Life Extension Magazine®
We recognize the medical establishment is agonizingly slow at grasping new concepts. They do wake up to scientific reality, however, when they smell an opportunity to earn tens of billions of dollars. Life Extension members were warned long ago about the dangers of excess C-reactive protein in the blood. C-reactive protein is a marker of inflammation. Chronic inflammation, as evidenced by high C-reactive protein blood levels, is a cause of atherosclerosis.1-3 Published studies indicate that elevated C-reactive protein may be a greater risk factor than high cholesterol in predicting heart attack and especially stroke risk.4-8 There are many natural methods to lower C-reactive protein. The pharmaceutical industry favors using statin drugs: an unnatural way to reduce C-reactive protein. While statin drugs are prescribed to lower LDL (low-density lipoprotein) and total cholesterol, statin drugs also reduce heart attack and stroke risk by suppressing C-reactive protein. A clinical study was sponsored by a pharmaceutical company to see if its patented statin drug (Crestor®) would reduce heart attack and stroke risk if given to people with moderate LDL levels, but excess C-reactive protein. The results revealed a 43% reduction in various types of vascular disease after less than two years.9 These data are impressive on the surface, but the study exposed a harsh reality that we at Life Extension have voiced alarming concern about for decades. As you will read, Crestor® significantly reduced heart attack-stroke incidence, but there were still a startling number of heart attacks and strokes in people whose LDL levels plummeted to extremely low levels. While this study may be used to aggressively promote Crestor®, it exposes the limitations of statin drugs in preventing heart disease and stroke. This study does help validate the multipronged vascular protection program that most Life Extension members already follow, especially the comprehensive blood tests members take to uncover hidden risk factors like C-reactive protein. We don’t agree that people should start using high-dose Crestor® when safer, lower-cost, and more comprehensive approaches exist right now. The Crestor® Study Subjects
Fat cells are a source of C-reactive protein production in the body.10,11 Corpulent people usually have C-reactive protein levels much higher than lean individuals. In order to find enough subjects with high C-reactive protein levels, participants in the Crestor® study were recruited who were significantly overweight with a median body mass index of about 28. Overweight is clinically defined as a body mass index of 25 and above. Despite having only modest LDL elevations (median about 108 mg/dL), this group of overweight individuals was at high risk for vascular disease, as about 41% already suffered from metabolic syndrome when the study commenced. Metabolic syndrome is a constellation of risk factors that sharply elevates one’s risk for contracting a lethal disorder. The median study subjects’ baseline C-reactive protein blood levels were 4.25 mg/L, a reading that placed them at greater risk for a host of age-related diseases including cancer, dementia, heart attack, and stroke. High-Dose Crestor® UsedCrestor® is the most potent statin drug, compared with milder statin drugs like pravastatin and simvastatin. The 20 mg daily dose of Crestor® used in this study is on the very high side for this particular drug. In fact, the dose of Crestor® used in this study was double the recommended starting dose. This raises concern about long-term side effects, though few were reported in this relatively short-term study. In lieu of this high-dose Crestor®, many people may find similar benefits taking 5-20 mg of simvastatin or 20-40 mg a day of pravastatin, plus natural agents to lower C-reactive protein. The monthly cost to take Crestor® (20 mg) is $105, whereas generic simvastatin (20 mg) costs only $6.91 a month and generic pravastatin (40 mg) only $11.40 a month. C-Reactive Protein Not Lowered EnoughDespite the very high dose of Crestor® used, median C-reactive protein levels fell only from 4.25 mg/L to 2.2 mg/L of blood. The optimal range for C-reactive protein is under 0.55 mg/L in men and under 1.5 mg/L in women.12 Crestor®, even at the relatively high dose used, fell far short of reducing C-reactive protein enough to completely eliminate this inflammatory marker as a vascular disease risk factor.
What this high dose of Crestor® did do is lower LDL from a baseline average of 108 to 55 mg/dL at the end of the study. Few statin drug studies have suppressed LDL this much. Please remember that LDL is not all bad. LDL is essential to transport cholesterol from the liver to cells that need it throughout the body. Without sufficient LDL, people will die. The problem is that no one yet knows for sure what truly optimal LDL levels are. You need enough LDL to ensure that sufficient cholesterol is delivered to the cell membranes, but not so much LDL that arterial occlusion manifests. We believe that the 43% reduction in risk of major cardiovascular events (including heart attack, stroke, unstable angina, arterial revascularization, and death from cardiovascular causes) observed in this study was a result of suppressing both LDL and C-reactive protein levels, along with other endothelial benefits that statin drugs possess (which can also be obtained by using natural approaches). We are concerned, however, about the long-term effects of using a potent dose of a drug like Crestor®, when safer and more natural strategies are available. Too Many Crestor® Patients Suffered “Major Cardiovascular Events”Pharmaceutical companies have promoted statin drugs as a virtually universal remedy to prevent heart attack. According to conventional guidelines, statin drugs are to be prescribed when LDL blood levels exceed 130 mg/dL.
We at Life Extension have long argued that LDL levels should be kept below 100 mg/dL in healthy people to optimally protect against atherosclerosis (and below 70 mg/dL in certain high-risk cardiac patients). The high dose of Crestor® used in this study pushed LDL down to a low of 55 mg/dL and it reduced C-reactive protein by 37%. The fact that a significant number of subjects taking Crestor® still suffered “major cardiovascular events” exposes the fallacy of relying only on statin drugs to maintain healthy arterial blood flow. To put this in mathematical perspective, this study showed that if 10,000 people were not treated with Crestor® for one year’s time, there would be 136 major cardiovascular events. Based on the elevated baseline blood C-reactive protein (4.2 mg/L), the fact that LDL was over 100 mg/dL, and that 41% of these subjects had metabolic syndrome, this number of 136 cardiac events per 10,000 study subjects makes sense if no interventions are done. This study showed that if 10,000 study subjects took high-dose Crestor® for one year, 59 major cardiovascular events would not occur (compared with 136 events that would occur if Crestor® was not taken). What will not be disclosed in drug advertising, however, is that more than half (77 out of 136) of major cardiovascular events would occur despite the use of high-dose Crestor®. In statistical terms, while Crestor® reduced the relative risk of major cardiovascular events by 43%, the majority (57%) of cardiovascular events in this high-risk study group study would still take place! What this means is that if you have cardiac risk factors and rely solely on a high-dose statin drug, you are still at significant risk of suffering a heart attack. In fact, 142 patients treated with high-dose Crestor® experienced a cardio-vascular event during this study. Why Crestor® Failed 142 Patients in This Study
There are at least 17 independent risk factors involved in the development of atherosclerosis and subsequent heart attack and stroke. Statin drugs do not come close to correcting all of these risk factors. Based on the findings from this Crestor® study, it is obvious that even when LDL (and total cholesterol) is reduced to extremely low levels, too many people still suffer a major cardiovascular event. We predict this study will eventually be used in national advertisements to tout Crestor® as a panacea. An analysis of the actual study findings, however, documents the critical need to correct all known cardiovascular risk factors (including elevated LDL, total cholesterol, and C-reactive protein). We are not vilifying the proper use of statin drugs. For many people with stubbornly high LDL and C-reactive protein levels, they represent an important weapon against arterial disease. Our emphasis is that statin drugs are not the only way to lower LDL and C-reactive protein, and they should not be relied on as the only approach to protect against atherosclerosis. Reducing C-Reactive Protein Often Requires a Multimodal ApproachLife Extension has reviewed thousands of C-reactive protein blood test results over the years. Our consistent observation is that overweight and obese individuals have stubbornly elevated C-reactive protein levels.13 Our findings were confirmed in a recent study that showed the following:14,15 Percent with Elevated C-Reactive Protein (>1 mg/dL)
These grim findings correlate well with the increased risks of cancer,16-18 stroke,8,19 heart attack,19-23 and dementia24 that occur as people accumulate excess body fat. In the Crestor® study, average C-reactive protein levels were 4.25 mg/L at baseline. Obese individuals can have C-reactive protein levels that are easily double this. The biological challenge in overweight people is to combat the excess C-reactive protein made directly by fat cells (adipocytes) and the C-reactive protein made in the liver in response to excess amounts of interleukin-6 expressed in abdominal fat that is dumped directly into the liver. Since obese and overweight individuals spew out C-reactive protein from their liver and fat cells, it is often challenging to bring this lethal inflammatory compound (C-reactive protein) into safe ranges. While we are impressed with the data from the Crestor® study showing the reduction in C-reactive protein and major cardiovascular events, our decade-long evaluation of C-reactive protein blood results prompts us to warn that it will require more than statin drugs to suppress the dangerously high C-reactive protein levels prevalent in so many individuals. The good news is that low-cost nutrients and hormones, along with dietary changes, can work as well as statins in reducing deadly C-reactive protein. Vitamin C Reduces C-Reactive ProteinRight after the media put Crestor® on the front pages, a study was published showing that 1,000 mg a day of vitamin C reduces C-reactive protein as well as some statin drugs.14 Needless to say, this vitamin C study received scant media coverage. In this University of California at Berkeley study, participants who received vitamin C and started out with C-reactive protein levels greater than 2.00 mg/L had 34% lower levels compared with the placebo group after only two months.14,15 This study was done based on previous findings that vitamin C supplements reduce elevated C-reactive protein. It would have been interesting to see if the addition of 1,000 mg a day of vitamin C would have reduced the number of “major cardiovascular events” that occurred in the Crestor® study. A Healthy Diet Significantly Reduces C-Reactive ProteinEating too much saturated fat or high-glycemic carbohydrates increases C-reactive protein.25,26 One study showed a 39% decrease in C-reactive protein levels after only eight weeks of consuming a diet low in saturated fat and cholesterol.27 The study participants also saw reductions in their LDL, total cholesterol, body weight, and arterial stiffness. So while you may soon see ads promoting the 37% C-reactive protein reduction in response to high-dose Crestor®, you should be aware that the same benefit has already been shown in response to healthier eating—with no drugs used. Another study shows that eating cholesterol-lowering food works about as well as consuming a very low-fat diet plus statin drug therapy. This study showed a 33.3% reduction in C-reactive protein and 30.9% reduction in LDL in subjects eating a very low-fat diet and taking a statin drug. Those who ate the cholesterol-lowering foods showed a 28.2% reduction in C-reactive protein and a 28.6% reduction in LDL.28 This study showed that eating cholesterol-lowering foods achieved almost the same benefit as those who followed a very low-fat diet and took a statin drug. The cholesterol-lowering foods used in this study include almonds, soy protein, fiber, and plant sterols.28 Few people can follow a rigorous low-fat diet and some people want to avoid statin drugs. Based on this study, those who need to reduce LDL and/or C-reactive protein blood levels can accomplish this by eating cholesterol-lowering foods or taking supplements such as soluble fiber powder before heavy meals. In a study of 3,920 people, subjects who ingested the most dietary fiber were found to have a 41% lower risk of elevated C-reactive protein levels, compared with those who ate the least fiber. The doctors who conducted this study concluded: “Our findings indicate that fiber intake is independently associated with serum CRP concentration and support the recommendation of a diet with a high fiber content.”29 There is an important take-home lesson here for those with high C-reactive protein levels that persist even after initiating statin drug therapy. You may be able to achieve significant additive benefits by making dietary modifications, taking at least 1,000 mg of vitamin C each day, and following other proven ways to quell chronic inflammatory reactions.
| |||||||||
Sex Hormones and Inflammation in MenAging men are plagued with declining testosterone levels while their estrogen remains the same or even increases. This imbalance often sets the stage for a host of chronic inflammatory disorders, while increasing the amount of abdominal adiposity. For years, we at Life Extension have advised maturing men to restore their free testosterone to youthful ranges (between 20 and 24 pg/mL of blood) and keep their estrogen from getting too high. Ideal estrogen (estradiol) levels in men have been shown to be between 20 and 30 pg/mL of blood.
We have seen countless cases of men with chronic inflammation experience a reversal of their elevated C-reactive protein (and painful symptoms) when a youthful sex hormone profile is properly restored. Independent published studies corroborate our findings that low testosterone and high estradiol predisposes aging men to chronic inflammatory status and higher C-reactive protein.30-32 Based on these findings, the overweight Crestor® study subjects could have benefited enormously if their sex hormone balance was restored to youthful ranges. It is tantalizing to think what benefits could have been shown if those who took Crestor® used these additive approaches to reduce their C-reactive protein to optimal levels. Simple Guidelines to Protect Yourself Against Heart Attack and Stroke
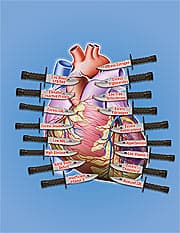
At the end of this article is a reprint of our 17 “daggers aimed at the heart” diagram that represents independent risk factors associated with heart attack and stroke. Any one of these daggers can create vascular disease. Regrettably, aging people often suffer multiple risk factors (daggers aimed at their heart) that cause them to die prematurely. Fortunately, the proper blood tests can identify risk factors unique to each individual so that corrective action can be taken before one’s heart or brain is decimated by a catastrophic vascular event. The third article in this month’s issue discusses the 17 independent risk factors involved in vascular disease and describes the simple steps you can take to make sure that none of them causes a problem for you. As you will readily see, there is a wide range of lifestyle, nutrient, hormone, and drug choices available. If you don’t want to take drugs, plenty of natural alternatives exist. Some people will need to take drugs, however, to get into optimal ranges.
Lethal Dangers of C-Reactive Protein ElevationMultiple studies document that a chronic inflammatory process is directly involved in the degenerative diseases of aging including cancer,89-91 dementia,92-94 stroke,95-97 visual disorders,98,99 arthritis,100-102 liver failure,103,104 and heart attack.4,105-109 Fortunately, a low-cost C-reactive protein blood test can identify whether you suffer a smoldering inflammatory fire within your body that will likely cause you to die prematurely. An abundance of scientific research provides a wide range of proven approaches to suppress chronic inflammatory reactions.33-78,110,111 The comprehensive Male and Female Blood Test Panels reveal what your C-reactive protein level is right now, along with other factors that could cause your C-reactive protein to be too high. Blood components that can spike C-reactive protein levels include high LDL,112 low HDL,113 low testosterone114 and excess estradiol (in men),115 elevated glucose,116,117 excess homocysteine,118 and DHEA deficit.119 Remember, optimal blood levels of C-reactive protein are below 0.55 mg/L in men and below 1.50 mg/L in women.12 Standard reference ranges accept higher levels as normal because so many people fail to take care of themselves and thus suffer chronically high C-reactive protein levels with subsequently increased risk of heart attack,6,120-123 stroke,6-8,124 cancer,89-91 senility,125,126 etc.127
No More Heart Attacks!The Crestor® study showed it is possible to achieve a dramatic reduction in heart attack and stroke incidence when C-reactive protein and LDL are reduced.
Yet the same study revealed that a significant number of study subjects who suffered “major cardiovascular events” were not protected by the high dose of Crestor® they took. This proves beyond any doubt that more than cholesterol, LDL, and C-reactive protein5,128-132 are involved in the atherosclerotic process that results in heart attack and stroke being today’s leading causes of disability and death. If one is to achieve ultimate protection against arterial disease, all of the independent risk factors (as identified in the 17 daggers aimed at the heart graphic) have to be brought under control. We should all be grateful to live in an era when these vascular risk factors can be easily measured and corrected before a major cardiovascular event manifests! Lowest Blood Test Prices of the YearOnce a year, Life Extension discounts the price of the popular Male or Female Blood Test Panels. The medical establishment charges around $1,000 for these comprehensive tests. To review the many longevity factors included in the Male or Female Blood Test Panels, and how you can use the findings from your blood test to protect against age-related disease, refer to How to Circumvent 17 Independent Heart Attack Risk Factors from this issue. When you place your blood test order, we send you a requisition form along with a listing of blood-drawing stations in your area. You can normally walk in during regular business hours for a convenient blood draw. For longer life,
William Faloon
| ||||||||||||||
| References | ||||||||||||||
|