Life Extension Magazine®
Osteoporosis has long been viewed as a disease that primarily affects women, turning their bones weak and prone to fractures as they age.
But men are at a far higher risk of osteoporosis than most realize. About one-third of all hip fractures worldwide occur in men.1
And while women do get osteoporosis more frequently, fractures in men result in more severe, and deadly complications.2-4
The rate of bone loss in osteoporosis is closely associated with increased mortality.5-8
And all men can strengthen bones and help prevent fractures with a few simple measures, including increased physical activity, weight-bearing exercises, resistance training, and ensuring proper intake of nutrients including magnesium, calcium, vitamin D, vitamin K, and more.
Together, these actions can help maintain healthy bones well into advanced age.
Osteoporosis in Men
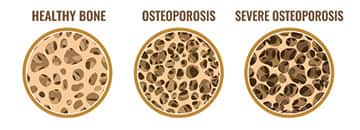
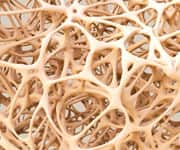
Healthy bone is constantly being remodeled. This means that old bone is broken down and new bone is formed.
For people with osteoporosis, bone loss outweighs bone growth. The result is low bone mass, deterioration of bone tissue, and bone fragility that leads to increased fracture risk.9,10
Osteoporosis usually produces no symptoms until a fracture occurs,2,11-13 so it remains underdiagnosed and undertreated. Many men, in particular, believe osteoporosis affects mostly aging women and ignore their own risks.14
But rates in men are striking:
-
Up to 1/3 of all hip fractures worldwide occur in men.1
-
Half of male hip fractures occur before the age of 80.1,15
Hip fractures are the most serious of all broken bones resulting from osteoporosis.2
In a study in men aged 60 and over, the mortality rate at one year from hip fractures was 37.5%,3 while another study found that men are more than twice as likely as women to die from infection during the first two years after a hip fracture.4
Fractures of the spinal vertebrae are much harder to detect than hip fractures. They may cause little pain at first, but can gradually lead to severe discomfort and risk of serious spinal cord injury.2,16
WHAT YOU NEED TO KNOW
Building and Protecting Strong Bones
-
Osteoporosis is no longer thought of as a disease that just affects older women. About one-third of all hip fractures worldwide occur in men.
-
Men have a higher death rate from hip fractures than women, and higher rates of bone loss are associated with higher mortality.
-
All men can benefit from ensuring adequate intake of vitamins and minerals that build up bone strength and help minimize risk of fracture, including calcium, vitamin D3, vitamin K, magnesium, manganese, zinc, silicon, and boron.
-
The nutrients curcumin and PQQ also play important roles in reducing the oxidative stress and inflammation that contribute to bone loss.
Assessing Fracture Risk

Osteoporosis in men usually results from a combination of risk factors, rather than from a single cause (like menopause in women).2
The most frequent causes of osteoporosis in men are alcohol abuse, excessive use of corticosteroids (medications often used to treat inflammatory disorders), and low testosterone and estrogen from aging, or from androgen-deprivation therapy for prostate cancer.2
Once osteoporosis has developed, many factors raise the risk of bone fractures in men, including:1,2,9,12
- Increasing age,
- Low body mass index,
- A history of fragility fractures in the individual or a parent,
- Low testosterone and estrogen,
- Prolonged immobilization or inactivity,
- High alcohol intake,
- Smoking,
- Glucocorticoid treatment,
- Type I diabetes,
- Rheumatoid arthritis,
- Thyroid disorders, and
- Chemotherapy treatment for cancer.
Weight-bearing and resistance exercises help build strong bones.17 And there are a variety of nutrients that can help slow bone loss and prevent fractures.
Nutrients to Promote Bone Strength

The standard nutritional “building blocks” of bone are calcium and vitamin D3.18
Calcium provides the bulk of the mineral content of bones, and vitamin D promotes calcium uptake from the gut.
But bones aren’t simple structures that can be built and left alone.
They’re dynamic, living tissue, with all the vulnerabilities to damage as any other tissue. It’s now recognized that healthy bones require additional nutritional support.
-
Magnesium regulates calcium movement into and between bone cells, increasing bone mineral density.19
-
Zinc stimulates new bone formation and helps calcium consolidate in bone.20
-
Manganese functions as an essential cofactor (helper molecule) for enzymes that promote the growth of bone and prevent damaging oxidative stress.21
-
Silicon improves the quality of bone matrix (the non-mineral part of bone composed of collagen and other proteins) and facilitates the bone-building process known as mineralization.22
-
Boron regulates the proper metabolism of calcium and other bone-forming minerals and influences the metabolism of vitamin D.23-25
-
Vitamin K is essential for activating a bone hormone (osteocalcin) needed to maintain bone strength.26,27 Low vitamin K status is associated with decreased bone density and increased fracture risk.28
New evidence is also emerging for two other compounds that support bone health.
1. Curcumin, an extract of the turmeric plant, has powerful anti-inflammatory properties. Chronic systemic inflammation is now being recognized as a contributor to osteoporosis risk.29,30
Newer studies have found that curcumin acts in multiple ways to increase bone mineral density and boost resistance to fractures.31-35 In one human study, curcumin in combination with calcium added to the effects of a prescription osteoporosis drug, alendronate.34
2. PQQ (pyrroloquinoline quinone) is a vitamin-like nutrient with anti-aging properties related to its ability to help mitochondria (the “powerhouses” of the cells) use energy more efficiently.36
Studies of PQQ in osteoporosis-prone mice show that it enhances the activity of bone-forming osteoblast cells while reducing the activity of bone-destroying osteoclast cells, resulting in increased bone mass and density.36-39
Ensuring adequate daily intake of all these nutrients can minimize the risk of developing osteoporosis and related fractures.
Summary

Osteoporosis is a progressive loss of bone density and strength, leading to sharply raised risk of fractures.
It was once thought mostly to affect older women. But about one-third of all hip fractures worldwide occur in men.
And because of the high osteoporosis risk, all men should regularly exercise to strengthen their bones, and should ensure they are getting the nutrients required to build and maintain strong bones.
Those include calcium, vitamin K, and vitamin D3, along with the minerals magnesium, manganese, zinc, silicon, and boron.
Further bone support can be obtained from curcumin and PQQ, which fight inflammation, improve bone cell energy use, and produce stronger bones.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Herrera A, Lobo-Escolar A, Mateo J, et al. Male osteoporosis: A review. World J Orthop. 2012 Dec 18;3(12):223-34.
- Giusti A, Bianchi G. Male osteoporosis. Reumatismo. 2014 Jul 28;66(2):136-43.
- Jiang HX, Majumdar SR, Dick DA, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005 Mar;20(3):494-500.
- Wehren LE, Hawkes WG, Orwig DL, et al. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003 Dec;18(12):2231-7.
- Lee P, Ng C, Slattery A, et al. Preadmission Bisphosphonate and Mortality in Critically Ill Patients. J Clin Endocrinol Metab. 2016 May;101(5):1945-53.
- Lenchik L, Register TC, Russell GB, et al. Volumetric bone mineral density of the spine predicts mortality in African-American men with type 2 diabetes. Osteoporos Int. 2018 Sep;29(9):2049-57.
- Masunari N, Fujiwara S, Kasagi F, et al. Height loss starting in middle age predicts increased mortality in the elderly. J Bone Miner Res. 2012 Jan;27(1):138-45.
- Bliuc D, Tran T, van Geel T, et al. Reduced Bone Loss Is Associated With Reduced Mortality Risk in Subjects Exposed to Nitrogen Bisphosphonates: A Mediation Analysis. J Bone Miner Res. 2019 Nov;34(11):2001-11.
- Pisani P, Renna MD, Conversano F, et al. Major osteoporotic fragility fractures: Risk factor updates and societal impact. World J Orthop. 2016 Mar 18;7(3):171-81.
- Kanis JA, McCloskey EV, Johansson H, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013 Jan;24(1):23-57.
- Nih Consensus Development Panel on Osteoporosis Prevention D, Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001 Feb 14;285(6):785-95.
- Drake MT, Khosla S. Male osteoporosis. Endocrinol Metab Clin North Am. 2012 Sep;41(3):629-41.
- Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993 Jun;94(6):646-50.
- Dy CJ, Lamont LE, Ton QV, et al. Sex and gender considerations in male patients with osteoporosis. Clin Orthop Relat Res. 2011 Jul;469(7):1906-12.
- Chang KP, Center JR, Nguyen TV, et al. Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res. 2004 Apr;19(4):532-6.
- Khosla S, Amin S, Orwoll E. Osteoporosis in men. Endocr Rev. 2008 Jun;29(4):441-64.
- Available at: https://www.bones.nih.gov/health-info/bone/bone-health/exercise/exercise-your-bone-health. Accessed January 27, 2020.
- Moyer VA, Force* USPST. Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013 May 7;158(9):691-6.
- Mammoli F, Castiglioni S, Parenti S, et al. Magnesium Is a Key Regulator of the Balance between Osteoclast and Osteoblast Differentiation in the Presence of Vitamin D(3). Int J Mol Sci. 2019 Jan 17;20(2).
- Yamaguchi M. Role of nutritional zinc in the prevention of osteoporosis. Mol Cell Biochem. 2010 May;338(1-2):241-54.
- Data on file.
- Price CT, Koval KJ, Langford JR. Silicon: a review of its potential role in the prevention and treatment of postmenopausal osteoporosis. Int J Endocrinol. 2013;2013:316783.
- Devirian TA, Volpe SL. The physiological effects of dietary boron. Crit Rev Food Sci Nutr. 2003;43(2):219-31.
- Naghii MR, Samman S. The role of boron in nutrition and metabolism. Prog Food Nutr Sci. 1993 Oct-Dec;17(4):331-49.
- Nielsen FH. Studies on the relationship between boron and magnesium which possibly affects the formation and maintenance of bones. Magnes Trace Elem. 1990;9(2):61-9.
- Fujita Y, Iki M, Tamaki J, et al. Association between vitamin K intake from fermented soybeans, natto, and bone mineral density in elderly Japanese men: the Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) study. Osteoporos Int. 2012 Feb;23(2):705-14.
- Bullo M, Estruch R, Salas-Salvado J. Dietary vitamin K intake is associated with bone quantitative ultrasound measurements but not with bone peripheral biochemical markers in elderly men and women. Bone. 2011 Jun 1;48(6):1313-8.
- Rodriguez-Olleros Rodriguez C, Diaz Curiel M. Vitamin K and Bone Health: A Review on the Effects of Vitamin K Deficiency and Supplementation and the Effect of Non-Vitamin K Antagonist Oral Anticoagulants on Different Bone Parameters. J Osteoporos. 2019;2019:2069176.
- Al-Daghri NM, Aziz I, Yakout S, et al. Inflammation as a contributing factor among postmenopausal Saudi women with osteoporosis. Medicine (Baltimore). 2017 Jan;96(4):e5780.
- Fang H, Zhang H, Wang Z, et al. Systemic immune-inflammation index acts as a novel diagnostic biomarker for postmenopausal osteoporosis and could predict the risk of osteoporotic fracture. J Clin Lab Anal. 2020 Jan;34(1):e23016.
- Chen Z, Xue J, Shen T, et al. Curcumin alleviates glucocorticoid-induced osteoporosis by protecting osteoblasts from apoptosis in vivo and in vitro. Clin Exp Pharmacol Physiol. 2016 Feb;43(2):268-76.
- Chen Z, Xue J, Shen T, et al. Curcumin alleviates glucocorticoid-induced osteoporosis through the regulation of the Wnt signaling pathway. Int J Mol Med. 2016 Feb;37(2):329-38.
- French DL, Muir JM, Webber CE. The ovariectomized, mature rat model of postmenopausal osteoporosis: an assessment of the bone sparing effects of curcumin. Phytomedicine. 2008 Dec;15(12):1069-78.
- Khanizadeh F, Rahmani A, Asadollahi K, et al. Combination therapy of curcumin and alendronate modulates bone turnover markers and enhances bone mineral density in postmenopausal women with osteoporosis. Arch Endocrinol Metab. 2018 Aug;62(4):438-45.
- Li G, Bu J, Zhu Y, et al. Curcumin improves bone microarchitecture in glucocorticoid-induced secondary osteoporosis mice through the activation of microRNA-365 via regulating MMP-9. Int J Clin Exp Pathol. 2015;8(12):15684-95.
- Huang Y, Chen N, Miao D. Effect and mechanism of pyrroloquinoline quinone on anti-osteoporosis in Bmi-1 knockout mice-Anti-oxidant effect of pyrroloquinoline quinone. Am J Transl Res. 2017;9(10):4361-74.
- Geng Q, Gao H, Yang R, et al. Pyrroloquinoline Quinone Prevents Estrogen Deficiency-Induced Osteoporosis by Inhibiting Oxidative Stress and Osteocyte Senescence. Int J Biol Sci. 2019;15(1):58-68.
- Wen H, He Y, Zhang K, et al. Mini-review:Functions and Action Mechanisms of PQQ in Osteoporosis and Neuro Injury. Curr Stem Cell Res Ther. 2018 Dec 10.
- Wu X, Li J, Zhang H, et al. Pyrroloquinoline quinone prevents testosterone deficiency-induced osteoporosis by stimulating osteoblastic bone formation and inhibiting osteoclastic bone resorption. Am J Transl Res. 2017;9(3):1230-42.

