Life Extension Magazine®
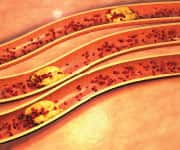
Most people are aware that a buildup of plaque in coronary arteries leads to heart disease, the cause of more American deaths than any other ailment.
But few know that not all arterial plaque is the same. There is hard (calcified) plaque and soft (noncalcified) plaque.
Although both pose a risk, the soft kind is a ticking time bomb. When soft plaque suddenly breaks loose, it can trigger a clot blockage large enough to cause acute heart attack or stroke.
Because soft plaque is unstable and causes no symptoms until it pops without warning, someone with atherosclerosis may feel fine, have a normal EKG, and pass a stress test—and later that same day have a plaque rupture, resulting in sudden death.
Researchers have identified two natural compounds that target arterial plaque and atherosclerosis. Together, they have been shown to boost stability of deadly soft plaque to help prevent a plaque rupture, while also slowing and even regressing the accumulation of soft and hard arterial plaque.1
Arterial Plaque—The Hidden Killer

Rupture-prone arterial plaques are more common than people realize.
In one cadaver study, advanced lesions, defined as rupture plaque or at least one vulnerable plaque were present in 100% of the hearts examined—regardless of the individuals’ cause of death.2,3
Arterial damage can initiate in childhood and slowly progress with normal aging.4 Atherosclerosis—from the Greek words for “hard paste”—is an inflammatory condition in which the interior of the arteries becomes stiff, clogged, damaged, and dysfunctional.5-7
When the delicate lining of the inner arteries becomes damaged, low-density lipoprotein (LDL) and fibrinogen adhere and begin to trap other components.
As it builds up, plaque may cause the arterial wall to remodel and ultimately internally rupture, allowing a blood clot to form.8 Arterial clots (thrombosis) can block local blood flow completely, or they may break free and cause dangerous blockages elsewhere.
Plaque Stability: A Key Factor in Preventing Fatalities
When seeking to reduce atherosclerotic risk, there is more to it than just prevention of plaque formation, as most of the danger posed by plaque occurs when it becomes unstable.
Early in this process, plaques are soft on the inside, making them vulnerable to rupture, like a kernel of corn being heated until it explodes into much larger popcorn. Fortunately, the surfaces of soft plaques are covered with hard fibrous caps that face the blood flow.
As long as these plaques remain thick, they are stable, meaning they are firm enough not to pose a major risk of rupturing.2,9 Over time, however, this cap begins to thin and weaken, making the plaque more vulnerable to rupturing. The result is a deadlier, much more unstable, softer type of plaque that may lead to ischemic stroke or heart attack.
The effects of atherosclerosis vary, depending on which arteries in the body narrow and become clogged with plaque. If the arteries that bring oxygen-rich blood to the heart are affected, the result can be coronary artery disease, chest pain, or heart attack. If the arteries to the brain are affected, the result can be a transient ischemic attack (TIA) or a stroke. If the arteries in the arms or legs are affected, peripheral artery disease can occur. And at any point in the body, a deadly bulge in the artery wall—an aneurysm—can develop.
This is why scientists have long sought a way to safely lower acute cardiovascular risk not only by reducing plaque but by stabilizing soft plaques.
The December 2016 issue of the journal Minerva Cardioangiologica published a controlled clinical study demonstrating the plaque stabilizing effects of a dual-extract plant formula.
This study showed a standardized extract from the French maritime pine combined with an extract of the Centella asiatica plant stabilized soft plaques, boosting the odds that they will stay put and not suddenly rupture. These two nutrients also demonstrated reversal of the number and size of arterial plaque deposits that progress to atherosclerosis.1
This 2016 study confirmed earlier evidence demonstrating the arterial protective properties of these two nutrients.
Before examining this compelling clinical evidence, let’s examine each compound separately.
What You Need to Know
 |
How to Prevent a Deadly Plaque Rupture
- While hard plaque in the arteries limits blood flow, soft or noncalcified plaque can suddenly break loose and cause a blood clot large enough to cause a deadly heart attack or stroke.
- The natural compound Centella asiatica stabilizes the hard, thick cap on atherosclerotic plaques, which slashes the risk of a plaque rupture. Standardized extract from French maritime pine slows progression of atherosclerotic plaques.
- Clinical research demonstrates that, when combined, these two supplements reduce the size, number, and instability of deadly soft plaques, while slowing and even regressing plaque accumulation.
Centella Asiatica Stabilizes Soft Plaque
Also known as gotu kola, Centella asiatica contains triterpenoid compounds that help stabilize soft plaque by improving the synthesis of collagen,10-13 a component of the thick caps that hold soft plaque in place.10,14 This Asian aquatic plant also helps stop the progression of plaque buildup by reducing the adhesion of monocytes, immune system cells that promote atherosclerosis.15
In a previous human study, participants with high-risk (soft) plaque took 60 mg of an extract of Centella asiatica three times daily. After 12 months, their carotid-artery plaque was denser (harder) by an average of 30%.14
Phase two of this same study used the same dose but in a randomized, placebo-controlled trial. Carotid-artery plaque stability significantly improved. MRI scans showed reduced blood flow to the brain in 17% of controls but only in 7% of the Centella asiatica group. And supplemented subjects experienced 41% fewer cardiovascular events.14
A similar placebo-controlled study of individuals with high-risk (soft) plaque in their femoral (main leg) arteries found that 60 mg of an extract of Centella asiatica three times daily produced a 63% harder plaque—indicating a lower rupture risk—in just 12 months. Critically, plaque size increased 23% in controls while supplemented patients showed zero plaque-size increase.10
Let’s now examine standardized extract from the French maritime pine, a compound that reduces atherosclerosis progression.
French Maritime Pine Extract Inhibits Plaque Accumulation
Standardized extract from French maritime pine contains procyanidins and phenolic acids16,17 shown to slow atherosclerosis.18 It achieves this by reducing production of fat cells and inflammatory signaling molecules that contribute to plaque formation.19,20
Lab studies show that standardized extract from French maritime pine improves arterial endothelial function by stimulating an enzyme (eNOS) that produces nitric oxide, the signaling molecule that maintains arterial elasticity. This increase in nitric oxide not only improves blood flow but also decreases platelet aggregation and stickiness to vessel walls, reducing the risks of blood clots and enlarging plaques.21
A placebo-controlled human trial demonstrated that 200 mg of standardized extract from French maritime pine daily for eight weeks improved endothelial function in coronary artery disease patients, helping to limit atherosclerosis progression. Flow-mediated dilation—a measure of how much arteries dilate in response to blood-flow changes—was improved 32% in the supplemented group contrasting with no significant change in the controls. Also, only supplemented subjects experienced a 7% drop in isoprostanes, a marker of how much oxidized fat is present and overall oxidative stress.22
Scientists then studied individuals with only borderline issues with blood pressure, blood lipids, and blood sugar, with no obvious atherosclerotic changes in their blood vessels and no existing coronary artery disease—reflecting the situation of most people that have not developed any clinically relevant disease but had definitive risk factors, making them ideal candidates for a preventive intervention. All 93 volunteers continued any medical treatment for symptoms, but half also took 150 mg of standardized extract from French maritime pine daily. Flow-mediated dilation in supplemented subjects improved 66%—after only 12 weeks.23
Scientists then produced a formulation combining standardized extracts from French maritime pine and Centella asiatica, leading to compelling clinical trials.
Dual-Extract Formulation Targets Atherosclerosis

One clinical trial enlisted individuals ages 45 to 60 who appeared healthy with no cardiovascular risk factors or symptoms and with plaques that did not narrow their arteries more than 50% (class IV). Each group was assigned a different supplement regimen daily along with lifestyle, diet, education, and exercise recommendations. Ultrasound was used to measure plaques that had progressed from class IV to class V (blocking over 50% of an artery). After 30 months, the percentage of plaques progressing from class IV to V was:18
- 21.3% in controls, which followed only diet and lifestyle recommendations. (This was the worst performing group as it showed more than 20% had progressive arterial narrowing.)
- 16.6% with 100 mg aspirin or ticlopidine (an antiplatelet drug) for aspirin-intolerant subjects,
- 8.4% with 50 mg standardized extract from French maritime pine alone,
- 5.3% with 100 mg standardized extract from French maritime pine alone,
- 4.0% with 100 mg standardized extract from French maritime pine plus 100 mg aspirin (or ticlopidine), and
- 1.1% with 100 mg standardized extract from French maritime pine plus 100 mg extract of Centella asiatica. (This was best performing group as it showed less than 2% had progressive inner arterial narrowing.)
Plaque progression in volunteers taking both compounds was an impressive 95% lower than in controls.18
Next, subjects with advanced atherosclerosis—at least one arterial lesion considered class V—but without symptoms were assigned to the same dosages as previously. Class V involves an instance of over-50% blockage without symptoms, while class VI also involves symptoms such as numbness, tingling, pain, or other, more serious cerebral or lower-limb symptoms. After 42 months, the percentage with plaques progressing from class V to VI was:24
- 48% in controls (worst performers in this study),
- 21% with aspirin or ticlopidine,
- 11% with 100 mg standardized extract from French maritime pine plus aspirin,
- 10% with 100 mg standardized extract from French maritime pine alone, and
- 6.5% with 100 mg standardized extract from French maritime pine plus 100 mg extract of Centella asiatica (best performers in this study).
Compared to controls, the standardized extracts from the French maritime pine plus Centella asiatica group showed a 7.4-fold reduction in the risk of developing cardiovascular-disease symptoms—and a nearly four-fold reduced risk of being hospitalized for a full-blown cardiovascular event.24
Blood Test May Detect Presence of Soft Plaque
 |
Published data suggests an association between elevated high-sensitivity CRP and soft plaque burden.
A low-cost blood test called C-reactive protein can help identity those at risk for soft, rupture-prone arterial plaque.
Life Extension® long ago published data showing that people with low CRP blood levels (that often correspond to reduced chronic inflammation) have markedly lower rates of cancer and stroke.27,28
A high-sensitivity C-reactive protein (CRP) test is included in the Male and Female Blood Test Panels that many readers of this publication have performed annually.
These comprehensive blood tests can be ordered for just $199 during the annual Blood Test Super Sale that ends June 5, 2017.
To order these tests, call 1-800-208-3444 (24 hours) or log on to: LifeExtension.com/Sale
Latest Human Trial Results
The study published in December 2016 added to the clinical evidence demonstrating the compelling effects of this dual-nutrient formula in stabilizing soft arterial plaques—to help prevent a potentially lethal plaque rupture—and in blocking the progression of plaque accumulation in aging arteries.1
Scientists set out to evaluate the stability of carotid plaques, before and after three months of supplementation, in 50 symptom-free volunteers with arterial plaque stenosis of less than 50% (class IV), high oxidative stress, and with a mean age of 61.5 years.
Half of the patients were given 150 mg of standardized extract from French maritime pine along with 225 mg of an extract of Centella asiatica, daily for three months. They also received standard management care, as did the control group.1
Supplemented patients showed significant improvement on the plaque stability index compared to controls. They also experienced a substantial increase in the “white component” of their plaque based on ultrasound imaging, indicating improved plaque density and “a significant reduction in possible events.” Critically, their plaques were also decreased in length, height, and number. The scientists noted that free radicals in the supplemented group’s plasma were significantly reduced, indicating a decrease in oxidative stress. No supplement-related, adverse events were observed.
By contrast, there were no significant improvements in any of these endpoints for those receiving only standard plaque management.
The study concluded that these “…plant extracts could be a safe option for prevention of cardiovascular events for patients with carotid plaques.”1
The Risk of Arterial Plaque
 |
Years of elevated cholesterol, chronic inflammation, and other factors often result eventually in atherosclerosis—the thickening and narrowing of arteries that leads to coronary heart disease (heart attack), stroke, and peripheral vascular disease.8 Research in recent years has produced a vastly more sophisticated understanding of the processes leading up to devastating arterial blockage by plaque lesions.
The foundation of plaque lesions begin even before the teen years with the development of fatty streaks—regions of increased fat in the walls of arteries.8,25,26 Initially, the small damaged fatty-streak areas trigger a “healing” response—as if the streak areas were a wound—attracting inflammatory cells that ingest and store excess fats.21
Eventually, arterial plaque begins to take shape as a core of fats develops outside of inflammatory cells.8,26 These plaques become less stable over time, making them more vulnerable to rupture, which leads to heart attacks and strokes.
Whatever will slow the progression of early fatty deposits into complete plaque lesions is beneficial. Because soft plaques are unstable and can rupture, whatever can be done to stabilize these soft plaques makes the risk of a sudden catastrophic heart attack or stroke much less likely.
Summary
Not all arterial plaque is the same. Hard (calcified) plaque limits blood flow—but soft (noncalcified) plaque is a ticking time bomb that can suddenly break loose and trigger a clot large enough to cause a fatal heart attack or stroke.
Two natural compounds have been identified that target arterial plaque and atherosclerosis. Standardized extract from French maritime pine has been demonstrated to slow the progression of atherosclerotic plaques, while extracts of Centella asiatica have been found to preserve the hard, thick cap on atherosclerotic plaques—slashing the risk of a plaque rupture.
Clinical evidence now demonstrates that, taken together, these two supplements reduce the size, number, and instability of deadly soft plaques to help prevent plaque rupture—while also slowing and even regressing the accumulation of both soft and hard plaque.
If you have any questions on the scientific content of this article, please call a Life Extension® Wellness Specialist at 1-866-864-3027.
References
- Luzzi R, Belcaro G, Ippolito E. Carotid plaque stabilization induced by the supplement association Pycnogenol(R) and centella asiatica (Centellicum(R)). Minerva Cardioangiol. 2016;64(6):603-9.
- Cheruvu PK, Finn AV, Gardner C, et al. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries: a pathologic study. J Am Coll Cardiol. 2007;50(10):940-9.
- Kolodgie FD, Burke AP, Farb A, et al. The thin-cap fibroatheroma: a type of vulnerable plaque: the major precursor lesion to acute coronary syndromes. Curr Opin Cardiol. 2001;16(5):285-92.
- Osika W, Dangardt F, Gronros J, et al. Increasing peripheral artery intima thickness from childhood to seniority. Arterioscler Thromb Vasc Biol. 2007;27(3):671-6.
- Tuttolomondo A, Di Raimondo D, Pecoraro R, et al. Atherosclerosis as an inflammatory disease. Curr Pharm Des. 2012;18(28):4266-88.
- Available at: http://www.strokeassociation.org/STROKEORG/LifeAfterStroke/HealthyLivingAfterStroke/UnderstandingRiskyConditions/Atherosclerosis-and-Stroke_UCM_310426_Article.jsp. Accessed November 29, 2016.
- Libby P, Theroux P. Pathophysiology of coronary artery disease. Circulation. 2005;111(25):3481-8.
- Bentzon JF, Otsuka F, Virmani R, et al. Mechanisms of plaque formation and rupture. Circ Res. 2014;114(12):1852-66.
- Leskinen MJ, Kovanen PT, Lindstedt KA. Regulation of smooth muscle cell growth, function and death in vitro by activated mast cells--a potential mechanism for the weakening and rupture of atherosclerotic plaques. Biochem Pharmacol. 2003; 66(8):1493-8.
- Incandela L, Belcaro G, Nicolaides AN, et al. Modification of the echogenicity of femoral plaques after treatment with total triterpenic fraction of Centella asiatica: a prospective, randomized, placebo-controlled trial. Angiology. 2001;52 Suppl 2:S69-73.
- Incandela L, Cesarone MR, Cacchio M, et al. Total triterpenic fraction of Centella asiatica in chronic venous insufficiency and in high-perfusion microangiopathy. Angiology. 2001;52 Suppl 2:S9-13.
- James JT, Dubery IA. Pentacyclic triterpenoids from the medicinal herb, Centella asiatica (L.) Urban. Molecules. 2009;14(10):3922-41.
- Gohil KJ, Patel JA, Gajjar AK. Pharmacological Review on Centella asiatica: A Potential Herbal Cure-all. Indian J Pharm Sci. 2010;72(5):546-56.
- Cesarone MR, Belcaro G, Nicolaides AN, et al. Increase in echogenicity of echolucent carotid plaques after treatment with total triterpenic fraction of Centella asiatica: a prospective, placebo-controlled, randomized trial. Angiology. 2001;52 Suppl 2:S19-25.
- Ivanov V, Ivanova S, Kalinovsky T, et al. Plant-derived micronutrients suppress monocyte adhesion to cultured human aortic endothelial cell layer by modulating its extracellular matrix composition. J Cardiovasc Pharmacol. 2008;52(1):55-65.
- D’Andrea G. Pycnogenol: a blend of procyanidins with multifaceted therapeutic applications? Fitoterapia. 2010;81(7):724-36.
- Rohdewald P. A review of the French maritime pine bark extract (Pycnogenol), a herbal medication with a diverse clinical pharmacology. Int J Clin Pharmacol Ther. 2002;40(4):158-68.
- Belcaro G, Dugall M, Hosoi M, et al. Pycnogenol(R) and Centella Asiatica for asymptomatic atherosclerosis progression. Int Angiol. 2014;33(1):20-6.
- 9. Gu JQ, Ikuyama S, Wei P, et al. Pycnogenol, an extract from French maritime pine, suppresses Toll-like receptor 4-mediated expression of adipose differentiation-related protein in macrophages. Am J Physiol Endocrinol Metab. 2008;295(6):E1390-400.
- Luo H, Wang J, Qiao C, et al. Pycnogenol attenuates atherosclerosis by regulating lipid metabolism through the TLR4-NF-kappaB pathway. Exp Mol Med. 2015;47:e191.
- Fitzpatrick DF, Bing B, Rohdewald P. Endothelium-dependent vascular effects of Pycnogenol. J Cardiovasc Pharmacol. 1998;32(4):509-15.
- Enseleit F, Sudano I, Periat D, et al. Effects of Pycnogenol on endothelial function in patients with stable coronary artery disease: a double-blind, randomized, placebo-controlled, cross-over study. Eur Heart J. 2012;33(13):1589-97.
- Hu S, Belcaro G, Cornelli U, et al. Effects of Pycnogenol(R) on endothelial dysfunction in borderline hypertensive, hyperlipidemic, and hyperglycemic individuals: the borderline study. Int Angiol. 2015;34(1):43-52.
- Belcaro G, Ippolito E, Dugall M, et al. Pycnogenol(R) and Centella asiatica in the management of asymptomatic atherosclerosis progression. Int Angiol. 2015;34(2):150-7.
- Available at: http://my.clevelandclinic.org/services/heart/disorders/coronary-artery-disease/understandingcad. Accessed November 30, 2016.
- Sakakura K, Nakano M, Otsuka F, et al. Pathophysiology of atherosclerosis plaque progression. Heart Lung Circ. 2013;22(6):399-411.
- Available at: http://www.lifeextension.com/Magazine/2014/5/Testing-For-C-reactive-Protein-May-Save-Your-Life/Page-0. Accessed February 24, 2017.
- Available at: http://www.lifeextension.com/Magazine/2005/4/report_stroke/Page-02. Accessed February 24, 2017.

