Life Extension Magazine®

A lot of people ask how Life Extension® is able to be consistently ahead of the curve when it comes to identifying modifiable disease risk factors.
I initially found it hard to answer this since our recommendations are based on the identical peer-reviewed literature that is often published by the medical establishment itself.
The reply to this question I now give relates to motivation and interpretation.
We at Life Extension don’t want ill health to befall our supporters…ever! We therefore interpret statistical data with the motivation to thwart degenerative disease for an indefinite time period.
So it was not hard for us to notice long ago that people with lower blood pressure lived considerably longer. Our recommendation relating to blood pressure therefore has always been to keep readings below 120/80 mmHg, with an ideal number for most individuals being 115/75 mmHg.
The medical establishment disagreed and said that blood pressure up to 139/89 mmHg was not a problem. A huge study released in 2015 exposed the lethality of this position. In the group whose target goal systolic blood pressure was below 120 there was a:1
- 38% lower relative risk of heart failure;
- 43% lower relative risk of cardiovascular death;
- 27% lower relative risk of mortality overall.
This article will review the establishment’s multi-decade failure to recognize the dangers of higher blood pressure. More important, we will reveal how you can safely lower blood pressure to what most all parties now concur are optimal ranges.
Hypertension is the term used to define high blood pressure.
A simple dictionary definition of hypertension is “abnormally high blood pressure.”
A medical definition of hypertension is “blood pressure high enough that it may eventually cause health problems, such as heart disease.”2
The problem over the past 49 years is that the medical establishment has mostly relied on the dictionary definition to diagnose hypertension. Since most aging people have blood pressure over 120/80 mmHg, physicians viewed this as “normal” and did nothing until levels exceeded 139/89 mmHg.
To understand the magnitude of this, one of every three adults in the United States has blood pressure readings over 139/89 mmHg.3 When you include those with readings over 120/80 mmHg, it’s easy to see why so many people suffer disorders related to hypertension.
Stated simply, the vast majority of adults have blood pressure high enough to cause heart disease and other health issues.
How Life Extension Realized This So Early

The gold standard for identifying beneficial longevity factors has long been to look at biomarkers in people that practice calorie restriction.
Calorie restrictors don’t behave like most of us, especially when viewing the toxic high-calorie foods that are endlessly advertised on television. As a result of their reduced food intake, calorie restrictors’ glucose, insulin, and lipid blood levels are remarkably low. So is their blood pressure.
Without taking medications, calorie restrictors over age 50 often have blood pressure readings around 90/60 mmHg and they are in remarkably good health.
We at Life Extension recognized this phenomenon in the 1980s and recommended most people strive to maintain blood pressure readings below 120/80 mmHg to emulate this longevity benefit observed in people practicing calorie restriction.
New Study Wakes Up Medical Establishment!

A large human study was initiated in year 2010 whose purpose was to assess whether targeting a reduction of systolic blood pressure below 120 mmHg was superior to the current standard of reducing it to below 140 mmHg.
The doctors focused on the systolic (top) number because it is a better predictor of heart attack and stroke. The “systolic” reading reflects the amount of pressure placed on the arterial system with each heartbeat.
The name of this study is Systolic Blood Pressure Intervention Trial, also known as SPRINT.1 It was published in the New England Journal of Medicine in 2015 and garnered huge media coverage.
The SPRINT study was supposed to last 5 years, but was stopped after 3.26 years because it was abundantly clear that the group whose blood pressure was reduced to a target systolic range under 120 mmHg were dying 26% less frequently.
What impressed the study’s researchers the most was a striking 43% lower relative risk of cardiovascular death in those whose blood pressure was aggressively reduced.
The SPRINT study also found that heart failure rates plummeted by 38% in patients whose target blood pressure aimed below 120 mmHg. Heart failure occurs when the heart cannot pump enough blood and oxygen to support other organs in one’s body. It is a leading cause of hospitalizations and costs this nation an estimated $32 billion each year.4
Heart disease happens to be the number one cause of death in the United States, killing about 610,000 Americans each year.5 The dramatic (43%) drop in cardiovascular deaths shown in the SPRINT study motivated mainstream cardiologists to question their long-standing practice of largely ignoring their patient’s blood pressure until readings exceeded 139/89 mmHg.
Based on widespread media coverage and physician concurrence, it appears the medical establishment has finally woken up to what readers of this publication were told to do in the 1980s.
Historic Failures to Recognize Disease Causation
It is regrettable that practicing clinicians did not bother to observe that patients with blood pressure readings over 120/80 mmHg had elevated rates of cardiac death. But then again, it took decades of research to raise suspicion of a causative role of cigarette smoking in the development of lung cancer.
Physicians in the 1930s were certainly aware that respiratory illnesses happened with greater frequency in smokers. Yet it took decades of published research for the tobacco-disease causation issue to be raised, and it wasn’t until 1964 that the Surgeon General stated that smoking increases risk for a host of deadly illnesses.6
A similar scenario has occurred with the debate as to what the safe upper limit for blood pressure should be. Persuasive evidence and common sense long ago indicated that Life Extension’s recommendation of 115/75 mmHg would spare many lives compared to the establishment’s position that blood pressure readings up to 139/89 mmHg were alright.
Similar to Controversy about Glucose
You may recall that in the 1980s, fasting blood glucose levels up to 139 mg/dL were considered “normal” by the establishment. Conventional doctors today consider a glucose level over 125 mg/dL indicative of type II diabetes. A glucose level over 99 mg/dL can diagnose prediabetes.
Based on blood results obtained from calorie restrictors in the 1980s, we at Life Extension knew that conventional medicine’s upper limit for glucose was dangerously high. We advised back then that people strive to keep their glucose levels below 100 mg/dL. Since then, we advised that optimal fasting glucose levels are below 86 mg/dL, which is not always possible to attain.
Reducing blood pressure is simpler (than glucose) for most individuals to achieve using a combination of lifestyle changes, nutrients, and the appropriate antihypertensive medications when necessary.
How Many Preventable Deaths?
Each year about 2.5 million Americans die.7 This number is expected to steadily rise as the aging population increases. Life Extension’s fundamental mission is to reverse this upward mortality trend in aging humans.
We wanted to glean some idea as to how many needless deaths occurred because it took the medical establishment so long to recognize the lifesaving benefits of lower blood pressure ranges. So we took the most conservative percentage of death reduction found in the SPRINT study, which was a 27% reduction in overall mortality in people age 50 and older. We then did a calculation using the approximate 2 million total deaths that have occurred each year in the United States in people age 50 and older dating back to year 1985.
Based on this 27% reduction in all-cause mortality, about 540,000 American lives could have been spared each year had the medical establishment adopted Life Extension’s recommendation to keep blood pressure levels below 120/80 mmHg.
This number of 540,000 annual deaths that could have been prevented is of course an exaggeration. It assumes that everyone ages 50 and older would have had their blood pressure checked and followed an aggressive program to reduce it to safe ranges. The reality is that hypertension is a “silent killer” and many people don’t know they have it. Patients prescribed antihypertensive drugs and lifestyle changes often don’t comply.
There were nonetheless tens of millions of Americans treated for hypertension since 1985, with the physician’s goal being to reduce it only to under 140/90 mmHg. This is where the needless carnage arose and where mainstream medicine needs to look at this failure as an example of the cost in human lives that occurs when published studies and common sense are discarded.
Our Delicate Vasculature

The extremely fragile nature of our vascular system remains an unappreciated phenomenon.
In youth, our arteries are flexible and readily expand and contract with each heartbeat as do our delicate capillary beds. As you can see by the illustration on this page, arteries narrow into smaller arterioles that eventually thin further down to microscopic capillaries. These capillaries are so tiny that red blood cells often have to bend their shape just to squeeze through and be returned to the venous system.
With each heart beat there is blood pressure exerted on arteries, arterioles, and delicate capillary beds. When blood pressure is in a perfect range, oxygen/nutrient enriched blood is delivered to all the body’s cells and returned to the heart with minimal damage to the vascular system.
Any increase in the pressure beyond what is needed to push blood through the vascular network causes additional stress and endothelial damage. This can manifest acutely in the form of a cerebral hemorrhage, where an arteriole in the brain ruptures and may quickly lead to death.
In most cases of higher-than-needed blood pressure, however, silent damage is constantly inflicted on the inner arterial lining (the endothelium) including the delicate capillaries.8 The result is a progressive loss of blood flow and cellular functionality that can manifest as ischemic heart disease,9-11 ischemic stroke,12-14 renal failure,15,16 and/or dementia.17-21
It was this fundamental understanding of the delicate structure of the vascular system that prompted Life Extension to recommend lower blood pressure ranges in the 1980s.
Fallacy of “Prehypertension”

flowing through and then the focal narrowing that occurs in
response to elevating blood pressures.
Not all physicians have been oblivious to the increased vascular risks in people with higher systolic blood pressure.
The term “prehypertension” was introduced to alert people that systolic pressure between 120 and 139 mmHg was reason to initiate lifestyle changes or modest drug therapy.
The problem with using the term prehypertension is that it caused patients and physicians to not take seriously the dangers it represents.
A systematic review on the clinical relevance of prehypertension was published in 2013 and revealed more increases in vascular risk than the carefully controlled SPRINT study.
The authors of this 2013 review performed an analysis of 18 previous studies that included a whopping 468,561 patients. They found that patients with prehypertension had a:22
- 55% increased risk of cardiovascular disease,
- 50% increased risk of coronary heart disease,
- 71% increased stroke risk.
The authors went a step further and looked at people in the low prehypertension range, defined by systolic blood pressure of just 120 to 129 mmHg. Risk of cardiovascular disease in this prehypertension group was 46% higher than for individuals with systolic blood pressure levels below 120 mmHg.
According to this very large analysis, even lower-range prehypertension has a significant impact on morbidity and mortality, which is why Life Extension has urged for so long that optimal blood pressure readings are 115/75 mmHg.
Based on the totality of the evidence, the term “prehypertension” should be discarded and most adults with systolic blood pressure over 119 mmHg should face the reality that they are hypertensive from a medical definition standpoint, i.e., they are at an increased risk of health problems.
This is analogous to the term prediabetes, which is used today to describe people with fasting glucose between 100-125 mg/dL. These individuals should instead be diagnosed as “diabetic” and treated accordingly. This includes lifestyle modifications that safely reduce blood glucose levels to optimal ranges.
Please know that upper-level acceptable systolic blood pressure readings at one time were considered a startling high of 160 mmHg. They were later reduced to 150 mmHg, then to 140 mmHg, and mercifully now down to 120 mmHg.
Do Not Rush to Lower Blood Pressure

The SPRINT study was released in 2015 and is likely to be a game-changer as it relates to better guidelines for blood pressure control. There were, however, limitations that cause us to urge caution before initiating steps to drastically lower your blood pressure.
The SPRINT study was of relatively short duration and longer term side effects from the aggressive drug therapies may not be fully understood.
Type II diabetics were excluded from SPRINT because a previous trial on diabetics called ACCORD failed to show a benefit in aggressively reducing their blood pressure.23 This failure may reflect the devastating impact on the vascular system inflicted by the elevated glucose levels seen in diabetics. Said differently, the severity of the endothelial damage that diabetics sustain might overwhelm the beneficial effects of aggressively lowering their systolic blood pressure.
Those who have had chronic higher blood pressure levels often suffer considerable damage to their delicate endothelial linings.8,24 An unfortunate consequence for some individuals is that they need to maintain somewhat higher blood pressure levels to provide adequate blood flow to the capillaries in their brain, kidneys and other tissues.
We have discussed this problem in previous issues of this publication, whereby those with severely damaged capillary beds require higher blood pressure to sustain organ/tissue function, even though over the longer term this higher pressure on the arterial system inflicts additional damage to the endothelium.25
The sad case for some individuals is that taking overly aggressive steps to push down blood pressure levels could create side effects such as hypotension, which causes one to faint.
A more serious effect observed in the SPRINT study was that there was almost a 3.5-fold increased risk of kidney damage in those aggressively treated for hypertension using multiple drugs. It is not known if it was the multiple drugs or overly aggressive lowering of the blood pressure that caused this kidney damage.
The authors of the SPRINT study were quick to point out that the huge reductions in morbidity and mortality in the aggressively-treated hypertensive group far outweighed the side effect risks observed. As one outside doctor who critiqued the study stated, “If there is a problem with an individual patient, you can always back off.”26
Our Precious Endothelium
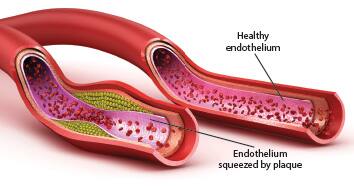 |
Our inner arterial lining is called the endothelium.
The endothelium is an ultra-thin, one-cell-thick layer of cells. It loses youthful function in response to normal aging.
An underappreciated factor in the development of cardiovascular disease is endothelial dysfunction. The consequences of endothelial dysfunction are diminished circulation, high blood pressure, thrombosis, and atherosclerosis, all of which are major causes of stroke and heart attack.27-31
Fortunately, astute scientists have discovered potent natural methods to tackle the underlying causes of endothelial dysfunction.
In addition to nutritional/lifestyle interventions, maintaining optimal blood pressure readings is essential to protect against loss of endothelial function.
Providing You with Real World Guidance
The encouraging news about all this is that if one intelligently embarks on a program to reduce their blood pressure to more optimal ranges, there are simple blood tests available that can identify if adverse effects are occurring in response to overly aggressive drug treatment.
These and other commonsense approaches to achieving optimal blood pressure levels are described in articles contained in this month’s issue. Readers should understand that the more one is willing to make healthier lifestyle changes, the less in the way of antihypertensive drugs they are likely to need, which should translate into a lower side effect risk profile.
We published an article 1.7 years ago that describes the ideal antihypertensive drug to begin with. This drug (telmisartan) not only lowers blood pressure in what we consider the most efficient manner, but has side benefits that include improvements in endothelial function and survival not seen with other antihypertensive medications.
Majority of Adults Are Hypertensive and Prevalence Increases as We Age!
 |
Most of you reading this article have higher-than-optimal blood pressure, or are effectively treating it.
Whether you treat it successfully or not, you are still classified as a hypertensive patient, just as one with high blood sugar is still a diabetic even though they may take enough medication to bring glucose down to a normal level.
The following chart reveals the huge percentage of noninstitutionalized persons with hypertension (defined as having measured high blood pressure and/or taking antihypertensive medication) between the years 2011-2014.32
Men | 65-74 years |
63.4% |
75 years and over | 72.3% | |
Women | 65-74 years | 64.3% |
75 years and over | 79.9% |
These data clearly show hypertension increasing with age, which makes taking control of one’s blood pressure so critical if one is to avoid the most common causes of death and disability.
Challenges in Persuading Our Supporters
I’ve been involved in helping people avoid degenerative illness since the 1970s.
One of my greatest challenges has been to persuade health-conscious individuals that they may need a prescription medication to optimize their blood pressure.
An argument I’ve encountered from people who eat properly, exercise, and take dietary supplements is that they don’t think they have to worry about slightly elevated blood pressure. While all these healthy practices can help protect against endothelial dysfunction, one cannot overlook the structural damage inflicted to our vasculature by higher-than-optimal blood pressure.
I also have run into resistance by people who think a blood pressure check several times a year at their doctor’s office is sufficient.
Based on my personal experience with my at-home blood pressure monitor, I know that my systolic pressure can range from a low of 95 mmHg to a high of 140 mmHg under stressful circumstances. When I see my blood pressure any level above 115/75 mmHg, I take an extra 40 mg dose of the drug telmisartan to reduce it. If I did not have an at-home blood pressure monitor, I would never have known my blood pressure spiked this high.
To make matters worse, your endothelium does not give you credit for the period of the day when your blood pressure is lower. It is during periods when blood pressure spikes up that massive vascular damage occurs. So I hope every one of you has an at-home blood pressure monitor based on our previous recommendations. As you can see on page 14, the price has come down considerably from what they cost just a few years ago.
To learn more about the blood pressure lowering drugs we favor, you can log on at no cost to: LifeExtension.comhttps://www.lifeextension.com/magazine/2018/3/hypertension2 These drug recommendations are not based on commercial interests, just our sincere desire to keep you alive and healthy for decades to come.
For longer life,
William Faloon
References
- Sprint Research Group, Wright JT, Jr., Williamson JD, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373(22):2103-16.
- Available at: http://www.mayoclinic.org/diseases-conditions/high-blood-pressure/basics/definition/con-20019580. Accessed August 22, 2016.
- Available at: http://www.cdc.gov/bloodpressure/facts.htm. Accessed June 14, 2016.
- Huynh-Hohnbaum AL, Marshall L, Villa VM, et al. Self-Management of Heart Disease in Older Adults. Home Health Care Serv Q. 2015;34(3-4):159-72.
- Available at: http://www.cdc.gov/heartdisease/facts.htm. Accessed August 22, 2016.
- Available at: https://profiles.nlm.nih.gov/NN/B/B/M/Q/. Accessed November 28, 2015.
- Available at: http://www.cdc.gov/nchs/fastats/deaths.htm. Accessed August 22, 2016.
- Dharmashankar K, Widlansky ME. Vascular endothelial function and hypertension: insights and directions. Curr Hypertens Rep. 2010;12(6):448-55.
- Rosendorff C, Black HR, Cannon CP, et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115(21):2761-88.
- Mukherjee D, Campbell CL. Optimal management of hypertension in patients with ischemic heart disease. Cardiovasc Hematol Agents Med Chem. 2009;7(3):198-205.
- Agbor-Etang BB, Setaro JF. Management of Hypertension in Patients with Ischemic Heart Disease. Curr Cardiol Rep. 2015;17(12):119.
- Johansson BB. Hypertension mechanisms causing stroke. Clin Exp Pharmacol Physiol. 1999;26(7):563-5.
- Chalmers J, Todd A, Chapman N, et al. International Society of Hypertension (ISH): statement on blood pressure lowering and stroke prevention. J Hypertens. 2003;21(4):651-63.
- Available at: http://www.medscape.com/viewarticle/473113. Accessed August 23, 2016.
- Bidani AK, Griffin KA. Long-term renal consequences of hypertension for normal and diseased kidneys. Curr Opin Nephrol Hypertens. 2002;11(1):73-80.
- Whitworth JA. Progression of renal failure -- the role of hypertension. Ann Acad Med Singapore. 2005;34(1):8-15.
- Faraco G, Iadecola C. Hypertension: a harbinger of stroke and dementia. Hypertension. 2013;62(5):810-7.
- Joas E, Backman K, Gustafson D, et al. Blood pressure trajectories from midlife to late life in relation to dementia in women followed for 37 years. Hypertension. 2012;59(4):796-801.
- Skoog I, Lernfelt B, Landahl S, et al. 15-year longitudinal study of blood pressure and dementia. Lancet. 1996;347(9009):1141-5.
- Shah NS, Vidal JS, Masaki K, et al. Midlife blood pressure, plasma beta-amyloid, and the risk for Alzheimer disease: the Honolulu Asia Aging Study. Hypertension. 2012;59(4):780-6.
- Ninomiya T, Ohara T, Hirakawa Y, et al. Midlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011;58(1):22-8.
- Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:177.
- Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575-85.
- Hausberg M, Lang D, Barenbrock M, et al. Large artery wall properties -- what is relevant for the classic management of hypertension?. Dtsch Med Wochenschr. 2005;130(46):2657-61.
- Available at: http://www.lifeextension.com/magazine/2015/3/best-drug-to-treat-hypertension/page-01. Accessed August 23, 2016.
- Available at: http://www.reuters.com/article/us-health-heart-bloodpressure-idUSKCN0SY2F920151109. Accessed August 23, 2016.
- Fordjour PA, Wang Y, Shi Y, et al. Possible mechanisms of C-reactive protein mediated acute myocardial infarction. Eur J Pharmacol. 2015;760:72-80.
- Eelen G, de Zeeuw P, Simons M, et al. Endothelial cell metabolism in normal and diseased vasculature. Circ Res. 2015;116(7):1231-44.
- Huveneers S, Daemen MJ, Hordijk PL. Between Rho(k) and a hard place: the relation between vessel wall stiffness, endothelial contractility, and cardiovascular disease. Circ Res. 2015;116(5):895-908.
- Seals DR, Jablonski KL, Donato AJ. Aging and vascular endothelial function in humans. Clin Sci (Lond). 2011;120(9):357-75.
- Pearson JD. Endothelial cell function and thrombosis. Baillieres Best Pract Res Clin Haematol. 1999;12(3):329-41.
- Available at: http://www.cdc.gov/nchs/fastats/older-american-health.htm. Accessed August 23, 2016.

