bao WJ, Jiang HX, Yu J. The Effect of Nighttime Snacking on Cognitive Function in Older Adults: Evidence from Observational and Experimental Studies. Nutrients. Nov 19 2022;14(22)doi:10.3390/nu14224900. https://www.ncbi.nlm.nih.gov/pubmed/36432586
- St-Onge MP, Mikic A, Pietrolungo CE. Effects of Diet on Sleep Quality. Adv Nutr. Sep 2016;7(5):938-49. doi:10.3945/an.116.012336. https://www.ncbi.nlm.nih.gov/pubmed/27633109
- Basner M, Smith MG, Jones CW, et al. Associations of bedroom PM(2.5), CO(2), temperature, humidity, and noise with sleep: An observational actigraphy study. Sleep health. Jun 2023;9(3):253-263. doi:10.1016/j.sleh.2023.02.010. https://www.ncbi.nlm.nih.gov/pubmed/37076419
- Billings ME, Hale L, Johnson DA. Physical and Social Environment Relationship With Sleep Health and Disorders. Chest. May 2020;157(5):1304-1312. doi:10.1016/j.chest.2019.12.002. https://www.ncbi.nlm.nih.gov/pubmed/31870910
- Caggiari G, Talesa GR, Toro G, Jannelli E, Monteleone G, Puddu L. What type of mattress should be chosen to avoid back pain and improve sleep quality? Review of the literature. J Orthop Traumatol. Dec 8 2021;22(1):51. doi:10.1186/s10195-021-00616-5. https://www.ncbi.nlm.nih.gov/pubmed/34878594
- Surman CBH, Walsh DM. Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches. Brain Sci. Oct 16 2021;11(10)doi:10.3390/brainsci11101361. https://www.ncbi.nlm.nih.gov/pubmed/34679425
- Bolic Baric V, Skuthalla S, Pettersson M, Gustafsson PA, Kjellberg A. The effectiveness of weighted blankets on sleep and everyday activities - A retrospective follow-up study of children and adults with attention deficit hyperactivity disorder and/or autism spectrum disorder. Scand J Occup Ther. Nov 2023;30(8):1357-1367. doi:10.1080/11038128.2021.1939414. https://www.ncbi.nlm.nih.gov/pubmed/34184958
- Lonn M, Svedberg P, Nygren J, Jarbin H, Aili K, Larsson I. The efficacy of weighted blankets for sleep in children with attention-deficit/hyperactivity disorder-A randomized controlled crossover trial. J Sleep Res. Apr 2024;33(2):e13990. doi:10.1111/jsr.13990. https://www.ncbi.nlm.nih.gov/pubmed/37452697
- Hjort Telhede E, Arvidsson S, Karlsson S, Ivarsson A. Weighted Blankets' Effect on the Health of Older People Living in Nursing Homes. Geriatrics (Basel). Jul 29 2022;7(4)doi:10.3390/geriatrics7040079. https://www.ncbi.nlm.nih.gov/pubmed/36005255
- Meth EMS, Brandao LEM, van Egmond LT, et al. A weighted blanket increases pre-sleep salivary concentrations of melatonin in young, healthy adults. J Sleep Res. Apr 2023;32(2):e13743. doi:10.1111/jsr.13743. https://www.ncbi.nlm.nih.gov/pubmed/36184925
- Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. Journal of physiological anthropology. May 31 2012;31(1):14. doi:10.1186/1880-6805-31-14. https://www.ncbi.nlm.nih.gov/pubmed/22738673
- Foundation S. Best Temperature for Sleep. Accessed 11/06/2023, https://www.sleepfoundation.org/bedroom-environment/best-temperature-for-sleep
- Cleveland Clinic. What’s the Best Temperature for Sleep? Accessed 9/30/2024, https://health.clevelandclinic.org/what-is-the-ideal-sleeping-temperature-for-my-bedroom
- Ko Y, Lee JY. Effects of feet warming using bed socks on sleep quality and thermoregulatory responses in a cool environment. Journal of physiological anthropology . Apr 24 2018;37(1):13. doi:10.1186/s40101-018-0172-z. https://www.ncbi.nlm.nih.gov/pubmed/29699592
- Lamport DJ, Breese E, Giao MS, Chandra S, Orchard F. Can air purification improve sleep quality? A 2-week randomised-controlled crossover pilot study in healthy adults. J Sleep Res. Jun 2023;32(3):e13782. doi:10.1111/jsr.13782. https://www.ncbi.nlm.nih.gov/pubmed/36351665
- Mishra AK, van Ruitenbeek AM, Loomans M, Kort HSM. Window/door opening-mediated bedroom ventilation and its impact on sleep quality of healthy, young adults. Indoor Air. Mar 2018;28(2):339-351. doi:10.1111/ina.12435. https://www.ncbi.nlm.nih.gov/pubmed/29164702
- Smith MG, Cordoza M, Basner M. Environmental Noise and Effects on Sleep: An Update to the WHO Systematic Review and Meta-Analysis. Environ Health Perspect . Jul 2022;130(7):76001. doi:10.1289/EHP10197. https://www.ncbi.nlm.nih.gov/pubmed/35857401
- Riedy SM, Smith MG, Rocha S, Basner M. Noise as a sleep aid: A systematic review. Sleep Med Rev. Feb 2021;55:101385. doi:10.1016/j.smrv.2020.101385. https://www.ncbi.nlm.nih.gov/pubmed/33007706
- Shih CY, Gordon CJ, Chen TJ, et al. Comparative efficacy of nonpharmacological interventions on sleep quality in people who are critically ill: A systematic review and network meta-analysis. Int J Nurs Stud . Jun 2022;130:104220. doi:10.1016/j.ijnurstu.2022.104220. https://www.ncbi.nlm.nih.gov/pubmed/35395573
- Cho Y, Ryu SH, Lee BR, Kim KH, Lee E, Choi J. Effects of artificial light at night on human health: A literature review of observational and experimental studies applied to exposure assessment. Chronobiol Int . 2015;32(9):1294-310. doi:10.3109/07420528.2015.1073158.
- Mason IC, Grimaldi D, Reid KJ, et al. Light exposure during sleep impairs cardiometabolic function. Proc Natl Acad Sci U S A. Mar 22 2022;119(12):e2113290119. doi:10.1073/pnas.2113290119. https://pmc.ncbi.nlm.nih.gov/articles/PMC8944904/pdf/pnas.202113290.pdf
- Greco V, Bergamo D, Cuoccio P, Konkoly KR, Munoz Lombardo K, Lewis PA. Wearing an eye mask during overnight sleep improves episodic learning and alertness. Sleep. Mar 9 2023;46(3)doi:10.1093/sleep/zsac305. https://www.ncbi.nlm.nih.gov/pubmed/36521010
- Xie Y, Liu S, Chen XJ, Yu HH, Yang Y, Wang W. Effects of Exercise on Sleep Quality and Insomnia in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front Psychiatry. 2021;12:664499. doi:10.3389/fpsyt.2021.664499. https://www.ncbi.nlm.nih.gov/pubmed/34163383
- Wu J, Yang D, Yang F. Exercise may not just be good for sleep; It can also help lower cardiovascular event risk. Curr Probl Cardiol . Jan 2024;49(1 Pt B):102166. doi:10.1016/j.cpcardiol.2023.102166. https://www.ncbi.nlm.nih.gov/pubmed/37871708
- Solis-Navarro L, Masot O, Torres-Castro R, et al. Effects on Sleep Quality of Physical Exercise Programs in Older Adults: A Systematic Review and Meta-Analysis. Clocks Sleep. Mar 23 2023;5(2):152-166. doi:10.3390/clockssleep5020014. https://www.ncbi.nlm.nih.gov/pubmed/37092426
- He XF, Liu DX, Zhang Q, et al. Voluntary Exercise Promotes Glymphatic Clearance of Amyloid Beta and Reduces the Activation of Astrocytes and Microglia in Aged Mice. Frontiers in molecular neuroscience . 2017;10:144. doi:10.3389/fnmol.2017.00144. https://www.ncbi.nlm.nih.gov/pubmed/28579942
- von Holstein-Rathlou S, Petersen NC, Nedergaard M. Voluntary running enhances glymphatic influx in awake behaving, young mice. Neurosci Lett . Jan 1 2018;662:253-258. doi:10.1016/j.neulet.2017.10.035. https://www.ncbi.nlm.nih.gov/pubmed/29079431
- Yue T, Liu X, Gao Q, Wang Y. Different Intensities of Evening Exercise on Sleep in Healthy Adults: A Systematic Review and Network Meta-Analysis. Nature and science of sleep. 2022;14:2157-2177. doi:10.2147/NSS.S388863. https://www.ncbi.nlm.nih.gov/pubmed/36540196
- Frimpong E, Mograss M, Zvionow T, Dang-Vu TT. The effects of evening high-intensity exercise on sleep in healthy adults: A systematic review and meta-analysis. Sleep Med Rev. Dec 2021;60:101535. doi:10.1016/j.smrv.2021.101535. https://www.ncbi.nlm.nih.gov/pubmed/34416428
- Stutz J, Eiholzer R, Spengler CM. Effects of Evening Exercise on Sleep in Healthy Participants: A Systematic Review and Meta-Analysis. Sports Med . Feb 2019;49(2):269-287. doi:10.1007/s40279-018-1015-0. https://www.ncbi.nlm.nih.gov/pubmed/30374942
- Fernandez FX. Current Insights into Optimal Lighting for Promoting Sleep and Circadian Health: Brighter Days and the Importance of Sunlight in the Built Environment. Nature and science of sleep. 2022;14:25-39. doi:10.2147/NSS.S251712. https://www.ncbi.nlm.nih.gov/pubmed/35023979
- Park HR, Choi SJ, Jo H, Cho JW, Joo EY. Effects of Evening Exposure to Light from Organic Light-Emitting Diodes on Melatonin and Sleep. J Clin Neurol. Jul 2020;16(3):401-407. doi:10.3988/jcn.2020.16.3.401. https://www.ncbi.nlm.nih.gov/pubmed/32657060
- Shechter A, Quispe KA, Mizhquiri Barbecho JS, Slater C, Falzon L. Interventions to reduce short-wavelength ("blue") light exposure at night and their effects on sleep: A systematic review and meta-analysis. Sleep Adv. 2020;1(1):zpaa002. doi:10.1093/sleepadvances/zpaa002. https://www.ncbi.nlm.nih.gov/pubmed/37192881
- Singh S, Keller PR, Busija L, et al. Blue-light filtering spectacle lenses for visual performance, sleep, and macular health in adults. Cochrane Database Syst Rev. Aug 18 2023;8(8):CD013244. doi:10.1002/14651858.CD013244.pub2. https://www.ncbi.nlm.nih.gov/pubmed/37593770
- Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic Physiol Opt . Nov 2017;37(6):644-654. doi:10.1111/opo.12406. https://www.ncbi.nlm.nih.gov/pubmed/29044670
- Jahrami H. The Relationship between Nomophobia, Insomnia, Chronotype, Phone in Proximity, Screen Time, and Sleep Duration in Adults: A Mobile Phone App-Assisted Cross-Sectional Study. Healthcare (Basel, Switzerland) . May 22 2023;11(10)doi:10.3390/healthcare11101503. https://www.ncbi.nlm.nih.gov/pubmed/37239789
- Dresp-Langley B, Hutt A. Digital Addiction and Sleep. Int J Environ Res Public Health . Jun 5 2022;19(11)doi:10.3390/ijerph19116910. https://www.ncbi.nlm.nih.gov/pubmed/35682491
- Silva SSD, Silveira M, Almeida HCR, Nascimento M, Santos M, Heimer MV. Use of digital screens by adolescents and association on sleep quality: a systematic review. Cadernos de saude publica. 2022;38(10):e00300721. doi:10.1590/0102-311XEN300721. https://www.ncbi.nlm.nih.gov/pubmed/36259788
- Albakri U, Drotos E, Meertens R. Sleep Health Promotion Interventions and Their Effectiveness: An Umbrella Review. Int J Environ Res Public Health . May 21 2021;18(11)doi:10.3390/ijerph18115533. https://www.ncbi.nlm.nih.gov/pubmed/34064108
- Rusch HL, Rosario M, Levison LM, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. Jun 2019;1445(1):5-16. doi:10.1111/nyas.13996. https://www.ncbi.nlm.nih.gov/pubmed/30575050
- Doty TJ, Stekl EK, Bohn M, Klosterman G, Simonelli G, Collen J. A 2022 Survey of Commercially Available Smartphone Apps for Sleep: Most Enhance Sleep. Sleep Med Clin. Sep 2023;18(3):373-384. doi:10.1016/j.jsmc.2023.05.008. https://www.ncbi.nlm.nih.gov/pubmed/37532376
- O'Daffer A, Colt SF, Wasil AR, Lau N. Efficacy and Conflicts of Interest in Randomized Controlled Trials Evaluating Headspace and Calm Apps: Systematic Review. Review. JMIR Ment Health. Sep 20 2022;9(9):e40924. doi:10.2196/40924. https://www.ncbi.nlm.nih.gov/pubmed/36125880
- Dadmehr M, Akhtari E, Haqiqi M. The effect of music on the improvement of sleep quality: a report from the viewpoint of Jorjani. Neurol Sci . May 2023;44(5):1787-1789. doi:10.1007/s10072-023-06702-2. https://www.ncbi.nlm.nih.gov/pubmed/36840854
- de Niet G, Tiemens B, Lendemeijer B, Hutschemaekers G. Music-assisted relaxation to improve sleep quality: meta-analysis. J Adv Nurs . Jul 2009;65(7):1356-64. doi:10.1111/j.1365-2648.2009.04982.x. https://www.ncbi.nlm.nih.gov/pubmed/19456998
- Wu WW, Kwong E, Lan XY, Jiang XY. The Effect of a Meditative Movement Intervention on Quality of Sleep in the Elderly: A Systematic Review and Meta-Analysis. J Altern Complement Med. Sep 2015;21(9):509-19. doi:10.1089/acm.2014.0251. https://www.ncbi.nlm.nih.gov/pubmed/26120865
- Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Before-bedtime passive body heating by warm shower or bath to improve sleep: A systematic review and meta-analysis. Sleep Med Rev. Aug 2019;46:124-135. doi:10.1016/j.smrv.2019.04.008. https://www.ncbi.nlm.nih.gov/pubmed/31102877
- Dawson SC, Krakow B, Haynes PL, Rojo-Wissar DM, McIver ND, Ulibarri VA. Use of Sleep Aids in Insomnia: The Role of Time Monitoring Behavior. Prim Care Companion CNS Disord. May 16 2023;25(3)doi:10.4088/PCC.22m03344. https://www.ncbi.nlm.nih.gov/pubmed/37227396
- Vochem J, Strobel C, Maier L, et al. Pre-Sleep Arousal Scale (PSAS) and the Time Monitoring Behavior-10 scale (TMB-10) in good sleepers and patients with insomnia. Sleep Med. Apr 2019;56:98-103. doi:10.1016/j.sleep.2019.01.022. https://www.ncbi.nlm.nih.gov/pubmed/30853192
- Bani Issa W, Hijazi H, Radwan H, et al. Evaluation of the effectiveness of sleep hygiene education and FITBIT devices on quality of sleep and psychological worry: a pilot quasi-experimental study among first-year college students. Front Public Health. 2023;11:1182758. doi:10.3389/fpubh.2023.1182758. https://www.ncbi.nlm.nih.gov/pubmed/37680271
- Lukowski AF, Tsukerman D. Temperament, sleep quality, and insomnia severity in university students: Examining the mediating and moderating role of sleep hygiene. PLoS One. 2021;16(7):e0251557. doi:10.1371/journal.pone.0251557. https://www.ncbi.nlm.nih.gov/pubmed/34264959
- Polat F, Karasu F. Effect of sleep hygiene training given to elderly individuals on daytime sleepiness and fatigue: A randomized controlled trial. Perspect Psychiatr Care. Oct 2022;58(4):2161-2169. doi:10.1111/ppc.13043. https://www.ncbi.nlm.nih.gov/pubmed/35124807
- Souilm N, Elsakhy NM, Alotaibi YA, Ali SAO. Effectiveness of emotional freedom techniques (EFT) vs sleep hygiene education group therapy (SHE) in management of sleep disorders among elderly. Sci Rep. Apr 20 2022;12(1):6521. doi:10.1038/s41598-022-10456-w. https://www.ncbi.nlm.nih.gov/pubmed/35444166
- Pasquier F, Pla R, Bosquet L, Sauvet F, Nedelec M, Consortium DD. The Impact of Multisession Sleep-Hygiene Strategies on Sleep Parameters in Elite Swimmers. Int J Sports Physiol Perform. Nov 1 2023;18(11):1304-1312. doi:10.1123/ijspp.2023-0018. https://www.ncbi.nlm.nih.gov/pubmed/37709276
- Lever JR, Murphy AP, Duffield R, Fullagar HHK. A Combined Sleep Hygiene and Mindfulness Intervention to Improve Sleep and Well-Being During High-Performance Youth Tennis Tournaments. Int J Sports Physiol Perform . Feb 1 2021;16(2):250-258. doi:10.1123/ijspp.2019-1008. https://www.ncbi.nlm.nih.gov/pubmed/32781440
- Caia J, Scott TJ, Halson SL, Kelly VG. The influence of sleep hygiene education on sleep in professional rugby league athletes. Sleep health . Aug 2018;4(4):364-368. doi:10.1016/j.sleh.2018.05.002. https://www.ncbi.nlm.nih.gov/pubmed/30031530
- Shriane AE, Rigney G, Ferguson SA, Bin YS, Vincent GE. Healthy sleep practices for shift workers: consensus sleep hygiene guidelines using a Delphi methodology. Sleep. Dec 11 2023;46(12)doi:10.1093/sleep/zsad182. https://www.ncbi.nlm.nih.gov/pubmed/37429599
- Lee YC, Lu CT, Cheng WN, Li HY. The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare (Basel, Switzerland). Sep 13 2022;10(9)doi:10.3390/healthcare10091755. https://www.ncbi.nlm.nih.gov/pubmed/36141367
- Ali MM, Ellison M, Iweala OI, Spector AR. A sleep clinician's guide to runny noses: evaluation and management of chronic rhinosinusitis to improve sleep apnea care in adults. J Clin Sleep Med. Aug 1 2023;19(8):1545-1552. doi:10.5664/jcsm.10608. https://www.ncbi.nlm.nih.gov/pubmed/37082825
- Irawati N, Wardani RS, Poerbonegoro NL, Rahmawati I. Sleep Disturbance in Chronic Rhinitis: Evaluation of Nasal Symptoms, Sleep Disorder Questionnaires, and Sleep Architecture in Allergic and Non-allergic Rhinitis in Dr. Cipto Mangunkusumo Hospital. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India . Sep 2023;75(3):1888-1893. doi:10.1007/s12070-023-03783-5. https://www.ncbi.nlm.nih.gov/pubmed/37636688
- Schroeder K, Gurenlian JR. Recognizing Poor Sleep Quality Factors During Oral Health Evaluations. Clin Med Res. Jun 2019;17(1-2):20-28. doi:10.3121/cmr.2019.1465. https://www.ncbi.nlm.nih.gov/pubmed/31160475
- Cai Y, Goldberg AN, Chang JL. The Nose and Nasal Breathing in Sleep Apnea. Otolaryngol Clin North Am. Jun 2020;53(3):385-395. doi:10.1016/j.otc.2020.02.002. https://www.ncbi.nlm.nih.gov/pubmed/32192710
- Camacho M, Malu OO, Kram YA, et al. Nasal Dilators (Breathe Right Strips and NoZovent) for Snoring and OSA: A Systematic Review and Meta-Analysis. Pulm Med. 2016;2016:4841310. doi:10.1155/2016/4841310. https://www.ncbi.nlm.nih.gov/pubmed/28070421
- Gelardi M, Porro G, Sterlicchio B, Quaranta N, Ciprandi G, Group On Sonoring IS. Internal and external nasal dilatator in patients who snore: a comparison in clinical practice. Acta bio-medica : Atenei Parmensis . Jan 11 2019;90(2-S):10-4. doi:10.23750/abm.v90i2-S.8096. https://www.ncbi.nlm.nih.gov/pubmed/30715031
- Faridzadeh A, Salimi Y, Ghasemirad H, et al. Neuroprotective Potential of Aromatic Herbs: Rosemary, Sage, and Lavender. Front Neurosci . 2022;16:909833. doi:10.3389/fnins.2022.909833. https://www.ncbi.nlm.nih.gov/pubmed/35873824
- Luo J, Jiang W. A critical review on clinical evidence of the efficacy of lavender in sleep disorders. Phytother Res. Jun 2022;36(6):2342-2351. doi:10.1002/ptr.7448. https://www.ncbi.nlm.nih.gov/pubmed/35412693
- Cheong MJ, Kim S, Kim JS, et al. A systematic literature review and meta-analysis of the clinical effects of aroma inhalation therapy on sleep problems. Medicine (Baltimore). Mar 5 2021;100(9):e24652. doi:10.1097/MD.0000000000024652. https://www.ncbi.nlm.nih.gov/pubmed/33655928
- Chen TY, Hiyama A, Muramatsu M, Hinotsu A. The Effect of Lavender on Sleep Quality in Individuals Without Insomnia: A Systematic Review. Holistic nursing practice. Jul-Aug 01 2022;36(4):223-231. doi:10.1097/HNP.0000000000000528. https://www.ncbi.nlm.nih.gov/pubmed/35708558
- Sazawa K, Kawada S, Ogawa Y. Effects of nighttime lavender aromatherapy on mood and physiological indices of stress in healthy young females. Journal of physical therapy science. Jul 2022;34(7):503-508. doi:10.1589/jpts.34.503. https://www.ncbi.nlm.nih.gov/pubmed/35784602
- Lillehei AS, Halcon LL, Savik K, Reis R. Effect of Inhaled Lavender and Sleep Hygiene on Self-Reported Sleep Issues: A Randomized Controlled Trial. J Altern Complement Med. Jul 2015;21(7):430-8. doi:10.1089/acm.2014.0327. https://www.ncbi.nlm.nih.gov/pubmed/26133206
- Hirokawa K, Nishimoto T, Taniguchi T. Effects of lavender aroma on sleep quality in healthy Japanese students. Perceptual and motor skills . Feb 2012;114(1):111-22. doi:10.2466/13.15.PMS.114.1.111-122. https://www.ncbi.nlm.nih.gov/pubmed/22582680
- Kavurmaci M, Sariaslan A, Yildiz I. Determination the effects of lavender oil quality of sleep and fatigue of students. Perspect Psychiatr Care . Jul 2022;58(3):1013-1020. doi:10.1111/ppc.12892. https://www.ncbi.nlm.nih.gov/pubmed/34114222
- Ko LW, Su CH, Yang MH, Liu SY, Su TP. A pilot study on essential oil aroma stimulation for enhancing slow-wave EEG in sleeping brain. Sci Rep . Jan 13 2021;11(1):1078. doi:10.1038/s41598-020-80171-x. https://www.ncbi.nlm.nih.gov/pubmed/33441798
- Goel N, Kim H, Lao RP. An olfactory stimulus modifies nighttime sleep in young men and women. Chronobiol Int. 2005;22(5):889-904. doi:10.1080/07420520500263276. https://www.ncbi.nlm.nih.gov/pubmed/16298774
- Velasco-Rodriguez R, Perez-Hernandez MG, Maturano-Melgoza JA, et al. The effect of aromatherapy with lavender (Lavandula angustifolia) on serum melatonin levels. Complement Ther Med. Dec 2019;47:102208. doi:10.1016/j.ctim.2019.102208. https://www.ncbi.nlm.nih.gov/pubmed/31780012
- Aydin Yildirim T, Kitis Y. The Effect of Aromatherapy Application on Cognitive Functions and Daytime Sleepiness in Older Adults Living in a Nursing Home. Holistic nursing practice. Mar/Apr 2020;34(2):83-90. doi:10.1097/HNP.0000000000000371. https://www.ncbi.nlm.nih.gov/pubmed/32049695
- Lee HW, Ang L, Choi J, Lee MS. Aromatherapy for Managing Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Trials. J Altern Complement Med. Oct 2021;27(10):813-823. doi:10.1089/acm.2020.0315. https://www.ncbi.nlm.nih.gov/pubmed/34242093
- Roozbeh N, Ghazanfarpour M, Khadivzadeh T, Kargarfard L, Dizavandi FR, Shariati K. Effect of Lavender on Sleep, Sexual Desire, Vasomotor, Psychological and Physical Symptom among Menopausal and Elderly Women: A Systematic Review. Journal of menopausal medicine. Aug 2019;25(2):88-93. doi:10.6118/jmm.18158. https://www.ncbi.nlm.nih.gov/pubmed/31497578
- Zhang Y, Xiao A, Zheng T, Xiao H, Huang R. The Relationship between Sleeping Position and Sleep Quality: A Flexible Sensor-Based Study. Sensors (Basel, Switzerland). Aug 19 2022;22(16)doi:10.3390/s22166220. https://www.ncbi.nlm.nih.gov/pubmed/36015983
- Levendowski DJ, Gamaldo C, St Louis EK, et al. Head Position During Sleep: Potential Implications for Patients with Neurodegenerative Disease. J Alzheimers Dis. 2019;67(2):631-638. doi:10.3233/JAD-180697. https://www.ncbi.nlm.nih.gov/pubmed/30614805
- Gnarra O, Calvello C, Schirinzi T, et al. Exploring the Association Linking Head Position and Sleep Architecture to Motor Impairment in Parkinson's Disease: An Exploratory Study. J Pers Med . Nov 10 2023;13(11)doi:10.3390/jpm13111591. https://www.ncbi.nlm.nih.gov/pubmed/38003906
- Dijkstra F, Reyn N, de Bruyn B, et al. REM sleep without atonia and nocturnal body position in prediagnostic Parkinson's disease. Sleep Med . Aug 2021;84:308-316. doi:10.1016/j.sleep.2021.06.011. https://www.ncbi.nlm.nih.gov/pubmed/34217921
- Sommerauer M, Werth E, Poryazova R, Gavrilov YV, Hauser S, Valko PO. Bound to supine sleep: Parkinson's disease and the impact of nocturnal immobility. Parkinsonism Relat Disord. Oct 2015;21(10):1269-72. doi:10.1016/j.parkreldis.2015.08.010. https://www.ncbi.nlm.nih.gov/pubmed/26299159
- Ravesloot MJL, White D, Heinzer R, Oksenberg A, Pepin JL. Efficacy of the New Generation of Devices for Positional Therapy for Patients With Positional Obstructive Sleep Apnea: A Systematic Review of the Literature and Meta-Analysis. J Clin Sleep Med. Jun 15 2017;13(6):813-824. doi:10.5664/jcsm.6622. https://www.ncbi.nlm.nih.gov/pubmed/28212691
- Huang Z, Lobbezoo F, Vanhommerig JW, et al. Effects of demographic and sleep-related factors on snoring sound parameters. Sleep Med . Apr 2023;104:3-10. doi:10.1016/j.sleep.2023.02.012. https://www.ncbi.nlm.nih.gov/pubmed/36857868
- Srijithesh PR, Aghoram R, Goel A, Dhanya J. Positional therapy for obstructive sleep apnoea. Cochrane Database Syst Rev. May 1 2019;5(5):CD010990. doi:10.1002/14651858.CD010990.pub2. https://www.ncbi.nlm.nih.gov/pubmed/31041813
- Benoist LBL, Vonk PE, de Vries N, Janssen H, Verbraecken J. New-generation positional therapy in patients with positional central sleep apnea. Eur Arch Otorhinolaryngol. Sep 2019;276(9):2611-2619. doi:10.1007/s00405-019-05545-y. https://www.ncbi.nlm.nih.gov/pubmed/31302742
- Dong J, Sun H, Zhang H, Guo R. The effect of head rotation on OSA is associated with disease severity: a cross-sectional study. Eur Arch Otorhinolaryngol . Jul 2023;280(7):3279-3285. doi:10.1007/s00405-023-07860-x. https://www.ncbi.nlm.nih.gov/pubmed/36738327
- Cazan D, Mehrmann U, Wenzel A, Maurer JT. The effect on snoring of using a pillow to change the head position. Sleep Breath. Sep 2017;21(3):615-621. doi:10.1007/s11325-017-1461-1. https://www.ncbi.nlm.nih.gov/pubmed/28127672
- Foster RG. Sleep, circadian rhythms and health. Interface Focus . Jun 6 2020;10(3):20190098. doi:10.1098/rsfs.2019.0098. https://www.ncbi.nlm.nih.gov/pubmed/32382406
- Ruben MD, Hogenesch JB, Smith DF. Sleep and Circadian Medicine: Time of Day in the Neurologic Clinic. Neurol Clin. Aug 2019;37(3):615-629. doi:10.1016/j.ncl.2019.03.004. https://www.ncbi.nlm.nih.gov/pubmed/31256793
- Meyer N, Harvey AG, Lockley SW, Dijk DJ. Circadian rhythms and disorders of the timing of sleep. Lancet. Sep 24 2022;400(10357):1061-1078. doi:10.1016/S0140-6736(22)00877-7. https://www.ncbi.nlm.nih.gov/pubmed/36115370
- Khan S, Duan P, Yao L, Hou H. Shiftwork-Mediated Disruptions of Circadian Rhythms and Sleep Homeostasis Cause Serious Health Problems. Int J Genomics. 2018;2018:8576890. doi:10.1155/2018/8576890. https://www.ncbi.nlm.nih.gov/pubmed/29607311
- James SM, Honn KA, Gaddameedhi S, Van Dongen HPA. Shift Work: Disrupted Circadian Rhythms and Sleep-Implications for Health and Well-Being. Curr Sleep Med Rep. Jun 2017;3(2):104-112. doi:10.1007/s40675-017-0071-6. https://www.ncbi.nlm.nih.gov/pubmed/29057204
- Prather AA, Carroll JE. Associations between sleep duration, shift work, and infectious illness in the United States: Data from the National Health Interview Survey. Sleep health. Oct 2021;7(5):638-643. doi:10.1016/j.sleh.2021.05.004. https://www.ncbi.nlm.nih.gov/pubmed/34193397
- Vitale E, Lupo R, Artioli G, et al. How shift work influences anxiety, depression, stress and insomnia conditions in Italian nurses: an exploratory study. Acta bio-medica : Atenei Parmensis. Apr 24 2023;94(2):e2023102. doi:10.23750/abm.v94i2.14230. https://www.ncbi.nlm.nih.gov/pubmed/37092618
- Montaruli A, Castelli L, Mule A, et al. Biological Rhythm and Chronotype: New Perspectives in Health. Biomolecules. Mar 24 2021;11(4)doi:10.3390/biom11040487. https://www.ncbi.nlm.nih.gov/pubmed/33804974
- Chellappa SL. Individual differences in light sensitivity affect sleep and circadian rhythms. Sleep. Feb 12 2021;44(2)doi:10.1093/sleep/zsaa214. https://www.ncbi.nlm.nih.gov/pubmed/33049062
- Kennaway DJ. The dim light melatonin onset across ages, methodologies, and sex and its relationship with morningness/eveningness. Sleep. May 10 2023;46(5)doi:10.1093/sleep/zsad033. https://www.ncbi.nlm.nih.gov/pubmed/36799668
- Zou H, Zhou H, Yan R, Yao Z, Lu Q. Chronotype, circadian rhythm, and psychiatric disorders: Recent evidence and potential mechanisms. Front Neurosci . 2022;16:811771. doi:10.3389/fnins.2022.811771. https://www.ncbi.nlm.nih.gov/pubmed/36033630
- Lee Y, Field JM, Sehgal A. Circadian Rhythms, Disease and Chronotherapy. J Biol Rhythms. Dec 2021;36(6):503-531. doi:10.1177/07487304211044301. https://www.ncbi.nlm.nih.gov/pubmed/34547953
- Faulkner SM, Bee PE, Meyer N, Dijk DJ, Drake RJ. Light therapies to improve sleep in intrinsic circadian rhythm sleep disorders and neuro-psychiatric illness: A systematic review and meta-analysis. Sleep Med Rev . Aug 2019;46:108-123. doi:10.1016/j.smrv.2019.04.012. https://www.ncbi.nlm.nih.gov/pubmed/31108433
- D'Agostino A, Ferrara P, Terzoni S, et al. Efficacy of Triple Chronotherapy in unipolar and bipolar depression: A systematic review of the available evidence. J Affect Disord. Nov 1 2020;276:297-304. doi:10.1016/j.jad.2020.07.026. https://www.ncbi.nlm.nih.gov/pubmed/32697712
- Li D, Fang P, Liu H, et al. The Clinical Effect of Blue Light Therapy on Patients with Delayed Sleep-Wake Phase Disorder. Nature and science of sleep . 2022;14:75-82. doi:10.2147/NSS.S344616. https://www.ncbi.nlm.nih.gov/pubmed/35082544
- Mantua J, Spencer RMC. Exploring the nap paradox: are mid-day sleep bouts a friend or foe? Sleep Med. Sep 2017;37:88-97. doi:10.1016/j.sleep.2017.01.019. https://www.ncbi.nlm.nih.gov/pubmed/28899546
- Brooks A, Lack L. A brief afternoon nap following nocturnal sleep restriction: which nap duration is most recuperative? Sleep. Jun 2006;29(6):831-40. doi:10.1093/sleep/29.6.831. https://www.ncbi.nlm.nih.gov/pubmed/16796222
- Hilditch CJ, McHill AW. Sleep inertia: current insights. Nature and science of sleep . 2019;11:155-165. doi:10.2147/NSS.S188911. https://www.ncbi.nlm.nih.gov/pubmed/31692489
- Mattingly SM, Martinez G, Young J, Cain MK, Striegel A. Snoozing: an examination of a common method of waking. Sleep. Oct 10 2022;45(10)doi:10.1093/sleep/zsac184. https://www.ncbi.nlm.nih.gov/pubmed/35951011
- Sundelin T, Landry S, Axelsson J. Is snoozing losing? Why intermittent morning alarms are used and how they affect sleep, cognition, cortisol, and mood. J Sleep Res. May 2024;33(3):e14054. doi:10.1111/jsr.14054. https://www.ncbi.nlm.nih.gov/pubmed/37849039
- Ogawa K, Kaizuma-Ueyama E, Hayashi M. Effects of using a snooze alarm on sleep inertia after morning awakening. Journal of physiological anthropology . Dec 31 2022;41(1):43. doi:10.1186/s40101-022-00317-w. https://www.ncbi.nlm.nih.gov/pubmed/36587230
- McFarlane SJ, Garcia JE, Verhagen DS, Dyer AG. Alarm Tones, Voice Warnings, and Musical Treatments: A Systematic Review of Auditory Countermeasures for Sleep Inertia in Abrupt and Casual Awakenings. Clocks Sleep . Oct 20 2020;2(4):416-433. doi:10.3390/clockssleep2040031. https://www.ncbi.nlm.nih.gov/pubmed/33118526
- Miller DJ, Sargent C, Roach GD. A Validation of Six Wearable Devices for Estimating Sleep, Heart Rate and Heart Rate Variability in Healthy Adults. Sensors (Basel, Switzerland). Aug 22 2022;22(16)doi:10.3390/s22166317. https://www.ncbi.nlm.nih.gov/pubmed/36016077
- OuraRing. News: Oura Ring is Now FSA and HSA Eligible. Available at https://ouraring.com/blog/oura-ring-fsa-hsa/ Published 09/07/2023. Accessed 10/02/2023. 2023;
- HSAStore. Fitness Tracker: HSA Eligibility. Available at https://hsastore.com/hsa-eligibility-list/f/fitness-tracker Accessed 10/02/2023. 2023;
- Zhai H, Yan Y, He S, Zhao P, Zhang B. Evaluation of the Accuracy of Contactless Consumer Sleep-Tracking Devices Application in Human Experiment: A Systematic Review and Meta-Analysis. Sensors (Basel, Switzerland) . May 17 2023;23(10)doi:10.3390/s23104842. https://www.ncbi.nlm.nih.gov/pubmed/37430756
- NSF. National Sleep Foundation. SleepTech Award. Available at https://www.thensf.org/sleeptech-award/ Accessed 10/03/2023. 2022;
- AYO. AYO. Circadian Health for Everyone. Available at https://goayo.com/our-science-light-therapy/ Accessed 10/03/2023. 2023;
- Kokoon. Kokoon. How it Works. Available at https://kokoon.io/pages/how-it-works Accessed 10/03/2023. 2023;
- Fuentes B, Kennedy K, Killgore W, Wills C, Grandner M. 0010 Bed Sharing Versus Sleeping Alone Associated with Sleep Health and Mental Health. Sleep. 2022;45(Supplement_1):A4-A4. doi:10.1093/sleep/zsac079.009. https://doi.org/10.1093/sleep/zsac079.009
- Drews HJ, Wallot S, Brysch P, et al. Bed-Sharing in Couples Is Associated With Increased and Stabilized REM Sleep and Sleep-Stage Synchronization. Front Psychiatry. 2020;11:583. doi:10.3389/fpsyt.2020.00583. https://www.ncbi.nlm.nih.gov/pubmed/32670111
- Richter K, Adam S, Geiss L, Peter L, Niklewski G. Two in a bed: The influence of couple sleeping and chronotypes on relationship and sleep. An overview. Chronobiol Int. 2016;33(10):1464-1472. doi:10.1080/07420528.2016.1220388. https://www.ncbi.nlm.nih.gov/pubmed/27624285